Chapter: Clinical Cases in Anesthesia : Abruptio Placenta and Placenta Previa
How is fetal distress diagnosed?
How is fetal distress diagnosed?
Continuous electronic FHR monitoring was
developed, in the 1960s, to assess fetal well-being during labor. FHR
monitoring can be performed directly by placing an elec-trode on the fetal
scalp or indirectly by placing an ultra-sound probe on the maternal abdomen.
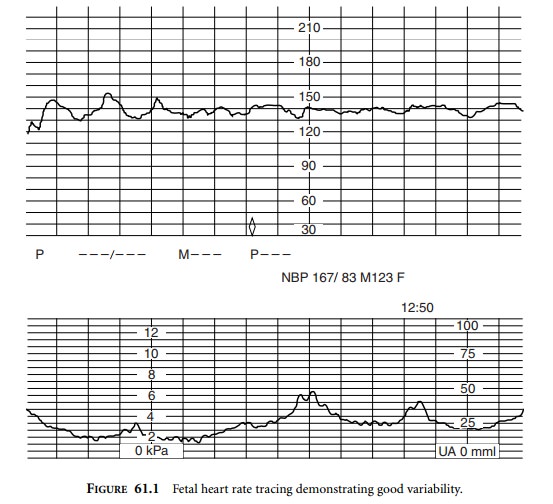
Characteristics of FHR patterns are divided into baseline and periodic
fea-tures. Baseline features include heart rate as well as vari-ability. In normal
labor, the FHR is determined by a balance between the sympathetic and
parasympathetic innervation of the fetal heart. Normal FHR is between 110 and
160 beats per minute (bpm). Variability of the FHR is very important in
determining fetal well-being. In normal labor there is beat-to-beat variability
(R-R interval) of about 3–5 bpm, and long-term periodic accelerations of 10–15
bpm lasting 10–15 seconds, occurring 3 or more times per 20 minute window
(Figure 61.1). FHR tracings demonstrating good beat-to-beat and long-term
variability are referred to as reactive tracings and imply normal neonatal
acid–base status, as assessed by a normal scalp pH (7.25–7.35). This is
associated with the delivery of a healthy and vigorous neonate, with Apgar
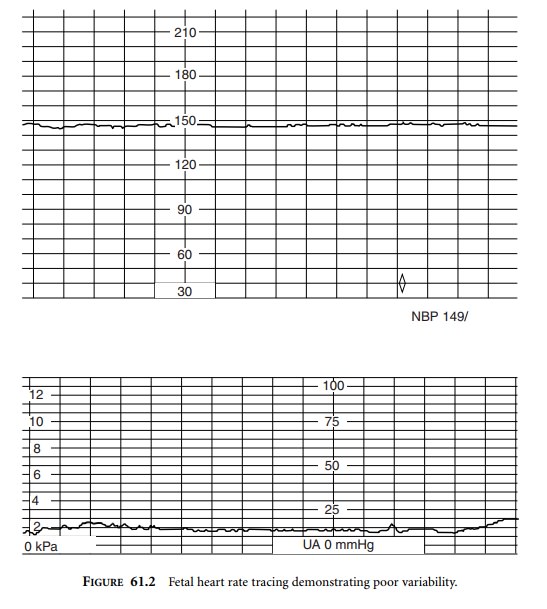
score ≥7 at 5 minutes. The absence of long-term and beat-to-beat
vari-ability may indicate fetal hypoxia (Figure 61.2).
The presence of good variability is the most sensitive indicator of fetal well-being. However, poor FHR variabil-ity is not always due to fetal hypoxia. Non-rapid eye move-ment fetal sleep cycles, lasting about 20 minutes, are the most common cause of poor variability. Congenital fetal heart disease, such as heart block, and fetal anencephaly are associated with poor FHR variability. Iatrogenic causes include the maternal administration of opioids, local anes-thetics, and atropine.
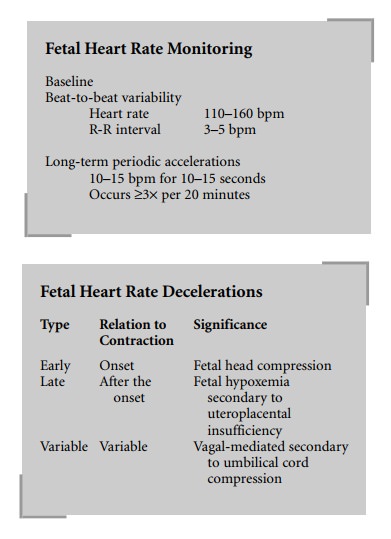
Early decelerations occur with the onset of the
contrac-tion and appear as a mirror image of the contraction. They are thought
to occur secondary to fetal head compression. They are accompanied by good
variability and are not associated with fetal hypoxia or acidosis.
Late decelerations are always associated with
fetal hypoxemia (Figure 61.3). In the presence of uteroplacental insufficiency
there is a significant decrease in fetal pO2 resulting in a
vagal-mediated slowing of the FHR. In inter-preting the significance of a late
deceleration, FHR vari-ability must be assessed. In the presence of good
variability significant neonatal cerebral hypoxia has not yet occurred and a
good neonatal outcome can be expected. If late decel-erations occur with poor
FHR variability, the tracing is more ominous. Fetal scalp blood sampling to
assess neo-natal acid–base status or immediate delivery is indicated.
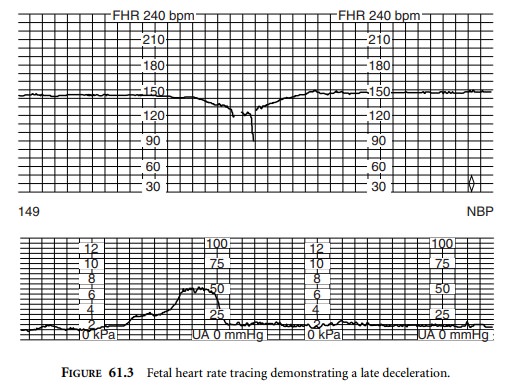
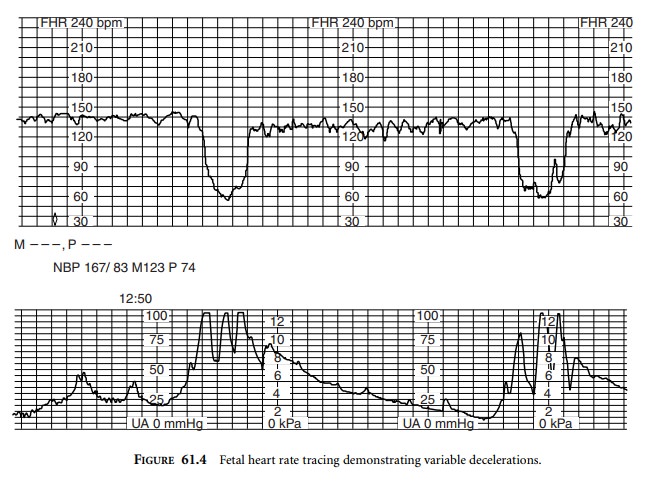
Variable decelerations are unrelated to the
time of onset of the uterine contraction (Figure 61.4). Variable decelerations
are due to a vagal-mediated reflex stimulated by umbilical cord compression.
Variable decelerations are considered severe if they last for more than 30
seconds with a nadir FHR of 60 bpm or less. Mild to moderate variable
decelerations are rarely associated with fetal hypoxia. However, severe and
recurrent decelerations may lead to the development of fetal hypoxia and
acidosis. In that case, the FHR tracing will also demonstrate loss of
variability. Fetal scalp blood sampling or immediate delivery may be indicated.
Fetal scalp blood sampling is performed when
the FHR tracing is indicative of fetal hypoxia and delivery is not immi-nent.
Scalp pH <7.20 is considered ominous and necessitates immediate delivery.
Fetal scalp stimulation, by digital exami-nation, may also be used to assess
fetal well-being. The pres-ence of fetal heart rate acceleration after scalp
stimulation is associated with a scalp pH above 7.20.
Intrapartum fetal pulse oximetry is a new
technology that may offer advantages over traditional monitoring techniques,
but is currently not widely used.
When a non-reassuring FHR tracing is
identified, in utero fetal resuscitation should commence. Correctable causes
include maternal hypotension, hyperstimulation of the uterus by pitocin, and
umbilical cord compression. Fetal well-being may be enhanced by administering
oxygen to the mother, improving left uterine displacement, and increasing
maternal blood pressure with either fluids or vasopressors.
Related Topics