Chapter: Psychiatric Mental Health Nursing : Mood Disorders
Application of the Nursing Process: Depression
APPLICATION OF THE NURSING
PROCESS: DEPRESSION
Assessment
History
The nurse can collect assessment data from the client and family or
significant others, previous chart information, and others involved in the
support or care. It may take several short periods to complete the assessment
because clients who are severely depressed feel exhausted and overwhelmed. It
can take time for them to process the question asked and to formulate a
response. It is important that the nurse does not try to rush clients because
doing so leads to frustration and incomplete assessment data.
To assess the client’s perception of the problem, the nurse asks
about behavioral changes: when they started, what was happening when they
began, their duration, and what the client has tried to do about them.
Assessing the history is important to determine any previous episodes of
depression, treatment, and client’s response to treatment. The nurse also asks about
family history of mood disor-ders, suicide, or attempted suicide.
General Appearance and Motor Behavior
Many people with depression look sad; sometimes they just look ill.
The posture often is slouched with head down, and they make minimal eye contact.
They have psychomotor retardation (slow
body movements, slow cognitive
processing, and slow verbal interaction). Responses to questions may be
minimal, with only one or two words. Latency
of response is seen when clients take up to 30 seconds to respond to a
question. They may answer some questions with “I don’t know” because they are
simply too fatigued and overwhelmed to think of an answer or respond in any
detail. Clients also may exhibit signs of agitation or anxiety such as wringing
their hands and having difficulty sitting still. These clients are said to have
psychomotor agitation (increased
body movements and thoughts), which includes pacing, accelerated think-ing, and
argumentativeness.
Mood and Affect
Clients with depression may describe themselves as hope-less,
helpless, down, or anxious. They also may say they are a burden on others or
are a failure at life, or they may make other similar statements. They are
easily frustrated, are angry with themselves, and can be angry with others
(APA, 2000). They experience anhedonia,
losing any sense of pleasure from activities they formerly enjoyed. Clients may
be apathetic, that is, not caring about self, activities, or much of anything.
Their affect is sad or depressed or may be flat with no emotional
expressions. Typically, depressed clients sit alone, staring into space or lost
in thought. When addressed, they interact minimally with a few words or a
gesture. They are overwhelmed by noise and people who might make demands on
them, so they withdraw from the stimulation of interaction with others.
Thought Process and Content
Clients with depression experience slowed thinking pro-cesses:
their thinking seems to occur in slow motion. With severe depression, they may
not respond verbally to ques-tions. Clients tend to be negative and pessimistic
in their thinking, that is, they believe that they will always feel this bad,
things will never get any better, and nothing will help. Clients make
self-deprecating remarks, criticizing them-selves harshly and focusing only on
failures or negative attributes. They tend to ruminate, which is repeatedly going over the same thoughts. Those
who experience psychotic symptoms have delusions; they often believe they are
responsible for all the tragedies and miseries in the world.
Often clients with depression have thoughts of dying or committing
suicide. It is important to assess suicidal ideation by asking about it
directly. The nurse may ask, “Are you thinking about suicide?” or “What
suicidal thoughts are you having?” Most clients readily admit to suicidal
thinking.
Sensorium and Intellectual Processes
Some clients with depression are oriented to person, time, and
place; others experience difficulty with orientation, especially if they
experience psychotic symptoms or are withdrawn from their environment.
Assessing general knowledge is difficult because of their limited ability to
respond to questions. Memory impairment is common. Clients have extreme
difficulty concentrating or paying attention. If psychotic, clients may hear
degrading and belittling voices or they may even have command halluci-nations
that order them to commit suicide.
Judgment and Insight
Clients with depression experience impaired judgment because they
cannot use their cognitive abilities to solve problems or to make decisions.
They often cannot make decisions or choices because of their extreme apathy or
their negative belief that it “doesn’t matter anyway.”
Insight may be intact, especially if clients have been depressed
previously. Others have very limited insight and are totally unaware of their
behavior, feelings, or even their illness.
Self-Concept
Sense of self-esteem is greatly reduced; clients often use phrases
such as “good for nothing” or “just worthless” to describe themselves. They feel
guilty about not being able to function and often personalize events or take
responsi-bility for incidents over which they have no control. They believe
that others would be better off without them, a belief which leads to suicidal
thoughts.
Roles and Relationships
Clients with depression have difficulty fulfilling roles and
responsibilities. The more severe the depression, the greater the difficulty.
They have problems going to work or school; when there, they seem unable to
carry out their responsibilities. The same is true with family
responsibili-ties. Clients are less able to cook, clean, or care for chil-dren.
In addition to the inability to fulfill roles, clients become even more
convinced of their “worthlessness” for being unable to meet life responsibilities.
Depression can cause great strain in relationships. Fam-ily members
who have limited knowledge about depression may believe clients should “just
get on with it.” Clients often avoid family and social relationships because
they feel overwhelmed, experience no pleasure from interactions, and feel
unworthy. As clients withdraw from relationships, the strain increases.
Physiologic and Self-Care Considerations
Clients with depression often experience pronounced weight loss
because of lack of appetite or disinterest in eat-ing. Sleep disturbances are
common: either clients cannot sleep, or they feel exhausted and unrefreshed no
matter how much time they spend in bed. They lose interest in sexual
activities, and men often experience impotence. Some clients neglect personal
hygiene because they lack the interest or energy. Constipation commonly results
from decreased food and fluid intake as well as from inac-tivity. If fluid
intake is severely limited, clients also may be dehydrated.
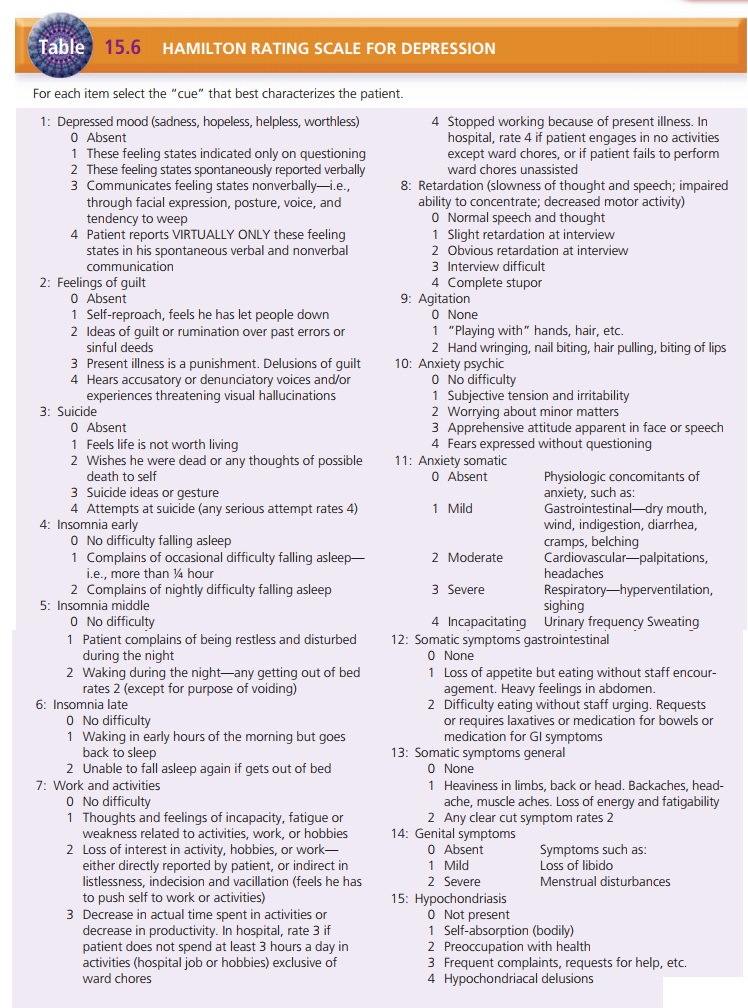
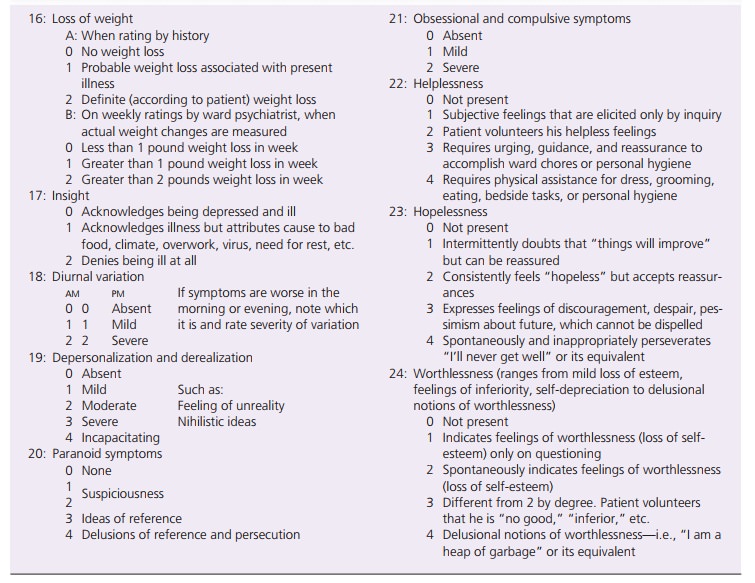
Depression Rating Scales
Clients complete some rating scales for depression; mental health
professionals administer others. These assessment tools, along with evaluation
of behavior, thought pro-cesses, history, family history, and situational
factors, help to create a diagnostic picture. Self-rating scales of depres-sive
symptoms include the Zung Self-Rating Depression Scale and the Beck Depression
Inventory. Self-rating scales are used for case finding in the general public
and may be used over the course of treatment to determine improve-ment from the
client’s perspective.
The Hamilton Rating Scale for Depression (Table 15.6) is a
clinician-rated depression scale used like a clinical interview. The clinician
rates the range of the client’s behaviors such as depressed mood, guilt,
suicide, and insomnia. There is also a section to score diurnal varia-tions,
depersonalization (sense of unreality about the self), paranoid symptoms, and
obsessions.
Data Analysis
The nurse analyzes assessment data to determine priorities and to
establish a plan of care. Nursing diagnoses com-monly established for the
client with depression include the following:
·
Risk for Suicide
·
Imbalanced Nutrition: Less Than Body Requirements
·
Anxiety
·
Ineffective Coping
·
Hopelessness
·
Ineffective Role Performance
·
Self-Care Deficit
·
Chronic Low Self-Esteem
·
Disturbed Sleep Pattern
·
Impaired Social Interaction
Outcome Identification
Outcomes for clients with depression relate to how the depression
is manifested—for instance, whether or not the person is slow or agitated,
sleeps too much or too little, or eats too much or too little. Examples of
outcomes for a client with the psychomotor retardation form of depres-sion
include the following:
·
The client will not injure himself or herself.
·
The client will independently carry out activities of daily living
(showering, changing clothing, grooming).
·
The client will establish a balance of rest, sleep, and activity.
·
The client will establish a balance of adequate nutri-tion,
hydration, and elimination.
·
The client will evaluate self-attributes realistically.
·
The client will socialize with staff, peers, and family/ friends.
The client will return to occupation or school activities.
·
The client will comply with antidepressant regimen.
·
The client will verbalize symptoms of a recurrence.
Intervention
Providing for Safety
The first priority is to determine whether a client with depression
is suicidal. If a client has suicidal ideation or hears voices commanding him
or her to commit suicide, measures to provide a safe environment are necessary.
If the client has a suicide plan, the nurse asks additional questions to
determine the lethality of the intent and plan. The nurse reports this information
to the treatment team. Health care personnel follow hospital or agency policies
and procedures for instituting suicide
precau-tions (e.g., removal of harmful items, increased supervi-sion).
Promoting a Therapeutic Relationship
It is important to have meaningful contact with clients who have
depression and to begin a therapeutic relationship regardless of the state of
depression. Some clients are quite open in describing their feelings of
sadness, hopelessness, helplessness, or agitation. Clients may be unable to
sustain a long interaction, so several shorter visits help the nurse to assess
status and to establish a therapeutic relationship.
The nurse may find it difficult to interact with these cli-ents
because of empathy with such sadness and depression. The nurse also may feel
unable to “do anything” for clients with limited responses. Clients with
psychomotor retarda-tion (slow speech, slow movement, slow thought processes)
are very noncommunicative or may even be mute. The nurse can sit with such clients
for a few minutes at intervals throughout the day. The nurse’s presence conveys
genuine interest and caring. It is not necessary for the nurse to talk to
clients the entire time; rather, silence can convey that cli-ents are
worthwhile even if they are not interacting.
“My name is
Sheila. I’m your nurse today. I’m going to sit with you for a few minutes. If
you need anything, or if you would like to talk, please tell me.”
After time has elapsed, the nurse would say the following:
“I’m going now.
I will be back in an hour to see you again.”
It is also important that the nurse avoids being overly cheerful or
trying to “cheer up” clients. It is impossible to coax or to humor clients out
of their depression. In fact, an overly cheerful approach may make clients feel
worse or convey a lack of understanding of their despair.
Promoting Activities of Daily Living and Physical Care
The ability to perform daily activities is related to the level of
psychomotor retardation. To assess ability to perform activities of daily
living independently, the nurse first asks the client to perform the global
task. For example,
“Martin, it’s
time to get dressed.” (global task)
If a client cannot respond to the global request, the nurse breaks
the task into smaller segments. Clients with depres-sion can become overwhelmed
easily with a task that has several steps. The nurse can use success in small,
concrete steps as a basis to increase self-esteem and to build compe-tency for
a slightly more complex task the next time.
If clients cannot choose between articles of clothing, the nurse
selects the clothing and directs clients to put them on. For example,
“Here are your
gray slacks. Put them on.”
This still allows clients to participate in dressing. If this is
what clients are capable of doing at this point, this activity will reduce
dependence on staff. This request is concrete, and if clients cannot do this,
the nurse has infor-mation about the level of psychomotor retardation.
If a client cannot put on slacks, the nurse assists by saying,
“Let me help you with your slacks, Martin.”
The nurse helps clients to dress only when they cannot perform any
of the above steps. This allows clients to do as much as possible for
themselves and to avoid becoming dependent on the staff. The nurse can carry
out this same process with clients when they eat, take a shower, and per-form
routine self-care activities.
Because abilities change over time, the nurse must assess them on
an ongoing basis. This continual assess-ment takes more time than simply
helping clients to dress. Nevertheless, it promotes independence and provides
dynamic assessment data about psychomotor abilities.
Often, clients decline to engage in activities because they are too
fatigued or have no interest. The nurse can validate these feelings yet still
promote participation. For example,
“I know you
feel like staying in bed, but it is time to get up for breakfast.”
Often, clients may want to stay in bed until they “feel like
getting up” or engaging in activities of daily living. The nurse can let
clients know they must become more active to feel better rather than waiting
passively for improvement. It may be helpful to avoid asking “yes-or-no”
questions. Instead of asking, “Do you want to get up now?” the nurse would say,
“It is time to get up now.”
Reestablishing balanced nutrition can be challenging when clients
have no appetite or don’t feel like eating. The nurse can explain that
beginning to eat helps stimulate appe-tite. Food offered frequently and in
small amounts can pre-vent overwhelming clients with a large meal that they
feel unable to eat. Sitting quietly with clients during meals can promote
eating. Monitoring food and fluid intake may be necessary until clients are
consuming adequate amounts.
Promoting sleep may include the short-term use of a sedative or
giving medication in the evening if drowsiness or sedation is a side effect. It
is also important to encourage clients to remain out of bed and active during
the day to facilitate sleeping at night. It is important to monitor the number
of hours clients sleep as well as whether they feel refreshed on awakening.
Using Therapeutic Communication
Clients with depression are often overwhelmed by the intensity of
their emotions. Talking about these feelings can be beneficial. Initially, the
nurse encourages clients to describe in detail how they are feeling. Sharing
the burden with another person can provide some relief. At these times, the
nurse can listen attentively, encourage clients, and validate the intensity of
their experience. For example,
Nurse: “How are you feeling today?” (broadopening)
Client: “I feel so awful . . . terrible.”
Nurse: “Tell me more. What is that like for you?” (using a general lead;
encouraging description)
Client: “I don’t feel like myself. I don’t know what to do.”
Nurse: “That must be frightening.” (validating)
It is important at this point that the nurse does not attempt to
“fix” the client’s difficulties or offer clichés such as “Things will get
better” or “But you know your family really needs you.” Although the nurse may
have good intentions, remarks of this type belittle the client’s feelings or
make the client feel more guilty and worthless.
As clients begin to improve, the nurse can help them to learn or
rediscover more effective coping strategies such as talking to friends,
spending leisure time to relax, taking positive steps to deal with stressors,
and so forth. Improved coping skills may not prevent depression but may assist
cli-ents to deal with the effects of depression more effectively.
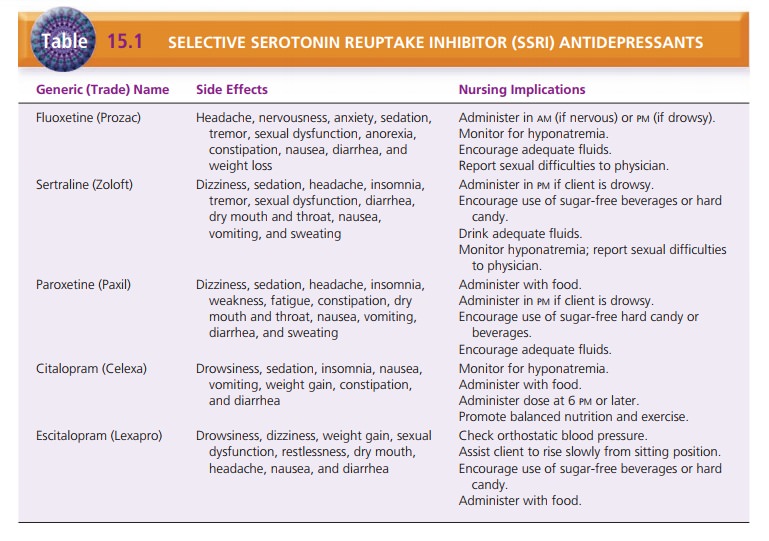
Managing Medications
The increased activity and improved mood that antidepres-sants
produce can provide the energy for suicidal clients to carry out the act. Thus,
the nurse must assess suicide risk even when clients are receiving
antidepressants. It is also important to ensure that clients ingest the
medication and are not saving it in attempt to commit suicide. As clients
become ready for discharge, careful assessment of suicide potential is
important because they will have a supply of antidepressant medication at home.
SSRIs are rarely fatal in overdose, but cyclic and MAOI antidepressants are
poten-tially fatal. Prescriptions may need to be limited to only a 1-week
supply at a time if concerns linger about overdose.
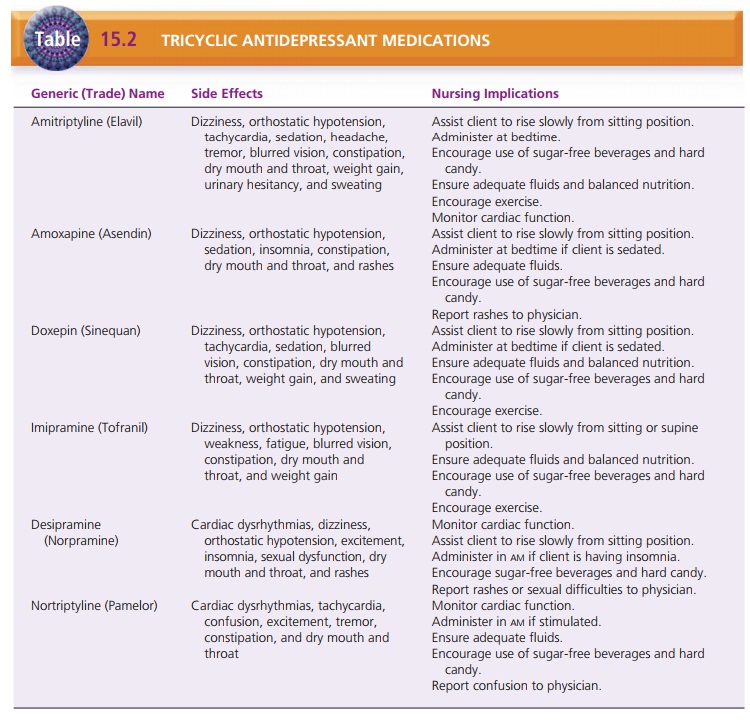
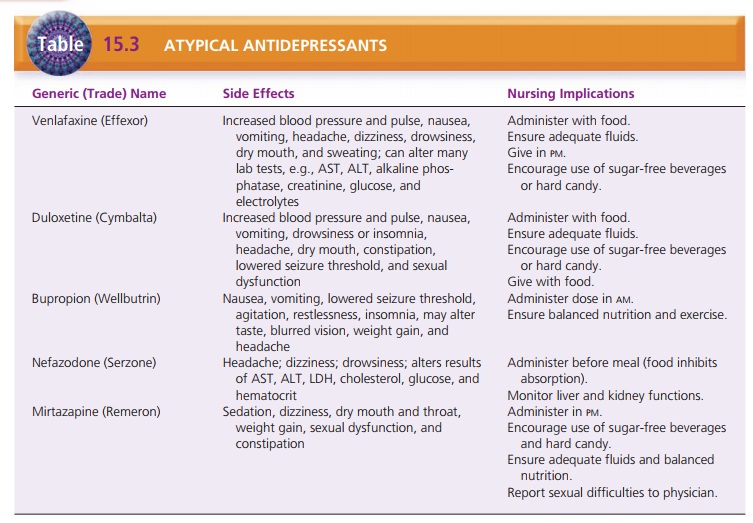
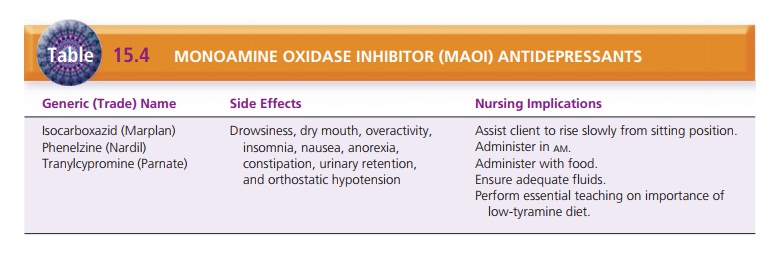
An important component of client care is management of side
effects. The nurse must make careful observations and ask clients pertinent
questions to determine how they are tolerating medications. Tables 15.1 through
15.4 give specific interventions to manage side effects of antidepres-sant
medications.
Clients and family must learn how to manage the medi-cation regimen
because clients may need to take these medications for months, years, or even a
lifetime. Educa-tion promotes compliance. Clients must know how often they need
to return for monitoring and diagnostic tests.
Providing Client and Family Teaching
Teaching clients and family about depression is important. They
must understand that depression is an illness, not a lack of willpower or
motivation. Learning about the begin-ning symptoms of relapse may assist
clients to seek treat-ment early and avoid a lengthy recurrence.
Clients and family should know that treatment out-comes are best
when psychotherapy and antidepressants are combined. Psychotherapy helps
clients to explore anger, dependence, guilt, hopelessness, helplessness, object
loss, interpersonal issues, and irrational beliefs. The goal is to reverse
negative views of the future, improve self-image, and help clients gain
competence and self-mas-tery. The nurse can help clients to find a therapist
through mental health centers in specific communities.
Support group participation also helps some clients and their
families. Clients can receive support and encourage-ment from others who
struggle with depression, and fam-ily members can offer support to one another.
The National Alliance for the Mentally Ill is an organization that can help
clients and families connect with local support groups.
Evaluation
Evaluation of the plan of care is based on achievement of
individual client outcomes. It is essential that clients feel safe and do not
experience uncontrollable urges to commit suicide. Participation in therapy and
medication compli-ance produce more favorable outcomes for clients with
depression. Being able to identify signs of relapse and to seek treatment
immediately can significantly decrease the severity of a depressive episode.
Related Topics