Chapter: Clinical Anesthesiology: Anesthetic Management: Hepatic Physiology & Anesthesia
Liver Tests
LIVER TESTS
The most commonly performed liver tests are nei-ther sensitive nor
specific. No one test evaluates overall hepatic function, reflecting instead
one aspect of hepatic function that must be interpreted in conjunction with
other tests and clinical assess-ment of the patient.
Many “liver function” tests, such as serum
transaminase measurements, reflect hepato-
cellular integrity more than hepatic
function. Liver tests that measure hepatic synthetic function include
serum albumin, prothrombin time (PT, or inter-national normalized ratio
[INR]), cholesterol, and pseudocholinesterase. Moreover, because of the liver’s
large functional reserve, substantial cirrhosis may be present with few or no
laboratory abnormalities.
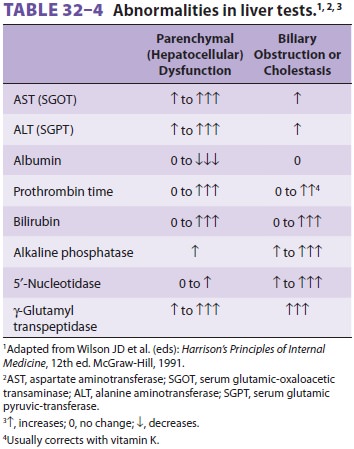
Liver abnormalities can often be divided into either parenchymal
disorders or obstructive dis-orders based on laboratory tests (Table 32–4). Obstructive disorders
primarily affect biliary excre-tion of substances, whereas parenchymal
disorders result in generalized hepatocellular dysfunction.
Serum Bilirubin
The normal total bilirubin concentration,
composed of conjugated (direct), water-soluble and uncon-jugated (indirect),
lipid-soluble forms, is less than 1.5 mg/dL (<25 mmol/L) and reflects the balance between
bilirubin production and excretion. Jaundice is usually clinically obvious when
total bilirubin exceeds 3 mg/dL. A predominantly conjugated hyper-bilirubinemia
(>50%) is associated with
increased urinary urobilinogen and may reflect hepatocellular dysfunction,
congenital (Dubin–Johnson or Rotor syndrome) or acquired intrahepatic
cholestasis, or extrahepatic biliary obstruction. Hyperbilirubinemia that is
primarily unconjugated may be seen with hemolysis or with congenital (Gilbert
or Crigler– Najjar syndrome) or acquired defects in bilirubin conjugation.
Unconjugated bilirubin is neurotoxic, and high levels may produce
encephalopathy.
Serum Aminotransferases (Transaminases)
These enzymes are released into the circulation as a result of
hepatocellular injury or death. Two aminotransferases are most commonly
measured: aspartate aminotransferase (AST), also known as serum
glutamic-oxaloacetic transaminase (SGOT), and alanine aminotransferase (ALT),
also known as serum glutamic pyruvic-transferase (SGPT).
Serum Alkaline Phosphatase
Alkaline phosphatase is produced by the
liver, bone, small bowel, kidneys, and placenta and is excreted into bile.
Normal serum alkaline phosphatase activ-ity is generally 25–85 IU/L; children
and adolescents have much higher levels, reflecting active growth. Most of the
circulating enzyme is normally derived from bone; however, with biliary
obstruction, more hepatic alkaline phosphatase is synthesized and released into
the circulation.
Serum Albumin
The normal serum albumin
concentration is 3.5– 5.5 g/dL. Because its half-life is about 2–3 weeks,
albumin concentration may initially be normalwith
acute liver disease. Albumin values less than 2.5 g/dL are generally indicative
ofchronic liver disease, acute stress, or severe
malnu-trition. Increased losses of albumin in the urine (nephrotic syndrome) or
the gastrointestinal tract (protein-losing enteropathy) can also produce
hypoalbuminemia.
Blood Ammonia
Significant elevations of blood ammonia levels usually reflect
disruption of hepatic urea syn-thesis. Normal whole blood ammonia levels are
47–65 mmol/L (80–110 mg/dL). Marked elevations usually reflect severe
hepatocellular damage and may cause encephalopathy.
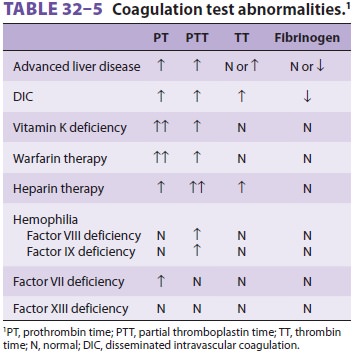
Prothrombin Time
The PT, which normally ranges between 11–14
sec, depending on the control value,measures the activity of fibrinogen,
prothrom-bin, and factors V, VII, and X. The relatively short half-life of
factor VII (4–6 h) makes the PT useful in evaluating hepatic synthetic function
of patients with acute or chronic liver disease. Prolongations of the PT
greater than 3–4 sec from the control are considered significant and usually
correspond to an INR 1.5. Because only 20% to 30% of normal factor activity is
required for normal coagulation, prolon-gation of the PT usually reflects
either severe liver disease or vitamin K deficiency. (See Table 32–5 for a list
of coagulation test abnormalities.)
Point-of-Care Viscoelastic Coagulation Monitoring
This technology provides a “real time”
assessment of the coagulation status and utilizes thromboelas-tography (TEG ®), rotation
thromboelastometry (ROTEM®), or Sonoclot® analysis to assess global coagulation via the viscoelastic properties
of whole blood (Figure 32–7). A clear picture is
provided of the global effect of imbalances between the proco-agulant and
anticoagulant systems and the profibri-nolytic and antifibrinolytic systems and
the resultant
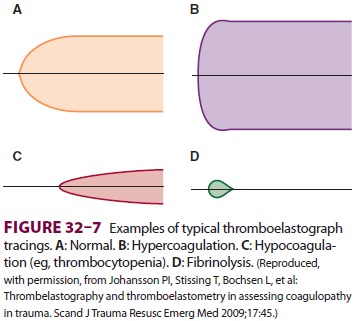
clot tensile strength, allowing precise management of hemostatic
therapy. The rate of clot formation, the strength of the clot, and the impact
of any lysis can be observed. The presence of disseminated intravas-cular
coagulation can be evaluated, as can the effect of heparin or heparinoid
activity. In addition, plate-let function can be assessed, including the
effects of platelet inhibition.
Related Topics