Chapter: Pharmaceutical Biotechnology: Fundamentals and Applications : Monoclonal Antibodies in Solid Organ Transplantation
Monoclonal Antibodies Administered at the Time of Transplant
Monoclonal
Antibodies Administered at the Time of Transplant
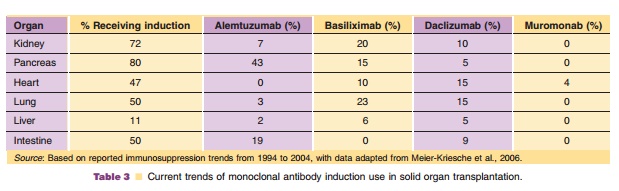
Current
maintenance immunosuppression is aimed at various targets within the immune
system to halt propagation of signal transduction pathway. Available agents,
although effective, are associated with sig-nificant patient and allograft
adverse effects which are associated with long-term exposure (Table 3). The
leading cause of death in non-cardiac transplant recipients is a cardiovascular
event. These cardiovas-cular events have been linked to long-term
corticos-teroid exposure. In addition, chronic administration of calcineurin
inhibitors (cyclosporine and tacrolimus) is also associated with acute and
chronic kidney dysfunction leading to hemodialysis or need for a kidney
transplant. Monoclonal antibodies given at the time of transplant (induction)
have been used to decrease the need for corticosteroids and allow for the delay
or a reduction in the amount of calcineurin inhibitor used. Determination of the
solid organ transplant recipient’s immunologic risk at the time of transplant
is necessary to determine which mono-clonal antibody to use in order to
minimize the risk of early acute rejection and graft loss. Recipients are
stratified based on several donor, allograft and recipient variables to
determine their immunologic risk. Patients at high risk for acute rejection or
those in
which maintenance immunosuppression is going to be minimized should
receive a polyclonal or mono-clonal antibody that provides cellular apoptosis,
for example alemtuzumab or rabbit-antithymocyte glo-bulin. Recipients at low
risk for acute rejection may receive a monoclonal antibody which provides
im-munomodulation without lymphocyte depletion, such as basiliximab or
daclizumab.
Several important pharmacokinetic parameters must be considered when
these agents are adminis-tered to the various organ transplant recipients. The
volume of distribution, biological half-life and total body clearance can
differ significantly from a kidney transplant recipient to a heart transplant
recipient. Clinicians must consider when to administer mono-clonal antibodies
in different transplant populations to maximize efficacy and minimize toxicity.
For example, heart and liver transplant recipients tend to lose large volumes
of blood around the time of transplant, therefore intraoperative administration
may not be the optimal time to administer a monoclonal antibody since a large
portion may be lost during surgery. Monoclonal antibodies are also removed by
plasma exchange procedures, such as plasmapheresis, which may be performed
during the perioperative period (Nojima et al., 2005).
Related Topics