Chapter: Ophthalmology: Orbital Cavity
Orbital Cellulitis
Orbital Inflammation
Because of the close proximity of the orbital
cavity to the paranasal sinuses, which are particularly susceptible to
inflammation, orbital inflammation represents the second most frequent group of orbital disorders after Graves’
disease. Orbital cellulitis is the most
severe of these.
Orbital Cellulitis
Definition
Acute inflammation of the contents of the orbital
cavity with the cardinal symptoms of limited motility and general malaise.
Orbital cellulitis is the most frequent cause
of exophthalmos in children.
Etiology:
Acute orbital inflammation posterior to the orbital septum isusu-ally an inflammation that has spread
from surrounding tissue. Over 60% of allcases (as high as 84% in children) may
be classified as originating in the sinuses,
especially the ethmoidal air cells and the frontal sinus. In infants, tooth germ inflammations may be the
cause.Less frequently, this clinical
pic-ture occurs in association with facial furuncles, erysipelas, hordeolum,
panophthalmitis, orbital injuries, and sepsis.
Symptoms:
Patients report severe malaise, occasionally accompanied byfever
and pain exacerbated by eye movement.
Diagnostic considerations:
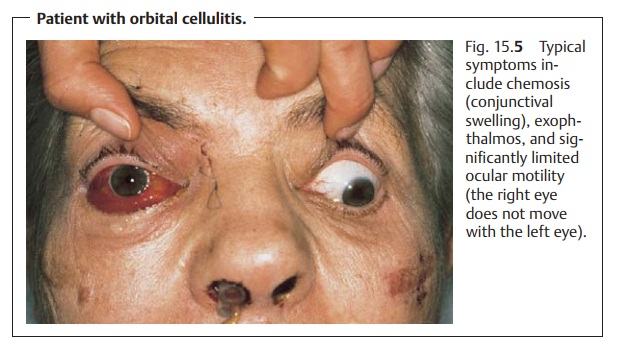
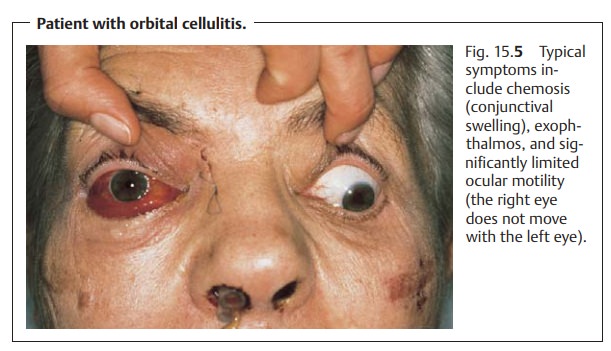
Typical symptoms includeexophthalmoswithsevere chemosis (conjunctival swelling), eyelid swelling, and significantly limited ocular motility (“cemented” globe; see Fig. 15.5). Patients mayexhibit leukocytosis and an increased erythrocyte sedimentation rate. Where there is clinical evidence of suspected involvement of the paranasal sinuses, an ENT specialist should be consulted to evaluate the sinuses and initiate any necessary treatment.
Differential diagnosis:
Preseptal cellulitis, which ismore
frequently encoun-tered, should be excluded. The inflammation in preseptal
cellulitis is anteriorto the orbital septum; chemosis and limited motility
are absent. Rarer clinicalsyndromes that
should also be considered in a differential diagnosis includean orbital pseudotumor, orbital periostitis which may be
accompanied by a subperiosteal abscess, and an orbital abscess.
The crucial characteristic feature of orbital
cellulitis for differential diag-nosis is the significantly limited ocular
motility (“cemented” globe). A rhabdomyosarcoma should also be considered in
children.
Treatment:
This consists ofhigh-dose
intravenous antibiotic therapywith1.5 g of oxacillin every four hours
combined with one million units of penicil-lin G every four hours. Infants are
treated with ceftriaxone and school-age children with oxacillin combined with
cefuroxime in the appropriate doses. Treatment
of underlying sinusitis is indicated in applicable cases.
Clinical course and complications:
Orbital inflammation can lead toopticneuritis with subsequent atrophy and loss of vision. Purulent
thrombophle-bitis of the orbital veins can result in cavernous sinus thrombosis
with menin-gitis, cerebral abscess, or sepsis.
Orbital cellulitis can progress to a
life-threatening situation (cavernous sinus thrombosis).
Related Topics