Chapter: Obstetrics and Gynecology: Postpartum Care
Management of the Immediate Postpartum Period
MANAGEMENT OF THE IMMEDIATE POSTPARTUM PERIOD
Hospital Stay
In the
absence of complications, the postpartum hospital stay ranges from 48 hours
after a vaginal
delivery to 96 hours after a cesarean delivery, excluding day of delivery. Shortened
hos-pital stays are appropriate when certain criteria are met to ensure the
health of the mother and baby, such as the ab-sence of fever in the mother;
normal pulse and respiration rates and blood pressure level; lochia amount and
color appropriate for the duration of recovery; absence of any abnormal
physical, laboratory, or emotional findings; and ability of the mother to
perform activities such as walking, eating, drinking, self-care, and care for
the newborn. In addition, the mother should have adequate support in the first
few days following discharge and should receive in-structions about postpartum
activity, exercise, and com-mon postpartum discomforts and relief measures.
During
the hospital stay, the focus should be on preparation of the mother for newborn
care, infant feeding including the spe-cial issues involved with breastfeeding,
and required newborn laboratory testing. When
patients are discharged early, ahome visit or follow-up telephone call by a
healthcare provider within 48 hours of discharge is encouraged.
Maternal–Infant Bonding
Shortly after delivery, the
parents become totally engrossed in the events surrounding the newborn infant.
The mother should have close contact with her infant. Obstetric units should be
organized to facilitate these interactions by min-imizing unnecessary medical
interventions while increas-ing participation by the father and other family
members. Nursing staff can observe the interactions between the in-fant and the
new parents and intervene when necessary.
Postpartum Complications
Infection occurs in approximately
5% of patients and sig-nificant immediate postpartum
hemorrhage occurs in approximately 1% of patients. Immediately after the
delivery of the pla-centa, the uterus is palpated bimanually to ascertain that
it is firm. Uterine palpation through the abdominal wall is repeated at
frequent intervals during the immediate post-partum period to prevent and/or
identify uterine atony. Perineal pads are applied, and the amount of blood on
these pads as well as the patient’s pulse and pressure are monitored closely
for the first several hours after delivery to detect excessive blood loss.
Some patients will experience an
episode of increased vaginal bleeding between days 8 and 14 postpartum, most
likely associated with the separation and passage of the placental eschar. This
is self-limited and needs no therapy other than reassurance. Bleeding that
persists or is excessive is called delayed
postpartum hemorrhage, and it occurs in approximately 1% of cases.
Treatment includes oxytocic therapy or suction evacuation of the uterus.
Suction is suc-cessful in most cases, whether or not there is retained
pla-cental tissue, as is found in one-third of cases.
Analgesia
After vaginal delivery, analgesic
medication (including topical lidocaine cream) may be necessary to relieve
per-ineal and episiotomy pain and facilitate maternal mobility. This is best
addressed by administering the drug on an as-needed basis according to
postpartum orders. Most mothers experience considerable pain in the first 24
hours after cesarean delivery. Analgesic techniques
include spinalor epidural opiates, patient-controlled epidural or intravenous
analgesia, and potent oral analgesics.
Regardless
of the route of administration, opioids can cause respiratory depression and
decrease intestinal motility.
Adequate supervision and
monitoring should be ensured for all postpartum patients receiving these drugs.
Ambulation
Postpartum
patients should be encouraged to begin ambulation as soon as possible after
delivery. They should be offered as
Early ambulation helps
avoid urinary retention and prevents puerperal venous thromboses and pulmonary
emboli.
Breast Care
Breast
engorgement in women who are not breastfeed-ing occurs in the
first few days postpartum and gradually abates over this period. If the breasts
become painful, they should be supported with a well-fitting brassiere. Ice
packs and analgesics may also help relieve discomfort. Women who do not wish to
breastfeed should be encouraged to avoid nipple stimulation and should be
cautioned against continued manual expression of milk.
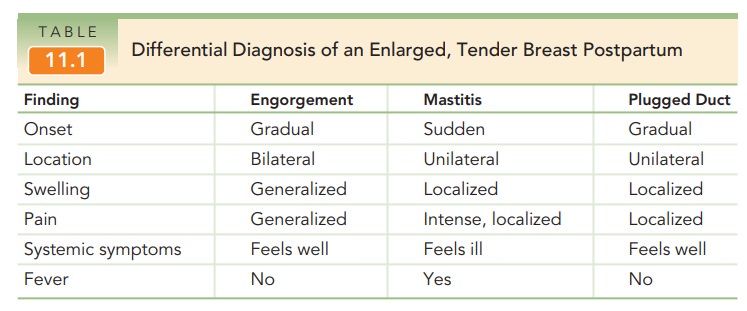
A plugged duct (galactocele) and mastitis may also
re-sult in an enlarged, tender breast postpartum (Table 11.1). Mastitis, or infection of the breast
tissue, most often occursin lactating women and is characterized by
sudden-onset fever and localized pain and swelling. Mastitis is associ-ated
with infection by Staphylococcus aureus,
Group A or B streptococci, βHaemophilus species,
and Escherichiacoli. Treatment
includes continuation of breastfeeding oremptying the breast with a breast pump
and the use of ap-propriate antibiotics. Breast milk remains safe for the
full-term, healthy infant.
Symptoms of a breast abscess are similar to those of mastitis, but a fluctuant mass is also present. Persistent fever after starting antibiotic therapy for mastitis may also suggest an abscess. Treatment requires surgical drainage of the abscess in addition to antibiotic therapy.
Immunizations
Women who do not have antirubella
antibody should be immunized for rubella
during the immediate postpartum period. Breastfeeding is not a contraindication
to this immunization. If a patient has not already received the tetanus-diphtheria acellular pertussis
vaccine, and if ithas been at least 2 years since her last
tetanus-diphtheria booster, she should be given a dose before hospital
dis-charge. If the woman is D-negative, is not isoimmunized, and has given
birth to a D-positive or weak-D-positive in-fant, 300 micrograms of anti-D immune globulin should be
administered postpartum, ideally within 72 hours of giving birth.
This dose
may be inadequate in circumstances in which there is a potential for greater-than-average
fetal-to-maternal hemorrhage, such as placental abruption, placenta previa,
intrauterine manipulation, and manual removal of the pla-centa.
Universal immunization with
hepatitis B surface antigen (HbSAg1) is recommended for all newborns weighing
2000 g. In addition, all newborns receive a full range of screening tests.
Bowel and Bladder Function
It is common for a patient not to
have a bowel movement for the first 1 to 2 days after delivery, because
patients have often not eaten for a long period. Stool softeners may be
prescribed, especially if the patient has had a fourth-degree episiotomy repair
or a laceration involving the rec-tal mucosa.
Hemorrhoids
are varicosities of the hemorrhoidalveins. Surgical
treatment should not be considered for at least 6 months postpartum to allow
for natural involution. Sitz baths, stool softeners, and local preparations are
use-ful, combined with reassurance that resolution is the most common outcome.
Periurethral edema after vaginal
delivery may cause transitory urinary retention. Patients’ urinary output shouldbe monitored for the first 24 hours
after delivery. If catheteriza-tion is required more than twice in the
first 24 hours, place-ment of an indwelling catheter for 1 to 2 days is
advisable.
Care of the Perineum
During the first 24 hours,
perineal pain can be minimized using oral analgesics and the application of an
ice bag to minimize swelling. Local anesthetics, such as witch hazel pads or
benzocaine spray, may be beneficial. Beginning 24 hours after delivery, moist
heat in the form of a warm sitz bath may reduce local discomfort and promote
healing.
Severe
perineal pain unresponsive to the usual analgesics may signify the development
of a hematoma, which requires
careful examination of the vulva, vagina, and rectum.
Infection of the episiotomy is
rare (<0.1%) and
usually is limited to the skin and responsive to broad-spectrum anti-biotics. Dehiscence (rupture of the incision) is
uncommon,with repair individualized on the basis of the nature and ex-tent of
the wound.
Contraception
Postpartum care in the hospital
should include discus-sion of contraception.Approximately 15% of non-nursingwomen are
fertile at 6 weeks postpartum. Combined estrogen–progestin oral
contraceptive preparations are not con-traindicated by breastfeeding, although
they may inhibit lactation slightly. Progestin preparations (oral
norethin-drone or depo-medroxyprogesterone acetate) have no effect or may
slightly facilitate lactation. Women may consider initiating progesterone-only
contraceptives at 6 weeks if breastfeeding exclusively or at 3 weeks if not
ex-clusively. Once lactation is established, neither the volume nor the
composition of breast milk are adversely affected by the administration of
hormonal contraceptives, and there is no effect on the growth of breastfed
infants. Insertion of intrauterine contraceptive 4 to 6 weeks post-partum is
acceptable in the appropriately selected patient.
Postpartum sterilization is performed at the time of cesarean delivery or after a vaginal delivery and should not extend the patient’s hospital stay. Ideally, postpartum minilaparotomy is performed before the onset of signif-icant uterine involution but following a full assessment of maternal and neonatal well-being. Postpartum minilaparotomy may be performed using local anesthesia with sedation, regional anesthesia, or general anesthesia. Postpartum sterilization requires counseling and informed consent before labor and deliv-ery. Consent should be obtained during prenatal care, when thepatient can make a considered decision, review the risks and ben-efits of the procedure, and consider alternative contraceptive methods. In all cases of intrapartum or postpartum medicalor obstetric complications, the physician should consider postponing sterilization to a later date. The federal and state regulations that address the timing of consent also are important to consider.
Sexual Activity
Coitus may be resumed when the
patient is comfortable; however, the risks
of hemorrhage and infection are minimalat approximately 2 weeks postpartum. Women
should becounseled, especially if breastfeeding, that coitus may ini-tially be
uncomfortable because of a lack of lubrication due to low estrogen levels, and
that the use of exogenous, water-soluble lubrication is helpful. The lactating
patient may also be counseled to apply topical estrogen or a lubricant to the
vaginal mucosa to minimize the dyspareunia caused by coital trauma to the
hypoestrogenic tissue. The female superior position may be recommended, as the
woman is thereby able to control the depth of penile penetration.
Patient Education
Patient education at the time of
discharge should not be solely focused on postpartum and contraceptive issues.
It is also a good opportunity to reinforce the value and need for healthcare of
both mother and infant. Follow-up care that has been arranged for the newborn
and frequency of healthcare for the new mother should be reviewed. High-risk
behaviors such as alcohol, tobacco, and drug abuse should be discussed, along
with appropriate interventions. Physicians should also assess the patient’s
mental state and her ease with care of the newborn. Infant safety concerns
(e.g., automobile child restraints) are also appropriate top-ics of discussion.
Postpartum follow-up of any preexisting medical conditions should also be
reviewed and, when needed, the patient should be referred for care.
Weight Loss
Maternal postpartum weight loss
can occur at a rate of 2 lb per month without affecting lactation. On average,
a woman will retain 2 lb more than her prepregnancy weight at 1 year
postpartum. There is no relationship between body mass index or total weight
gain and weight retention. Aging, rather than parity, is the major determinant
of in-creases in a woman’s weight over time.
Residual postpartum retention of
weight gained dur-ing pregnancy that results in obesity is a concern. Special
attention to lifestyle, including exercise and eating habits, will help these
women return to a normal body mass index.
Lactation and Breastfeeding
Because
breast milk is the ideal source of nutrition for the neonate, it is recommended
that women breastfeed exclusively for the first 6 months and continue
breastfeeding for as long as mutually desired. Benefits
of breastfeeding include decreasedrisks of otitis and respiratory infections,
diarrheal illness, sudden infant death, allergic and atopic disease,
juvenile-onset diabetes, and childhood cancers; fewer hospital admissions in
the first year of life; and improved cogni-tive function. For premature
infants, breast milk reduces the risk of necrotizing enterocolitis. Maternal
benefits include improved maternal–child attachment, reduced fertility due to
lactational amenorrhea, and reduced in-cidence of some hormonally sensitive
cancers, including breast cancer.
There are few contraindications
to breastfeeding. Women with HIV should not breastfeed due to the risk of
vertical transmission. Women with active, untreated tuber-culosis should not
have close contact with their infants until they have been treated and are
noninfectious; their breast milk may be expressed and given to the infant,
except in the rare case of tuberculosis mastitis. Mothers under-going chemotherapy,
receiving antimetabolites, or who have received radioactive materials should
not breastfeed until the breast milk has been cleared of these substances.
Infants with galactosemia should not be breastfed due to their sensitivity to
lactose. Mothers who use illegal drugs should not breastfeed their infants.
Drugs in
the breast milk are a common concern for the breastfeeding mother. Less than
1% of the total dosage ofany medication appears in breast milk. This should be
considered when any medication is prescribed by a physi-cian or when any
over-the-counter medications are con-templated by the patient. Specific
medications that would contraindicate breastfeeding include lithium carbonate,
tetracycline, bromocriptine, methotrexate, and any radio-active substance. All
substances of abuse are included as well, such as amphetamine, cocaine, heroin,
marijuana, and phencyclidine (PCP).
At the time of delivery, the drop
in estrogen levels and other placental hormones is a major factor in removing
the inhibition of the action of prolactin. Also, suckling by the infant
stimulates release of oxytocin from the neuro-hypophysis. The increased levels
of oxytocin in the blood result in contraction of the myoepithelial cells and
empty-ing of the alveolar lumen of the breast. The oxytocin also increases
uterine contractions, thereby accelerating invo-lution of the postpartum
uterus. Prolactin release is also stimulated by suckling, with resultant
secretion of fatty acids, lactose, and casein. Colostrum is produced in the first 5 days postpartum and is slowly
replaced by maternal milk. Colostrum contains more minerals and protein but
less fat and sugar than maternal milk, although it does contain large fat
globules, the so-called colostrum corpus-cles, which are probably epithelial
cells that have undergone fatty degeneration. Colostrum also contains
immuno-globulin A, which may offer the newborn some protection from enteric
pathogens. Subsequently, on approximately the third to sixth day postpartum,
milk is produced.
For milk to be produced on an
ongoing basis, there must be adequate insulin, cortisol, and thyroid hormone,
and adequate nutrients and fluids in the mother’s diet. The minimal caloric
requirement for adequate milk pro-duction in a woman of average size is 1800
kcal per day. In general, an additional 500 kcal of energy daily is
recom-mended throughout lactation. All vitamins except K are found in human
milk, but because they are present in vary-ing amounts, maternal vitamin
supplementation is recom-mended. Vitamin K may be administered to the infant to
prevent hemorrhagic disease of the newborn. To maintain breastfeeding, the
alveolar lumen must be emptied on a regular basis.
Nipple
care is also important during breastfeeding.The nipples
should be washed with water and exposed to the air for 15 to 20 minutes after
each feeding. A water-based cream such as lanolin or A and D ointment may be
applied if the nipples are tender. Fissuring of the nipple may make
breastfeeding extremely difficult. Temporary cessation of breastfeeding, manual
expression of milk, and use of a nipple shield will aid in recovery.
Related Topics