Chapter: Ophthalmology: Orbital Cavity
Orbital Involvement in Autoimmune Disorders: Graves Disease
Orbital Involvement in Autoimmune Disorders: Graves’ Disease
Definition
Autoimmune disorder with orbital involvement
frequently associated with thy-roid dysfunction. Histologic examination reveals
inflammatory infiltration of the orbital cavity.
Epidemiology:
Women are affected eight times as often as men. Sixty percent of
all patients have hyperthyroidism. Ten per cent of patients with thy-roid
disorders develop Graves’ disease during the course of their life.
Graves’ disease is the most frequent cause of
both unilateral and bilateral exophthalmos.
Etiology:
The precise etiology of this autoimmune disorder is not clear.
Histo-logic examination reveals lymphocytic infiltration of the orbital cavity.
The ocular muscles are particularly severely affected. Fibrosis develops after
the acute phase.
An autonomous adenoma of the thyroid gland is
not associated with Graves’ disease. Some patients with Graves’ disease never
exhibit any thyroid dysfunction during their entire life.
Symptoms:
The onset of this generally painless disorder is usually
betweenthe ages of 20 and 45. Patients complain of reddened dry eyes with a
sensa-tion of pressure (symptoms of keratoconjunctivitis sicca) and of cosmetic
problems. Ocular motility is also limited, and patients may experience double
vision.
Diagnostic considerations:
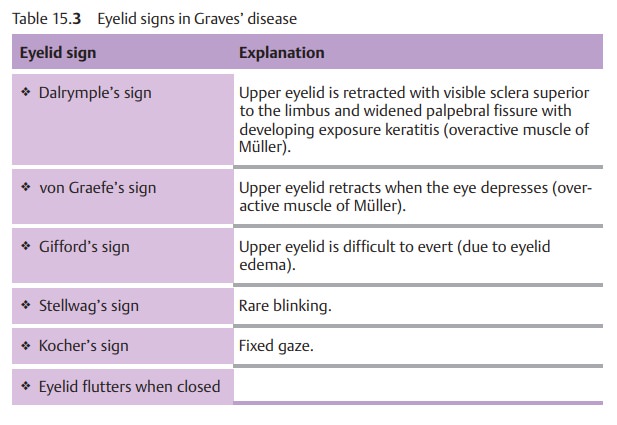
Cardinal symptoms includeexophthalmos,which is unilateral in only 10% of all cases, and eyelid changes that involve development of a characteristic eyelid sign (Table 15.3 and Fig. 15.3). Thicken-ing of the muscles (primarily the rectus inferior and medialis) and sub-sequent fibrosis lead to limited motility and double vision. Elevation is impaired; this can lead to false high values when measuring intraocularpressure with the gaze elevated.
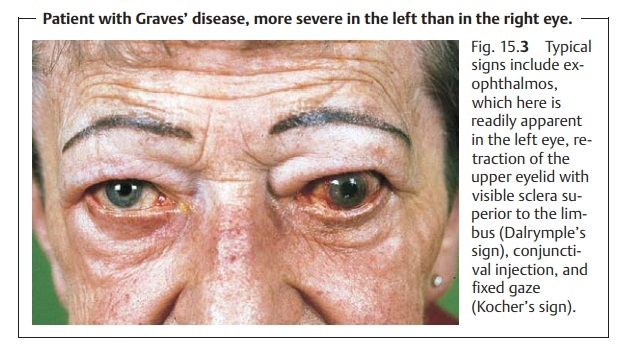
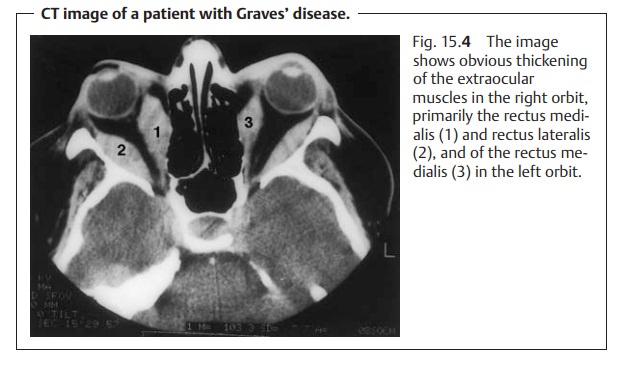
The tentative clinical diagnosis of Graves’ disease is supported by thicken-ing of the extraocular muscles identified in ultrasound or CT studies (Fig. 15.4). The further diagnostic work-up requires the cooperation of an internist, endocrinologist, and radiologist.
Differential diagnosis:
Rarer clinical syndromes such as orbital tumors andorbital
pseudotumors must be excluded.
Treatment:
The main principles in treating the disease in itsacute stageinclude management of the thyroid dysfunction, systemic cortisone (initially 60 – 100 mg of prednisone) and radiation therapy of the orbital cavity.
Surgicaldecompression of the orbital
cavity is indicated inrecurrent
cases that do notrespond to treatment to avoid compressive optic
neuropathy. Exposure ker-atitis (keratitis
due to inability to close the eye) should be treated withartifi-cial tears or
tarsorrhaphy (partial or complete suture closure of the upper andlower
eyelid to shorten or close the palpebral fissure). In the postinflam-matory stage of the disease,eye muscle surgerymay be performed to correctstrabismus.
Clinical course and prognosis:
Visual acuity will remain good if treatment isinitiated promptly.
In the postinflammatory phase, exophthalmos often per-sists despite the fact
that the underlying disorder is well controlled.
Related Topics