Chapter: Ophthalmology: Orbital Cavity
Orbital Cavity: Examination Methods
Examination Methods
Cardinal symptoms:
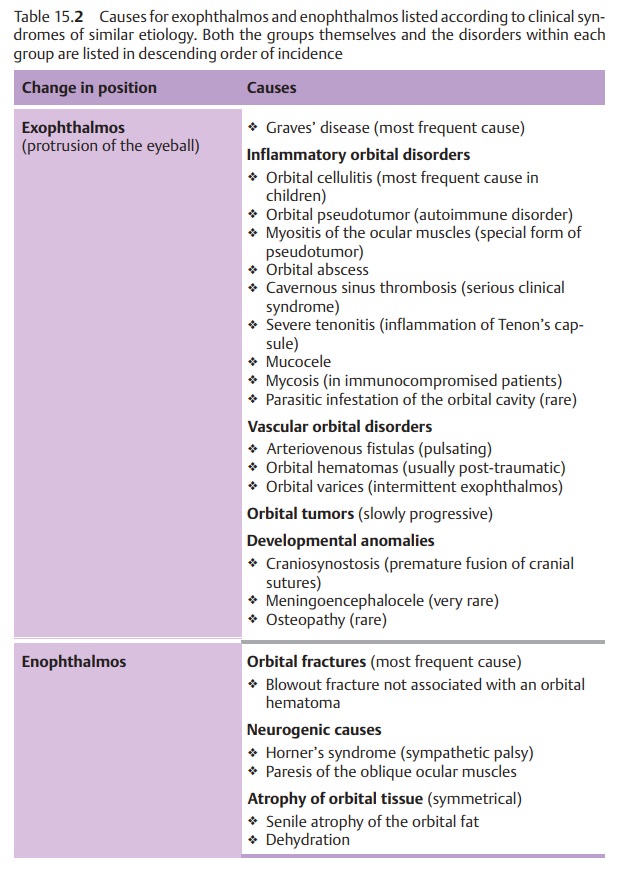
Unilateral or bilateralenophthalmos(recession
of theeyeball within the orbital cavity) or exophthalmos (protrusion of the eyeball) are characteristic of many
orbital disorders (Table 15.2).
These conditions should be distinguished from pseudoexophthalmos due to a long eyeball in severe myopia, and pseudoenophthalmos due to a small
eyeball, such as in microphthalmos or phthisis bulbi.
The following list of examination techniques
begins with the simple stan-dard techniques and progresses to the difficult,
more elaborate methods. As a general rule, orbital disorders require
interdisciplinary cooperation between ENT specialists, neurologists, neurosurgeons,
neuroradiologists, internists, nuclear medicine specialists, and oncologists.
Visual acuity:.
Visual acuity, the sharpness of
near and distance vision, is tested separately for each eye. One eye is covered
with a piece of paper or the palm of the hand placed lightly over the eye. The
fingers should not be used to cover the eye because the patient will be able to
see between them (Fig. 1.4).
The general practitioner or student can perform an approximate test of visual acuity. The patient is first
asked to identify certain visual symbols
referred to as optotypes (see Fig. 1.2)
at a distance of 5 meters or 20 feet (test
of distance vision). These visual
symbols are designed so that optotypes of a cer-tain size can barely be
resolved by the normal eye at a specified distance (this standard distance is
specified in meters next to the respective symbol). The eye charts must be
clean and well illuminated for the examination. The sharpness of vision
measured is expressed as a fraction:
Normal visual acuity is 5/5 (20/20), or 1.0 as a
decimal number, where the actual
distance equals the standard distance.
An
example of diminished visual acuity
(see Fig. 1.2): The patient sees
only the “4” and none of the smaller symbols on the left eye chart at a
distance of 5 meters (20 feet) (actual distance). A normal-sighted person would
be able to discern the “4” at a distance of 50 meters or 200 feet (standard
distance). Accordingly, the patient has a visual acuity of 5/50 (20/200) or
0.1.
The
ophthalmologist tests visual acuity
after determining objective refraction using the integral lens system of a
Phoroptor, or a box of individual lenses and an image projector that projects
the visual symbols at a defined distance in front of the eye. Visual acuity is
automatically calculated from the fixed actual distance and is displayed as a
decimal value. Plus lenses (convex
lenses) are used for farsightedness
(hyperopia or hypermetropia), minus lenses (concave lenses) for nearsightedness (myopia), and cylindrical lenses for astigmatism.
If the patient cannot discern the symbols on the eye chart at a distance of 5 meters (20 feet), the examiner shows the patient the chart at a distance of 1 meter or 3 feet (both the ophthalmologist and the general practitioner use eye charts for this examination). If the patient is still unable to discern any symbols, the examiner has the patient count fingers, discern the direction of hand motion, and discern the direction of a point light source.
Ocular motility:
The pattern of disturbed ocular motility can be asign of thecause of the disorder.
Causes may be neurogenic, myogenic, or mechanical.
Examination of the fundus:
Retrobulbar processes can press the globeinward. This often
produces choroidal folds that are
visible upon ophthal-moscopy. Compression of the optic nerve by a tumor may
result in optic nerve atrophy or edema.
Meningiomas in the sheath of the optic nerve leadto the development of shunt vessels on the optic disk.
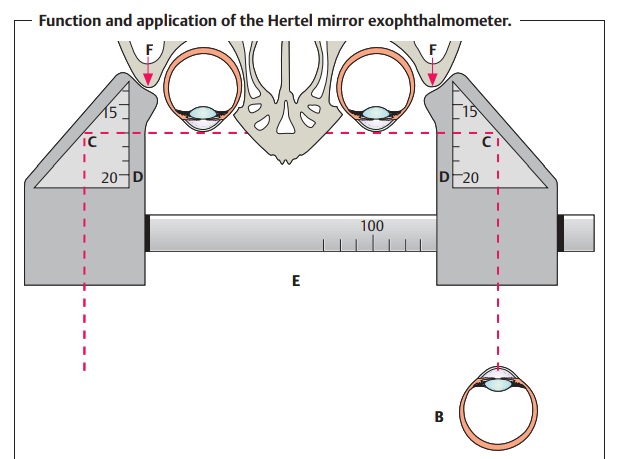
Exophthalmometry:
TheHertel mirror exophthalmometer(Figs. 15.2aandb)measures the anterior projection of the globe beyond the orbital rim. A change in the position of the globe with respect to the orbital rim is a cardi-nal symptom of many orbital disorders (see Table 15.2).
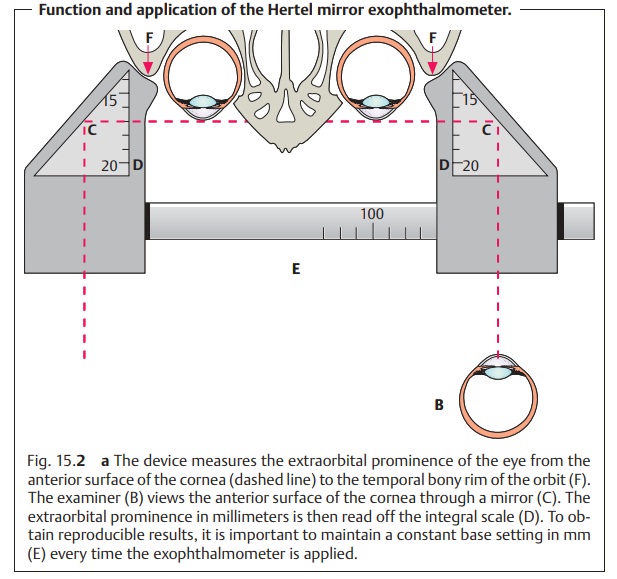
The difference between the two sides is more
important than the abso-lute value. A difference greater than 3 mm between the
two eyes is abnormal. Unilateral exophthalmos is recognizable without an
exoph-thalmometer. To do so, the examiner stands behind the patient, slightly
lifts the patient’s
upper eyelids, and looks down over the patient’s fore-head toward the cheek.
Visual field testing:
This is used to document damage to the optic nerve in orbital
disorders.
Ultrasound studies:
Two techniques are available for
this noninvasive examination.
The B-mode scan (B stands for brightness)
provides a two-dimensional image of orbital structures. This
examination is indicated in the presence of
suspected orbital masses.
The A-mode scan (A
stands for amplitude) permits precise measurement of optic nerve and muscle thickness. This
examination is indicated as a follow-up study in the presence of Graves’
disease (endocrine orbitopathy).
These studies may also be combined
with Doppler scans to evaluate blood
flow.
Conventional radiographic studies:
These studies usually only provide information
about the nature of bone structures,
i.e., whether a fracture is present and where it is located. Smaller fractures
often cannot be diagnosed by conventional radiography and require CT scans.
Computed tomography and magnetic resonance imaging:
These modern examination
modalities can precisely visualize orbital structures in various planes. They
are standard methods for diagnosing
tumors.
Angiography:
This is indicated in the presence of suspected arteriovenous fistulas.
Related Topics