Chapter: Psychiatric Mental Health Nursing : Mood Disorders
Major Depressive Disorder
MAJOR DEPRESSIVE DISORDER
Major depressive disorder typically involves 2 or more weeks of a
sad mood or lack of interest in life activities with at least four other
symptoms of depression such as anhedonia and changes in weight, sleep, energy,
concen-tration, decision making, self-esteem, and goals. Major depression is
twice as common in women and has a 1.5 to 3 times greater incidence in
first-degree relatives than in the general population. Incidence of depression
decreases with age in women and increases with age in men. Single and divorced
people have the highest incidence. Depres-sion in prepubertal boys and girls
occurs at an equal rate (Kelsoe, 2005).
Onset and Clinical Course
An untreated episode of depression can last 6 to 24 months before
remitting. Fifty to sixty percent of people who have one episode of depression
will have another. After a sec-ond episode of depression, there is a 70% chance
of recur-rence. Depressive symptoms can vary from mild to severe. The degree of
depression is comparable with the person’s sense of helplessness and
hopelessness. Some people with severe depression (9%) have psychotic features
(APA, 2000).
Treatment and Prognosis
Psychopharmacology
Major categories of antidepressants include cyclic
antide-pressants, monoamine oxidase inhibitors (MAOIs), selec-tive serotonin
reuptake inhibitors (SSRIs), and atypical antidepressants. The choice of which
antidepressant to use is based on the cli-ent’s symptoms, age, and physical health
needs; drugs that have or have not worked in the past or that have worked for a
blood relative with depression; and other medica-tions that the client is
taking.
Researchers believe that levels of neurotransmitters, especially
norepinephrine and serotonin, are decreased in depression. Usually, presynaptic
neurons release these neurotransmitters to allow them to enter synapses and
link with postsynaptic receptors. Depression results if too few
neurotransmitters are released, if they linger too briefly in synapses, if the
releasing presynaptic neurons reabsorb them too quickly, if conditions in
synapses do not support linkage with postsynaptic receptors, or if the number
of postsynaptic receptors has decreased. The goal is to increase the efficacy
of available neurotransmitters and the absorption by postsynaptic receptors. To
do so, antide-pressants establish a blockade for the reuptake of
norepi-nephrine and serotonin into their specific nerve terminals. This permits
them to linger longer in synapses and to be more available to postsynaptic
receptors. Antidepressants also increase the sensitivity of the postsynaptic
receptor sites (Rush, 2005).
In clients who have acute depression with psychotic features, an
antipsychotic is used in combination with an antidepressant. The antipsychotic
treats the psychotic fea-tures; several weeks into treatment, the client is
reassessed to determine whether the antipsychotic can be withdrawn and the
antidepressant maintained.
Evidence is increasing that antidepressant therapy should continue
for longer than the 3 to 6 months origi-nally believed necessary. Fewer
relapses occur in people with depression who receive 18 to 24 months of
antide-pressant therapy. As a rule, the dosage of antidepressants should be
tapered before being discontinued.
Selective Serotonin Reuptake Inhibitors. SSRIs, the newest category of antidepressants
(Table 15.1), are effective for most clients. Their action is specific to
serotonin reuptake inhibition; these drugs produce few sedating, anticholinergic,
and cardiovascular side effects, which make them safer for use in older adults.
Because of their low side effects and relative safety, people using SSRIs are
more apt to be compli-ant with the treatment regimen than clients using more
trou-blesome medications. Insomnia decreases in 3 to 4 days, appetite returns
to a more normal state in 5 to 7 days, and energy returns in 4 to 7 days. In 7
to 10 days, mood, concen-tration, and interest in life improve.
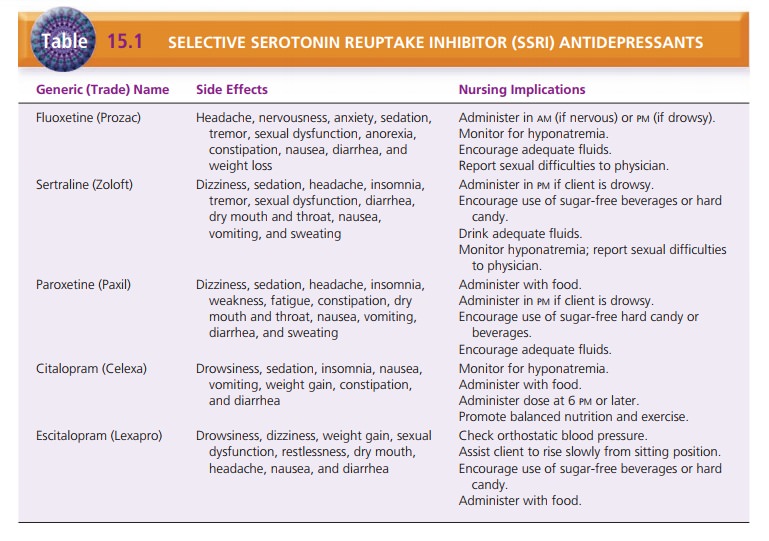
Fluoxetine (Prozac) produces a slightly higher rate of mild
agitation and weight loss but less somnolence. It has a half-life of more than
7 days, which differs from the 25-hour half-life of other SSRIs.
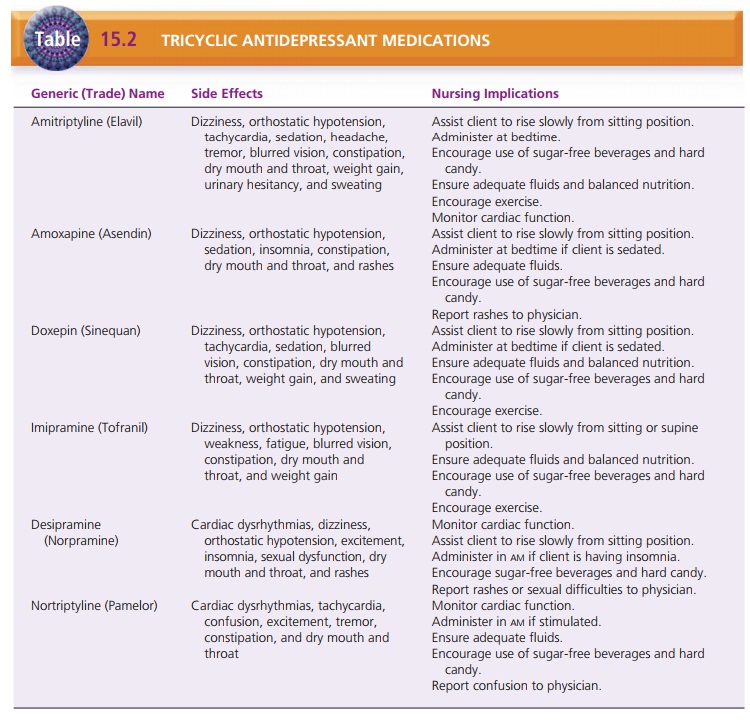
Cyclic Antidepressants. Tricyclics, introduced for
the treat-ment of depression in the mid-1950s, are the oldest antidepressants.
They relieve symptoms of hopelessness, helplessness, anhedonia, inappropriate
guilt, suicidal ide-ation, and daily mood variations (cranky in the morning and
better in the evening). Other indications include panic disor-der,
obsessive–compulsive disorder, and eating disorders. Each drug has a different
degree of efficacy in blocking the activity of norepinephrine and serotonin or
increasing the sensitivity of postsynaptic receptor sites. Tricyclic and
hetero-cyclic antidepressants have a lag period of 10 to 14 days before
reaching a serum level that begins to alter symptoms; they take 6 weeks to
reach full effect. Because they have a long serum half-life, there is a lag
period of 1 to 4 weeks be-fore steady plasma levels are reached and the
client’s symp-toms begin to decrease. They cost less primarily because they
have been around longer and generic forms are available.
Tricyclic antidepressants are contraindicated in severe impairment
of liver function and in myocardial infarction (acute recovery phase). They
cannot be given concurrently with MAOIs. Because of their anticholinergic side
effects, tricyclic antidepressants must be used cautiously in clients who have
glaucoma, benign prostatic hypertrophy, urinary retention or obstruction,
diabetes mellitus, hyperthyroid-ism, cardiovascular disease, renal impairment,
or respira-tory disorders (Table 15.2).
Overdosage of tricyclic antidepressants occurs over sev-eral days
and results in confusion, agitation, hallucinations, hyperpyrexia, and
increased reflexes. Seizures, coma, and cardiovascular toxicity can occur with
ensuing tachycardia, decreased output, depressed contractility, and
atrioventricular block. Because many older adults have concomitant health
problems, cyclic antidepressants are used less often in the geriatric
population than newer types of antidepressants that have fewer side effects and
less drug interactions.
Tetracyclic Antidepressants. Amoxapine (Asendin) may cause extrapyramidal
symptoms, tardive dyskinesia, and neuroleptic malignant syndrome. It can create
tolerance in 1 to 3 months. It increases appetite and causes weight gain and
cravings for sweets.
Maprotiline (Ludiomil) carries a risk for seizures (espe-cially in
heavy drinkers), severe constipation and urinary retention, stomatitis, and
other side effects; this leads to poor compliance. The drug is started and
withdrawn grad-ually. Central nervous system depressants can increase the
effects of this drug.
Atypical Antidepressants. Atypical antidepressants are used when the client has an
inadequate response to or side effects from SSRIs. Atypical antidepressants
include venla-faxine (Effexor), duloxetine (Cymbalta), bupropion (Well-butrin),
nefazodone (Serzone), and mirtazapine (Remeron) (Table 15.3).
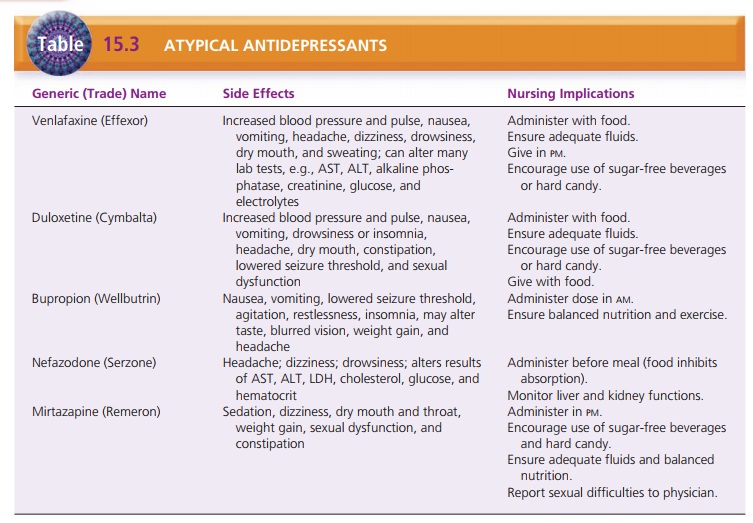
Venlafaxine blocks the reuptake of serotonin, norepineph-rine, and dopamine (weakly). Duloxetine selectively blocks both serotonin and norepinephrine. Bupropion modestly inhibits the reuptake of norepinephrine, weakly inhibits the reuptake of dopamine, and has no effects on serotonin. Bupropion is marketed as Zyban for smoking cessation.
Nefazodone inhibits the reuptake of serotonin and nor-epinephrine
and has few side effects. Its half-life is 4 hours, and it can be used in
clients with liver and kidney disease. It increases the action of certain
benzodiazepines (alprazo-lam, estazolam, and triazolam) and the H2 blocker
terfen-adine. Remeron also inhibits the reuptake of serotonin and
norepinephrine, and it has few sexual side effects; how-ever, its use comes
with a higher incidence of weight gain, sedation, and anticholinergic side
effects (Facts and Comparisons, 2009).
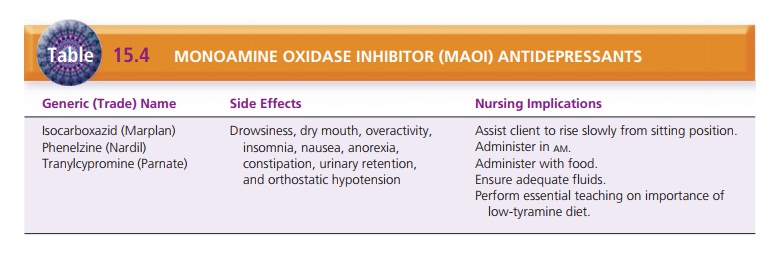
Monoamine Oxidase Inhibitors. MAOIs are used infre-quently
because of potentially fatal side effects and interac-tions with numerous
drugs, both prescription and over-the-counter preparations (Table 15.4). The
most seri-ous side effect is hypertensive
crisis, a life-threatening con-dition that can result when a client taking
MAOIs ingests tyramine-containing foods
and flu-ids or other medications. Symptoms are occipital headache,
hypertension, nausea, vomiting, chills, sweating, restless-ness, nuchal
rigidity, dilated pupils, fever, and motor agita-tion. These can lead to
hyperpyrexia, cerebral hemorrhage, and death. The MAOI–tyramine interaction
produces symp-toms within 20 to 60 minutes after ingestion. For hypertensive
crisis, transient antihypertensive agents, such as phentolamine mesylate, are
given to dilate blood vessels and decrease vascu-lar resistance (Facts and
Comparisons, 2009).
There is a 2- to 4-week lag period before MAOIs reach therapeutic
levels. Because of the lag period, adequate washout periods of 5 to 6 weeks are
recommended between the times that the MAOI is discontinued and another class
of antidepressant is started.
Other Medical Treatments and Psychotherapy
Electroconvulsive Therapy. Psychiatrists may use electro-convulsive therapy (ECT) to treat depression in selectgroups, such as
clients who do not respond to antidepres-sants or those who experience
intolerable side effects at therapeutic doses (particularly true for older
adults). In addition, pregnant women can safely have ECT with no harm to the
fetus. Clients who are actively suicidal may be given ECT if there is concern
for their safety while waiting weeks for the full effects of antidepressant
medication.
ECT involves application of electrodes to the head of the client to
deliver an electrical impulse to the brain; this causes a seizure. It is
believed that the shock stimulates brain chemistry to correct the chemical
imbalance of depression. Historically, clients did not receive any anes-thetic
or other medication before ECT, and they had full-blown grand mal seizures that
often resulted in injuries ranging from biting the tongue to breaking bones.
ECT fell into disfavor for a period and was seen as “barbaric.” Today, although
ECT is administered in a safe and humane way with almost no injuries, there are
still critics of the treatment.
Clients usually receive a series of 6 to 15 treatments scheduled
thrice a week. Generally, a minimum of six treatments are needed to see
sustained improvement in depressive symptoms. Maximum benefit is achieved in 12
to 15 treatments.
Preparation of a client for ECT is similar to preparation for any
outpatient minor surgical procedure: The client receives nothing by mouth (or,
is NPO) after midnight, removes any fingernail polish, and voids just before
the procedure. An intravenous line is started for the adminis-tration of
medication.
Initially, the client receives a short-acting anesthetic so he or
she is not awake during the procedure. Next, he or she receives a muscle
relaxant/paralytic, usually succinylcho-line, which relaxes all muscles to
reduce greatly the outwardsigns of the seizure (e.g., clonic–tonic muscle
contractions). Electrodes are placed on the client’s head: one on either side
(bilateral) or both on one side (unilateral). The electrical stimulation is
delivered, which causes seizure activity in the brain that is monitored by an
electroencephalogram, or EEG. The client receives oxygen and is assisted to
breathe with an Ambu bag. He or she generally begins to waken after a few
minutes. Vital signs are monitored, and the client is assessed for the return
of a gag reflex.
After ECT treatment, the client may be mildly confused or briefly
disoriented. He or she is very tired and often has a headache. The symptoms are
just like those of anyone who has had a grand mal seizure. In addition, the
client will have some short-term memory impairment. After a treatment, the
client may eat as soon as he or she is hungry and usually sleeps for a period.
Headaches are treated symptomatically.
Unilateral ECT results in less memory loss for the cli-ent, but
more treatments may be needed to see sustained improvement. Bilateral ECT
results in more rapid improve-ment but with increased short-term memory loss.
The literature continues to be divided about the effective-ness of
ECT. Some studies report that ECT is as effective as medication for depression,
whereas other studies report only short-term improvement. Likewise, some
studies report that memory loss side effects of ECT are short lived, whereas
oth-ers report they are serious and long term (Fenton, Fasula, Ostroff, &
Sanacora, 2006; Ross, 2006).
ECT is also used for relapse prevention in depression. Clients may
continue to receive treatments, such as one per month, to maintain their mood
improvement. Often, clients are given antidepressant therapy after ECT to
pre-vent relapse. Studies have found maintenance ECT to be effective in relapse
prevention (Frederikse, Petrides, & Kellner, 2006).
Psychotherapy. A combination of
psychotherapy and medications is considered the most effective
treatment for depressive disorders. There is no one specific type of ther-apy
that is better for the treatment of depression (Rush, 2005). The goals of
combined therapy are symptom remis-sion, psychosocial restoration, prevention
of relapse or recurrence, reduced secondary consequences such as marital
discord or occupational difficulties, and increasing treatment compliance.
Interpersonal therapy focuses on difficulties in relation-ships,
such as grief reactions, role disputes, and role tran-sitions. For example, a
person who, as a child, never learned how to make and trust a friend outside
the family structure has difficulty establishing friendships as an adult.
Interpersonal therapy helps the person to find ways to accomplish this
developmental task.
Behavior therapy seeks to increase the frequency of the client’s
positively reinforcing interactions with the envi-ronment and to decrease
negative interactions. It also may focus on improving social skills.
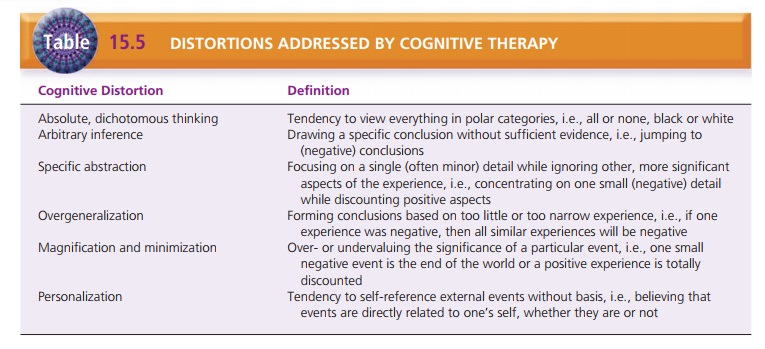
Cognitive therapy focuses on how the person thinks about the self,
others, and the future and interprets his or her experiences. This model
focuses on the person’s distorted thinking, which, in turn, influences
feelings, behavior, and functional abilities. Table 15.5 describes the
cognitive distor-tions that are the focus of cognitive therapy.
Investigational Treatments. Other treatments for
depres-sion are being tested. These include transcranial magnetic stimulation
(TMS), magnetic seizure therapy, deep brain stimulation, and vagal nerve
stimulation. TMS is the closest to approval for clinical use. These novel
brain-stimulation techniques seem to be safe, but their efficacy in relieving
depression needs to be established (Eitan & Lerer, 2006).
Related Topics