Chapter: Essentials of Psychiatry: Impulse Control Disorders
Intermittent Explosive Disorder
Intermittent
Explosive Disorder
Definition
Patients with intermittent explosive disorder have a problem with their temper (see DSMIV-TR criteria). This definition highlights the centrality of impulsive aggression in intermittent explo-sive disorder. Impulsive aggression, however, is not specific to intermittent explosive disorder. It is a key feature of several psy-chiatric disorders and nonpsychiatric conditions and may emerge during the course of yet other psychiatric disorders. Therefore, the definition of intermittent explosive disorder as formulated in the DSM-IV-TR is essentially a diagnosis of exclusion. As described in criterion C, a diagnosis of intermittent explosive disorder is made only after other mental disorders that might ac-count for episodes of aggressive behavior have been ruled out. The individual may describe the aggressive episodes as “spells” or “attacks”. The symptoms appear within minutes to hours and, regardless of the duration of the episode, may remit almost as quickly. As in other impulse control disorders, the explosive be-havior may be preceded by a sense of tension or arousal and is followed immediately by a sense of relief or release of tension Although not explicitly stated in the DSM-IV-TR definition of intermittent explosive disorder, impulsive aggressive behavior may have many motivations that are not meant to be includedwithin this diagnosis. Intermittent explosive disorder should not be diagnosed when the purpose of the aggression is monetary gain, vengeance, self-defense, social dominance, or expressing a political statement or when it occurs as a part of gang behavior. Typically, the aggressive behavior is egodystonic to individuals with intermittent explosive disorder, who feel genuinely upset, remorseful, regretful, bewildered, or embarrassed about their impulsive aggressive acts.
Etiology and Pathophysiology
Since the
second half of the 19th century, two main lines of explanation, which are to a
large extent complementary, have been developed to account for the existence of
individuals with episodic impulsive aggression. One line of explanation viewed
the etiology of impulsive aggression as stemming from the effects of early
childhood experiences and possibly childhood trauma on the development of
self-control, frustration tolerance, planning ability and gratification delay,
which are all important for self-prevention of impulsive aggressive outbursts.
Early experiences with “good-enough” mothering that fosters phase-appropriate
delay of gratification and the development of the potential for im-itation and
identification with the mother are considered impor-tant for normal
development. Too much or too little frustration, as well as overgratification
or undergratification, may impair the normal development of the ability to
anticipate frustration and delay gratification.
A second
line of explanation, which has yielded numer-ous positive findings during the
past 15 years, views impulsive aggression as the result of variations in brain
mechanisms that mediate behavioral arousal and behavioral inhibition. A rapidly
growing body of evidence has shown that impulsive aggression may be related to
defects in the brain serotonergic system, which acts as an inhibitor of motor
activity. Although the majority of studies involved patients who suffered from
impulsive aggression in the context of disorders other than intermittent
explosive dis-order, their findings may be relevant to the behavioral dimension
of impulsive aggression, of which intermittent explosive disorder is a “pure”
form. A number of researchers have confirmed a rela-tionship between levels of
5-hydroxyindoleacetic acid (5-HIAA) in the CSF and impulsive or aggressive
behaviors. Others have divided aggressive behaviors into impulsive and
nonimpulsive forms, and found that reduced CSF 5-HIAA levels were corre-lated
with impulsive aggression only. Pharmacological challenge studies of the
serotonergic system have also demonstrated that low serotonergic responsiveness
(as measured by the neuroen-docrine response to serotonergic agonists) correlates
with scores of impulsive aggression. Studies of impulsive aggression among
alcoholics have further defined a probable relationship between such behaviors
and diminished serotonergic function.
The
literature on serotonin and suicide, which may be viewed as an extreme form of
self-directed aggression, suggests another link between serotonin and
aggression. Postmortem studies found that brain stem levels of serotonin were
decreased in suicide victims, and reduced imipramine binding, which is thought
to be associated with reduced presynaptic serotonergic binding sites, was found
in the brains of suicide completers. Furthermore, an increase in postsynaptic
5-hydroxytryptamine (5-HT2) receptors was found in the brains of
suicide completers, and this finding was confirmed in subsequent studies. An
increase in 5-HT2 receptors, which are thought to be mostly
postsynaptic, may reflect the brain’s reaction to a decrease in functional
sero-tonergic neurons, with consequent upregulation of postsynaptic serotonin
binding sites
Another
line of neurobiological evidence links impulsive aggression with dysfunction of
the prefrontal cortex. Studies of neuropsychiatric patients with localized
structural brain lesions have demonstrated that some bilateral lesions in the
prefrontal cortex may be specifically associated with a chronic pattern of
impulsive aggressive behaviors. Neurological studies suggest that the
prefrontal cortical regions associated with impulsive aggression syndromes are
involved in the processing of affec-tive information and the inhibition of
motor responsiveness, both of which are impaired in patients with impulsive
aggres-sion. Interictal episodes of aggression may occur among some individuals
with epilepsy. In a quantitative MRI study of such episodes among individuals
with temporal lobe epilepsy (TLE) (Woermann et
al., 2000) three groups (24 TLE patients with ag-gressive behavior, 24 TLE
patients without such behavior and 35 nonpatient controls) were compared. The
researchers concluded that the aggressive behavior was associated with a
reduction of frontal neocortical gray matter.
Biological
studies implicate the serotonergic system and the prefrontal cortex in the
pathogenesis of impulsive aggression. The diagnosis of intermittent explosive
disorder is sometimes considered in forensic settings; the biological
correlates of im-pulsive aggression focus attention on, but do not solve, the
com-plicated problem of personal responsibility for impulsive violent acts that
are correlated with objective biological findings. Data from a study of
visual-evoked potentials and EEGs in a large group of children and adolescents
who demonstrated aggressive behavior also suggest that such behavior may be
associated with altered innate characteristics of central nervous system
function (Bars et al., 2001).
Assessment and Differential Diagnosis
Phenomenology and Variations in Presentation
Episodes
of violent behavior appear in several common psychi-atric disorders such as
antisocial personality disorder, borderline personality disorder and substance
use disorders and need to be distinguished from the violent episodes of
patients with intermit-tent explosive disorder, which are apparently rare. The
study of Felthous and coworkers (1991), in which 15 men with rigorously
diagnosed DSM-III-R intermittent explosive disorder were iden-tified from among
a group of 443 men who complained of vio-lence, permitted some systematic
observations about the “typical violent episode” as reported by patients with
intermittent explo-sive disorder.
In the
vast majority of instances, the subjects with inter-mittent explosive disorder
identified their spouse, lover, or girl-friend or boyfriend as a provocateur of
their violent episodes. Only one was provoked by a stranger. For most, the reactions
occurred immediately and without a noticeable prodromal pe-riod. Only one
subject stated that the outburst occurred between 1 and 24 hours after the
perceived provocation. All subjects with intermittent explosive disorder denied
that they intended the outburst to occur in advance. Most subjects remained
well oriented during the outbursts, although two claimed to lose track of where
they were. None lost control of urine or bowel function during the episode.
Subjects reported various degrees of subjective feelings of behavioral
dyscontrol. Only four felt that they completely lost control. Six had good
recollection of the event afterward, eight had partial recollection and one
lost memory of the event afterward. Most subjects with intermit-tent explosive
disorder attempted to help or comfort the victim afterwards.
Assessment
Special Issues in the Psychiatric Examination and History
The
DSM-IV-TR diagnosis of intermittent explosive disorder is essentially a
diagnosis of exclusion, and the psychiatrist should evaluate and carefully rule
out more common diagnoses that are associated with impulsive violence. The
lifelong nonremitting history of impulsive aggression associated with
antisocial person-ality disorder and borderline personality disorder, together
with other features of antisocial behavior (in antisocial personality disorder)
or impulsive behaviors in other spheres (in borderline personality disorder),
may distinguish them from intermittent explosive disorder, in which baseline
behavior and functioning are in marked contrast to the violent outbursts. Other
features of borderline personality disorder such as unstable and intense interpersonal
relationships, frantic efforts to avoid abandonment and identity disturbance
may also be elicited by a careful history. More than in most psychiatric
diagnoses, collateral information from an independent historian may be
extremely helpful. This is especially true in forensic settings. Of note,
patients with in-termittent explosive disorder are usually genuinely distressed
by their impulsive aggressive outbursts and may voluntarily seek psychiatric
help to control them. In contrast, patients with an-tisocial personality
disorder do not feel true remorse for their actions and view them as a problem
only insofar as they suffer their consequences, such as incarceration and
fines. Although patients with borderline personality disorder, like patients
with intermittent explosive disorder, are often distressed by their im-pulsive
actions, the rapid development of intense and unstable transference toward the
psychiatrist during the evaluation period of patients with borderline
personality disorder may be helpful in distinguishing it from intermittent
explosive disorder.
Other
causes of episodic impulsive aggression are sub-stance use disorders, in
particular alcohol abuse and intoxication. When the episodic impulsive
aggression is associated only with intoxication, intermittent explosive
disorder is ruled out. How-ever, as discussed earlier, intermittent explosive
disorder and al-cohol abuse may be related, and the diagnosis of one should
lead the psychiatrist to search for the other.
Neurological
conditions, such as dementias, focal frontal lesions, partial complex seizures
and postconcussion syndrome after recent head trauma, may all present as
episodic impulsive aggression and need to be differentiated from intermittent
explo-sive disorder. Other neurological causes of impulsive aggression include
encephalitis, brain abscess, normal-pressure hydrocepha-lus, subarachnoid
hemorrhage and stroke. In these instances, the diagnosis would be personality
change due to a general medical condition, aggressive type, and it may be made
with a careful his-tory and the characteristic physical and laboratory
findings.
Individuals
with intermittent explosive disorder may have comorbid mood disorders. Although
the diagnosis of a manic epi-sode excludes intermittent explosive disorder, the
evidence for serotonergic abnormalities in both major depressive disorder and
impulse control disorders supports the clinical observation that impulsive
aggression may be increased in depressed patients, leading ultimately to
completed suicide.
Physical Examination and Laboratory Findings
The
physical and laboratory findings relevant to the diagnosis of intermittent
explosive disorder and the differential diagnosis of impulsive aggression may
be divided into two main groups: those associated with episodic impulsive
aggression but not diagnostic of a particular disorder and those that suggest
the diagnosis of a psychiatric or medical disorder other than intermittent
explosive disorder. No laboratory or physical findings are specific for
inter-mittent explosive disorder.
The first
group of findings that are associated with impul-sive aggression across a
spectrum of disorders includes soft neuro-logical signs such as subtle
impairments in hand–eye coordination and minor reflex asymmetries. These signs
may be elicited by a comprehensive neurological examination and simple
pencil-and-paper tests such as parts A and B of the Trail Making Test.
Mea-sures of central serotonergic function such as CSF 5-HIAA lev-els, the
fenfluramine neuroendocrine challenge test, and positron emission tomography of
prefrontal metabolism also belong to this group. Although these measures
advanced our neurobiological understanding of impulsive aggression, their
utility in the diagno-sis of individual cases of intermittent explosive
disorder and other disorders with impulsive aggression is yet to be
demonstrated.
The
second group of physical and laboratory findings is useful in the diagnosis of
causes of impulsive aggression other than intermittent explosive disorder. The
smell of alcohol on a patient’s breath or a positive alcohol reading with a
Breathalyzer may help reveal alcohol intoxication. Blood and urine toxicology
screens may reveal the use of other substances, and track marks on the forearms
may suggest intravenous drug use. Partial com-plex seizures and focal brain
lesions may be evaluated by use of the EEG and brain imaging. In cases without
a grossly abnormal neurological examination, magnetic resonance imaging may be
more useful than computed tomography of the head. Magnetic resonance imaging
can reveal mesiotemporal scarring, which may be the only evidence for a latent
seizure disorder, sometimes in the presence of a normal or inconclusive EEG.
Diffuse slowing on the EEG is a nonspecific finding that is probably more
com-mon in, but not diagnostic of, patients with impulsive aggression.
Hypoglycemia, a rare cause of impulsive aggression, may be de-tected by blood
chemistry screens.
Differential Diagnosis
As
discussed earlier, the differential diagnosis of intermittent ex-plosive
disorder covers the differential diagnosis of impulsivity and aggressive
behavior in general. Aggression and impulsivity are defined as follows:
Aggression
is defined as forceful physical or verbal action, which may be appropriate and
self-protective or inappropriate as in hostile or destructive behavior. It may
be directed against another person, against the environment, or toward the
self. The psychiatric nosology of aggression is still preliminary. Impul-sivity
is defined as the tendency to act in a sudden, unpremedi-tated, and excessively
spontaneous fashion.
The
diagnosis of intermittent explosive disorder should be con-sidered only after
all other disorders that are associated with impulsivity and aggression have
been ruled out. Chronic impul-sivity and aggression may occur as part of a
cluster B person-ality disorder (antisocial and borderline); during the course
of substance use disorders and substance intoxication; in the setting of a
general medical (usually neurological) condition; and as part of disorders
first diagnosed during childhood and adolescence such as conduct disorder,
oppositional defiant disorder, attention-deficit/hyperactivity disorder and
mental retardation. In addition, impulsive aggression may appear during the
course of a mood disorder, especially during a manic episode, which precludes
the diagnosis of intermittent explosive disorder, and during the course of an
agitated depressive episode. Impulsive aggression may also be an associated
feature of schizophrenia, in which it may occur in response to hallucinations
or delusions. Impulsive aggression may also appear in variants of OCD, which
may pres-ent with concurrent impulsive and compulsive symptoms.
A special
problem in the differential diagnosis of impulsive aggression, which may arise
in forensic settings, is that it may rep-resent purposeful behavior. Purposeful
behavior is distinguished from intermittent explosive disorder by the presence
of motivation and gain in the aggressive act, such as monetary gain, vengeance,
or social dominance. Another diagnostic problem in forensic settings is
malingering, in which individuals may claim to have intermittent explosive
disorder to avoid legal responsibility for their acts.
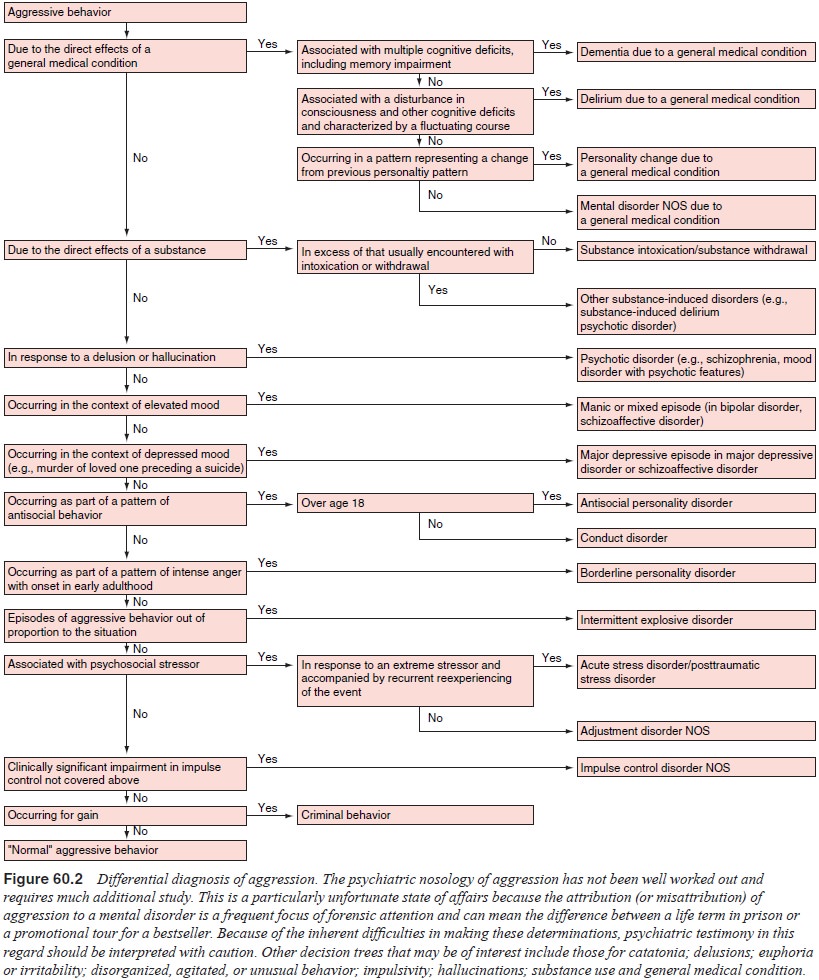
Figure
60.2 presents the differential diagnosis of aggression
Epidemiology
Prevalence and Incidence
Intermittent
explosive disorder has been subjected to little systematic study. The
exclusionary criterion in the DSM-IV-TR definition (criterion C) reflects an
ongoing debate over the boundaries of this disorder. In an early study of the
prevalence of DSM-III-R intermittent explosive disorder among violent men,
Felthous and colleagues (1991) found that of 443 sub-jects who complained of
violence, only 15 (3.4%) met crite-ria for intermittent explosive disorder.
However, the recently completed National Comorbidity Survey Replication (NCS-R)
(Kessler et al., 2005) found that
intermittent explosive disorder (12 month prevalence 2.6%) was as nearly common
as panic disorder (12 month prevalence 2.7%).
Comorbidity
The
DSM-IV-TR definition of intermittent explosive disorder allows signs of
generalized impulsivity or aggressiveness to be present between episodes. It
also allows the psychiatrist to give an additional diagnosis of intermittent
explosive disorder in the presence of another disorder if the episodes are not
better ac-counted for by the other disorder. The clinical reality is that most
individuals who have intermittent episodes of aggressive behavior also have
some impulsivity between episodes and often present with other past or current
psychiatric disorders. There is minimal research-based data available regarding
comorbidity. But the lit-erature on the comorbidity of impulsive aggressive
episodes sug-gests that it often occurs with three classes of disorders:
·
Personality disorders, especially antisocial
personality disor-der and borderline personality disorder. By definition,
antiso-cial personality disorder and borderline personality disorder are
chronic and include impulsive aggression as an essential feature. Therefore,
their diagnosis effectively excludes the di-agnosis of intermittent explosive
disorder (Figure 60.2).
·
A history of substance use disorders, especially
alcohol abuse. A concurrent diagnosis of substance intoxication excludes the
diagnosis of intermittent explosive disorder. However, many patients with
intermittent explosive disorder report past or family histories of substance
abuse, and in particular alcohol abuse. In light of evidence linking personal
and family history of alcohol abuse with impulsive aggression and the evidence
(reviewed later) linking both with low central serotonergic function, this
connection may be clinically relevant. There-fore, when there is evidence
suggesting that alcohol abuse may be present, a systematic evaluation of
intermittent explo-sive disorder is warranted, and vice versa.
·
Neurological disorders, especially severe head
trauma, partial complex seizures, dementias and inborn errors of metabolism.
Intermittent explosive disorder is not diagnosed if the aggres-sive episodes
are a direct physiological consequence of a gen-eral medical condition. Such
cases would be diagnosed as per sonality change due to a general medical
condition, delirium, or dementia. However, individuals with intermittent
explo-sive disorder often have nonspecific findings on neurologi-cal
examination, such as reflex asymmetries, mild hand–eye coordination deficits,
and childhood histories of head trauma with or without loss of consciousness.
Their EEGs may show nonspecific changes. Such isolated findings are com-patible
with the diagnosis of intermittent explosive disorder and preempt the diagnosis
only when they are indicative of a definitely diagnosable general medical or
neurological condi-tion. Such “soft” neurological signs may be diagnosed by a
full neurological examination and neuropsychological testing
McElroy
and coworkers (McElroy et al., 1998;
McElroy, 1999) studied 27 individuals who had symptoms that met criteria for
intermittent explosive disorder (IED) and reported: “Twenty-five (93%) subjects
had lifetime DSM-IV-TR diagnoses of mood disorders; 13 (48%), substance use
disorders; 13 (48%), anxiety disorders; 6 (22%), eating disorders; and 12
(44%), an impulse control disorder other than intermittent explosive disorder.
Sub-jects also displayed high rates of comorbid migraine headaches.
First-degree relatives displayed high rates of mood, substance use, and impulse
control disorders”.
Some
children with Tourette’s disorder may be prone to rage attacks. The clinical
manifestation of these rage attacks are similar to IED and may be more common
among children with To-urette’s who have comorbid mood disorders. On the basis
of these observations, the rage attacks of these children may flow from an
underlying dysregulation of brain function (Budman et al., 2000).
Course, Natural History and Prognosis
Little
systematic study has been done on the course of inter-mittent explosive
disorder. The onset of the disorder appears to be from late adolescence to the
third decade of life, and it may be abrupt and without a prodromal period.
Intermittent explosive disorder is apparently chronic and may persist well into
middle life unless treated successfully. In some cases, it may decrease in
severity or remit completely with old age.
Treatment
Given the
rarity of pure intermittent explosive disorder, it is not surprising that few
systematic data are available on its response to treatment and that some of the
recommended treatment ap-proaches to intermittent explosive disorder are based
on treat-ment studies of impulsivity and aggression in the setting of other
mental disorders and general medical conditions. Thus, no stan-dard regimen for
the treatment of intermittent explosive disorder can be recommended at this
time.
Psychological Treatment
Lion
(1992) has described the major psychotherapeutic task of teaching individuals
with intermittent explosive disorder how to recognize their own feeling states and
especially the affective state of rage. Lack of awareness of their own mounting
anger is presumed to lead to the build-up of intolerable rage that is then
discharged suddenly and inappropriately in a temper outburst. Patients with
intermittent explosive disorder are therefore taught how to first recognize and
then verbalize their anger appropri-ately. In addition, during the course of
insight-oriented psycho-therapy, they are encouraged to identify and express
the fantasies surrounding their rage. Group psychotherapy for temper-prone
patients has also been described. The cognitive–behavioral model of
psychological treatment may be usefully applied to problems with anger and rage
management.
Somatic Treatments
Several
classes of medications have been used to treat inter-mittent explosive
disorder. The same medications have also been used to treat impulsive
aggression in the context of other disorders. These included beta-blockers
(propranolol and meto-prolol), anticonvulsants (carbamazepine and valproic
acid), lithium, antidepressants (tricyclic antidepressants and serotonin
reuptake inhibitors) and antianxiety agents (lorazepam, alpra-zolam and
buspirone). Mattes (1990) compared the effectiveness of two commonly used
agents, carbamazepine and propranolol, for the treatment of rage outbursts in a
heterogeneous group of patients. He found that although carbamazepine and
propranolol were overall equally effective, carbamazepine was more effective in
patients with intermittent explosive disorder and propranolol was more
effective in patients with attention-deficit/hyperactiv-ity disorder. A
substantial body of evidence supports the use of propranolol – often in high
doses – for impulsive aggression in patients with chronic psychotic disorders
and mental retardation. Lithium has been shown to have antiaggressive
properties and may be used to control temper outbursts. In patients with
comor-bid major depressive disorder, OCD, or cluster B and C personal-ity
disorders, SSRIs may be useful. Overall, in the absence of more controlled
clinical trials, the best approach may be to tailor the psychopharmacological
agent to coexisting psychiatric co-morbidity. In the absence of comorbid
disorders, carbamazepine, titrated to antiepileptic blood levels, may be used
empirically.
Related Topics