Chapter: Clinical Cases in Anesthesia : Pheochromocytoma
How are patients with pheochromocytoma prepared for surgery?
How are
patients with pheochromocytoma prepared for surgery?
Mortality associated with pheochromocytoma
resection has been reduced from 20%, in reports 20 years ago, to 0–1% in recent
reports. There has been a similar reduction in reported major morbidity such as
myocardial infarction and stroke. This dramatic reduction probably represents
some publication bias, but is largely due to gradual pre-operative vasodilation
and intravascular volume repletion. Chronic exposure to norepinephrine produces
chronic vasoconstriction and hypovolemia. Rapid attempts to vasodilate and
restore intravascular volume can produce complications and may serve little
purpose. If the patient is not suffering from an acute hypertensive emergency,
it is best to allow for a more gradual correction of the volume status.
Outpatient administration of phenoxybenzamine,
an α-adrenergic blocking agent, has been the standard pre-operative
therapy for pheochromocytoma. The initial dose is approximately 20 mg/day, and
this is titrated gradually to control blood pressure. Common side-effects
include pos-tural hypotension and nasal stuffiness. Therapy often requires a
2-week period.
Phenoxybenzamine has two characteristics that
make it less than ideal. First, it is a nonselective α-blocker, so it prevents the α2-mediated inhibition of norepinephrine and epinephrine release.
Thus, most patients need simulta-neous β-adrenergic blockade. Phenoxybenzamine is also
a noncompetitive inhibitor that binds covalently. This causes more frequent and
more resistant postoperative hypo-tension than other alternative therapies.
Phenoxy-benzamine should be withheld for at least 12 hours before surgery.
Prazosin and doxazosin, selective α1-adrenergic
blockers, may be substituted for phenoxybenzamine. These are competitive
inhibitors with shorter half-lives, and cause less postoperative hypotension. Both
these drugs can be continued until the morning of surgery. Patients treated
with these agents usually do not require β-blockade, unless their tumor secretes
epinephrine or dopamine.
Treatment with calcium-channel blockers has
been advocated in several small published series and case
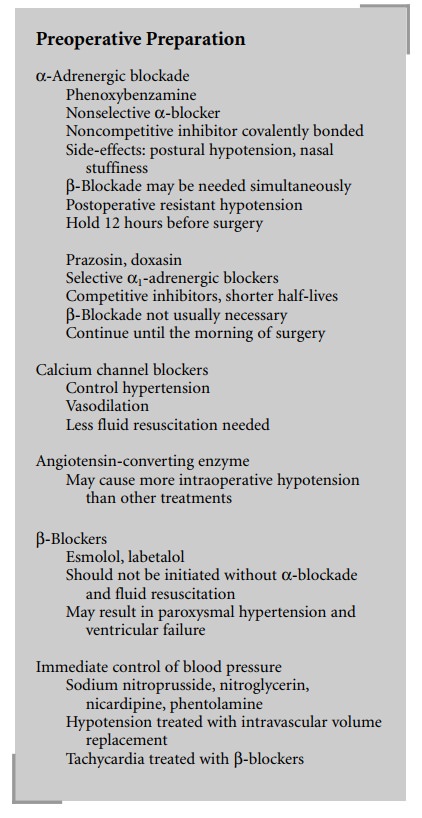
This treatment provides control of
hypertension and vasodilation, but may necessitate less fluid replace-ment and
cause less hypotension than treatment with phenoxybenzamine. With only small
studies, there is no strong evidence to recommend this over α-blockade.
Angiotensin-converting enzyme inhibitors have
also been used for preoperative blood pressure control and vasodilation. There
is no apparent benefit to using these agents, and they may cause more
intraoperative hypoten-sion than other treatment options.
Immediate control of systemic blood pressure
may be achieved for emergency cases through intravenous admin-istration of
vasodilators with a rapid onset and short dura-tion of action. Drugs that fit
this profile include sodium nitroprusside, nitroglycerin, nicardipine, and the
pure α-blocker phentolamine. Postural hypotension is treated with
intravascular volume repletion. A common side-effect of most of these
medications is tachycardia. The relative risk that tachycardia imposes on these
patients must be considered and potentially treated with intravenous β-blocking drugs.
Presently four β-blockers are available: esmolol, propranolol,
metoprolol, and labetalol. These drugs differ widely in their characteristics
and duration of action. Esmolol is β1-selective
and has a very short duration of action. Propranolol is intermediate in
duration but nonselective. While metoprolol is β1-selective,
it is perhaps too long-lasting to be useful in this condition. Labetalol is
nonselective in its β-blockade and has an additional beneficial
effect of mild α-blockade. β-Blockade should never be initiated before at
least partial α-blockade and intravascular resuscitation. β-Blockade with unopposed α-adrenergic stimulus can produce paroxysmal
hyperten-sion and acute left ventricular failure.
Related Topics