Chapter: Obstetrics and Gynecology: Postpartum Care
Anxiety, Depression, and the Postpartum Period
ANXIETY, DEPRESSION, AND THE POSTPARTUM PERIOD
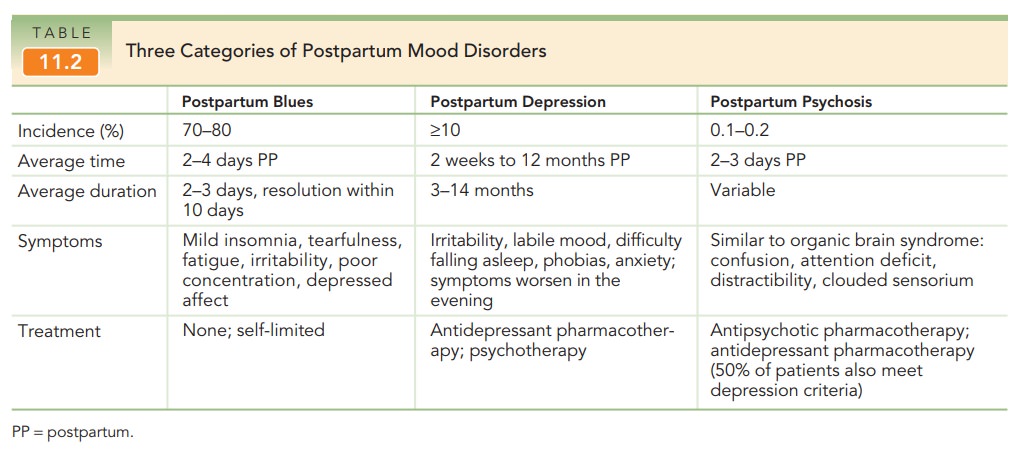
Although pregnancy and childbirth
are usually joyous times, depression to some degree is actually common in the
postpartum period. There is a wide spectrum of response to pregnancy and
delivery, ranging from mild postpartum blues to postpartum depression (Table
11.2). Approximately 70% to 80% of women report feeling sad, anxious, or angry
beginning 2–4 days after birth. These postpartumblues
may come and go throughout the day, are usuallymild, and abate within 1 to
2 weeks. Supportive care and reassurance are helpful in ensuring that symptoms
are self-limited. Approximately 10% to 15% of new mothers ex-perience postpartum depression (PPD), which is a
more serious disorder and usually requires medication and counseling. PPD differs from postpartum blues in the
sever-ity and duration of symptoms. Women with PPD have pro-nounced
feelings of sadness, anxiety, and despair that interfere with activities of
daily living. These symptoms do not abate, but instead worsen over several
weeks. Postpartum psychosis is the
most severe form of men-tal derangement and is most common in women with
preexisting disorders, such as manic–depressive illness or schizophrenia. This
condition should be considered a medical emergency and the patient should be
referred for immediate, often inpatient, treatment.
While the exact cause of PPD is
unknown, several associated factors have been identified. The normal hor-monal
fluctuations that occur following birth may trigger depression in some women.
Women who have a personal or family history of depression or anxiety may be
more likely to develop PPD. Acute stressors, including those specific to motherhood
(childcare), or other stressors (e.g., death of a family member) may contribute
to the development of PPD. Having a child with a difficult tem-perament or
health issues may lead the mother to doubt her ability to care for her newborn,
which can lead to depres-sion. The age of the mother may influence
susceptibility to PPD, with younger women more likely to experience depression
than older women. Toxins, poor diet, crowded living conditions, low
socioeconomic status, and low social support may also play a role. A strong predictor of PPD isdepression
during pregnancy. It is estimated that half of allcases of PPD may begin
during pregnancy. PPD may also be a continuation of a depressive disorder that
existed prior to pregnancy, rather than a new disorder.
Treatment must be tailored to the
patient’s individ-ual situation. Postpartum blues do not require treatment
other than support and reassurance. Women with PPD should receive mental health
counseling and medica-tion, if warranted. Effective therapies for the treatment
of PPD include cognitive-behavioral and interpersonal therapies.
Related Topics