Chapter: Paediatrics: Special senses
Paediatrics: Back of the eye problems
Back of the eye problems
Endophthalmitis
Infection within the eye may be endogenous (spread of bacterial or
fungal infection from the bloodstream) or exogenous
(s to trauma or surgery). Symptoms
may vary in severity, but include achy pain, photophobia, float-ers, and loss
of vision, the eye is usually red and a pus level within the an-terior chamber
(hypopyon) may be seen. Endophthalmitis requires emer-gency ophthalmic referral
and management with systemic and intra-vitreal agents to prevent blindness.
Retinopathy of prematurity
This is a fibrovascular
proliferative retinal disorder occurring in preterm and low birth weight
infants. Its development has been associated with high concentrations of
inspired oxygen during the neonatal period. Normal retinal vascularization is
not complete until full term. In preterm infants this process is interrupted
and, on restart-ing, may proceed abnormally with aberrant and proliferative new
vessel formation.
ROP screening
Infants born
<31wks gestation, or weighing <1500g are screened from 6wks of age until the retina has vascularized.
Treatment
Indirect laser therapy is used in
severe cases.
Other medical conditions causing retinopathy
Sickle cell disease
The deformed RBCs in sickle cell
disease may cause retinal vascular occlu-sion or ischaemia. A proliferative
retinopathy with new vessel formation, or a non-proliferative retinopathy with
scarring and fibrosis may develop. Screening is required with laser
photocoagulation for new vessel forma-tion.
Diabetes mellitus
Diabetic retinopathy is rarely
seen in children with type 1 diabetes and not usually before onset of puberty
and teenage years.
Retinitis pigmentosa (RP)
This progressive degenerative
disorder of the retina is characterized by typical pigmented retinal
appearances. It is an important cause of night blindness, reduced central and
peripheral vision, and cataracts. It may occur as an isolated finding or may be
part of a systemic disorder.
•
Usher’s syndrome: RP + congenital deafness.
•
Bassen–Kornweig syndrome: RP + abetalipoproteinaemia,
ataxia, and malabsorption.
•
Refsum’s disease: RP + polyneuropathy, deafness, and
cerebellar dysfunction.
Kearns–Sayre
syndrome: RP +
ophthalmoplegia, cardiac conduction defect.
Retinal dystrophies
A group of inherited disorders
causing rod, cone and/or inner retinal cell dysfunction. Early onset retinal
dystrophy may cause blindness in infancy, other forms can cause progressive
visual loss during childhood.
Rod dystrophies primarily reduce
night and peripheral vision. Cone dystrophies primarily reduce colour vision,
central vision, and cause pho-tophobia. Most children are otherwise healthy,
but retinal dystrophy can be part of a widespread disorder, e.g. Bardet–Biedl
syndrome, Cockayne syndrome, Batten disease, and peroxisomal disorders.
Children with early onset SN hearing loss should be referred in order to
exclude Usher syn-drome. Supportive help with optical and educational aids has
been the mainstay of management in the past, but recent success with gene
therapy gives us some optimism for future treatment.
Papilloedema/optic disc swelling
There are many causes of optic
disc swelling and the term papilloedema
is reserved for optic disc swelling secondary to raised ICP. Visual acuity is
usually good initially, but symptoms such as visual obscurations (momen-tary
loss of vision when leaning over or coughing) and diplopia secondary to
bilateral sixth nerve paresis may occur. If left untreated, the
papilloe-dematous nerve will start to become atrophic, initially causing visual
field constriction and eventually loss of central and colour vision.
Optic
disc drusen are
calcific deposits in the optic nerve head that can mimic optic disc swelling. Drusen ‘light up’ on ultrasonography
(performed by an ophthalmologist) and this non-invasive test can prevent
unnecessary neurological investigation.
Optic neuritis/neuropathy
Inflammation, infiltration, or
compression of the optic nerve cause ear-ly loss of central and colour vision.
Assessment of optic nerve function should include:
•
Visual
acuity.
•
Visual
fields to confrontation (or perimetry if able).
•
Colour
vision (ask child to compare brightness of red target in one eye to the other).
•
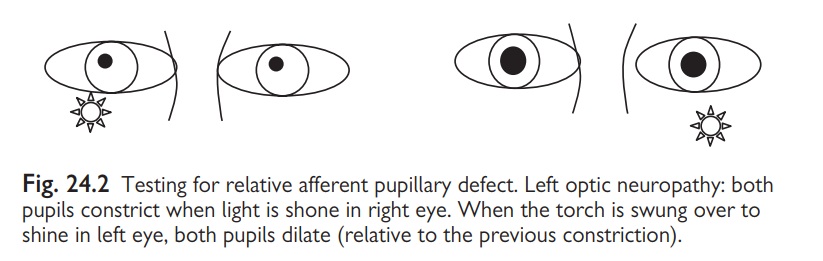
Pupil
reactions look for a relative afferent papillary defect (Fig. 24.2).
• Visualize the optic disc— it may be swollen or atrophic.
Related Topics