Chapter: Forensic Medicine: Head injuries
Head injuries
Head injuries
Introduction
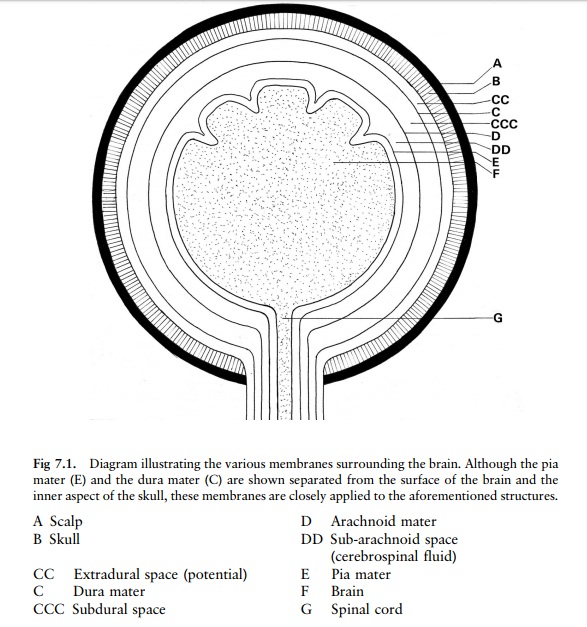
The brain, covered by three membranes
(meninges), is contained within the skull, which is covered by the scalp (fig
7.1). The innermost of the three membranes is known as the pia mater. This
membrane (rich in minute blood vessels) lies snugly against the surface of the
brain and follows the convolutions of the brain. There is a potential space
between the pia mater and the brain surface, which only becomes apparent when
haemorrhage occurs beneath the pia mater (fig 7.2).
The next membrane, which is thin and
transparent, contains no blood vessels.
It is called the arachnoid mater because it
resembles a spider web. Unlike the pia mater, it does not follow the
convolutions of the brain surface. The space between the surface of the brain
covered by the pia mater and the arachnoid mater is called the subarachnoid
space. It is filled with fluid known as the cerebrospinal fluid. This fluid
acts as a water cushion for the brain and the spinal cord.
The outermost of the three membranes is known as
the dura mater. It is a tough, relatively thick membrane which fits snugly
against the inner surface of the skull. The dura mater forms partitions which
separate and support various parts of the brain. It also forms venous channels
into which blood drains from the brain and then flows back through veins in the
neck to the heart.
There is a potential space between the outer
surface of the arachnoid mater and the inner surface of the dura mater (the
subdural space). Bridging veins are present in this space. There is also a
potential space between the dura mater and the overlying skull, called the extradural
or epidural space.
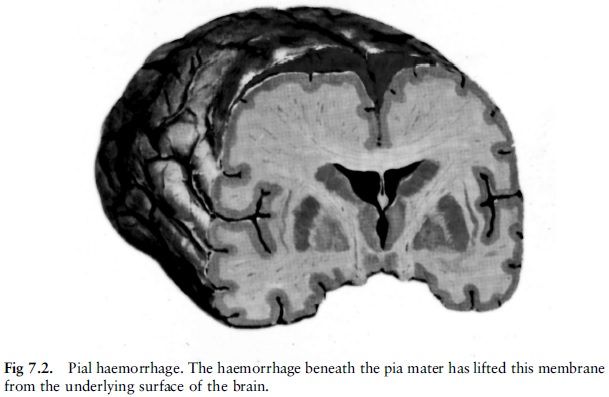
Arteries (meningeal arteries) run in grooves on
the inside of the skull, between the dura mater and the skull (fig 7.3). If the
head receives a blow, the force of the blow may injure the scalp as well as the
skull. If the skull fractures and the fracture involves a groove in which one
of these arteries is contained, the
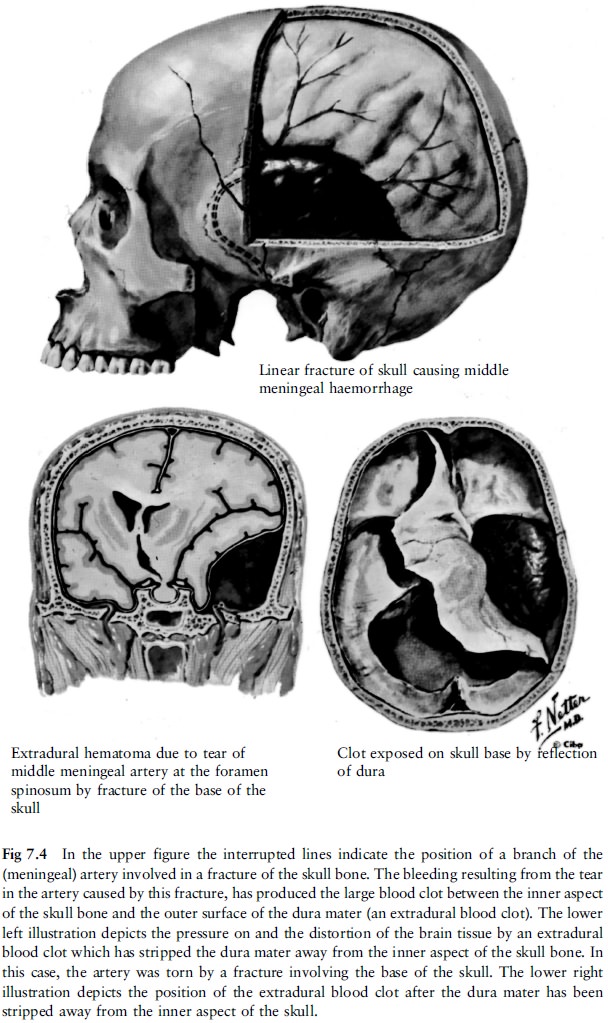
artery can rupture and start bleeding. An
arterial clot can form and can grow to a considerable size between the inside
of the skull and the outside of the dura mater. The latter can tear off from
the inner surface of the skull (fig 7.4).
Because this clot lies on the outside of the
dura mater, it is known as an extradural blood clot (haematoma). Because it
forms in the rigid skull, it will press on and distort the brain and its
connections, often with fatal results.
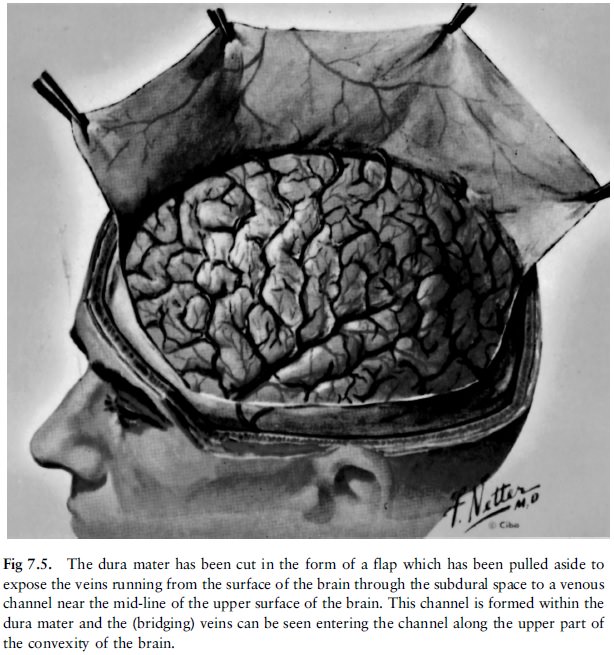
The veins draining the blood from the brain pass
from the brain's surface through the subarachnoid and subdural spaces to the
sinuses (venous channels) in the dura mater (fig 7.5). These are the so-called
bridging veins which bridge the space between the surface of the brain and the
venous channels in the dura mater into which they empty. If a bridging vein
ruptures in the subdural space, a venous blood clot (haematoma) will form and
grow in size in the subdural space between the external surface of the
arachnoid mater and the internal surface of the dura mater (fig 7.6, 7.7). A
subdural haemorrhage due to a rupture of one of these bridging veins may result
from a fracture of the skull which involves the subdural vessels.
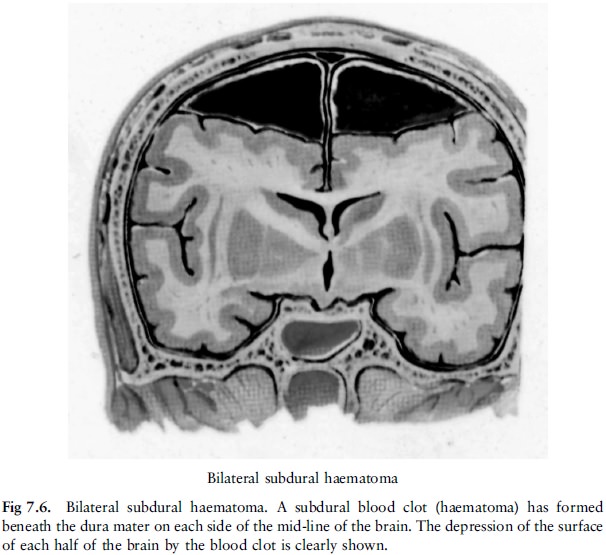
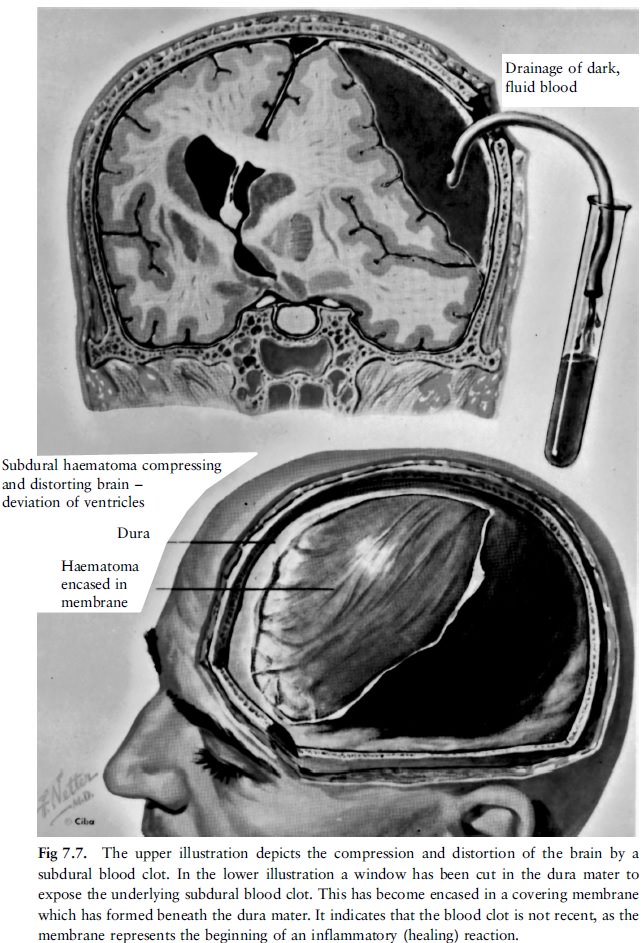
A blow on the head (without fracturing the skull) may, however, because of a sudden rotation of the head, cause the brain to swirl, so that the bridging veins in the subdural space are stretched to such an extent that they tear. A subdural blood clot can thus form without a fracture of the skull. Such a blood clot can also press on and distort the brain and its connections, with a fatal outcome if the condition is not relieved timeously.
By the mechanisms already described the bridging
veins passing through the subarachnoid space on their way to the venous sinuses
in the dura mater, can also be torn, producing subarachnoid haemorrhages.
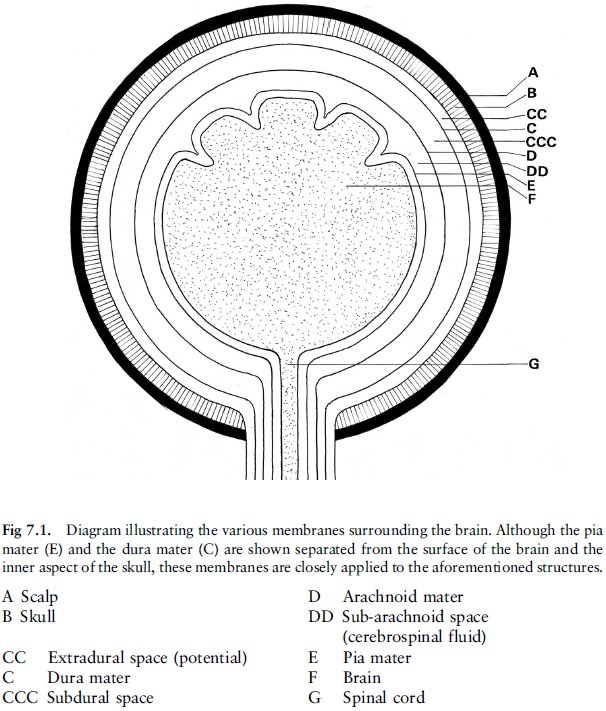
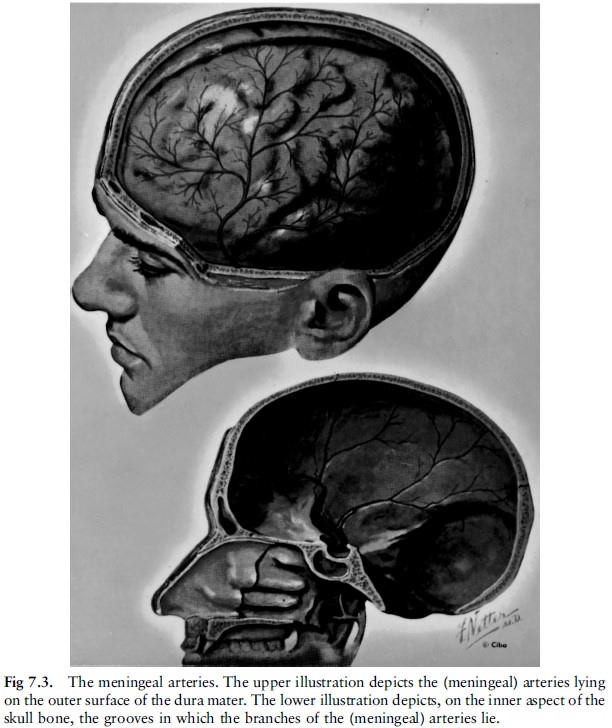
Haemorrhages on the surface of the brain caused
by a blow on the head, are called pial or subpial haemorrhages. They form
immediately beneath the pia mater.
A hard blow to the head can therefore produce
wounds of the scalp as well as bruises in and beneath the scalp. These injuries
may or may not be associated with fractures of the skull. The skull fractures,
in turn, may or may not be associated with extradural, subdural, subarachnoid
and pial or subpial haemorrhages. If the blow is strong enough or if portions
of the fractured skull are driven into the brain, there may also be
haemorrhages deep inside the brain (fig 7.8).

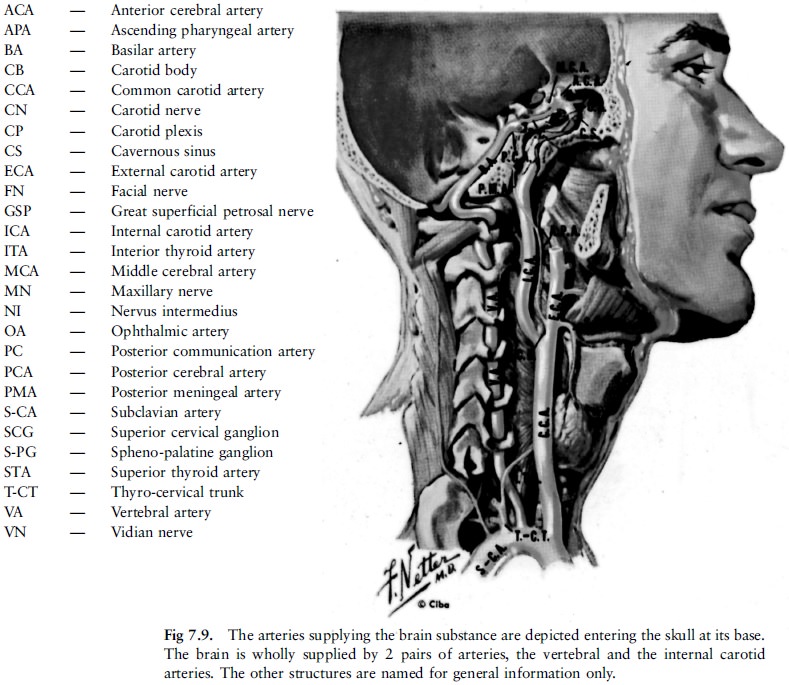
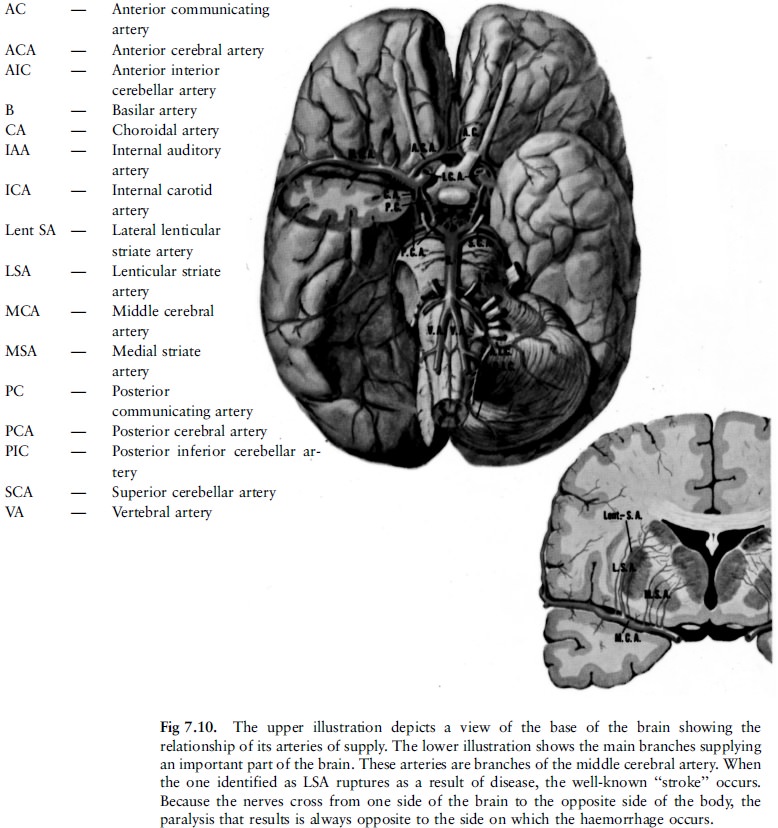
The brain itself is supplied by arteries which
enter it at its base (fig 7.9, 7.10). The arteries in the brain can undergo
degenerative changes, especially in the elderly (with or without associated
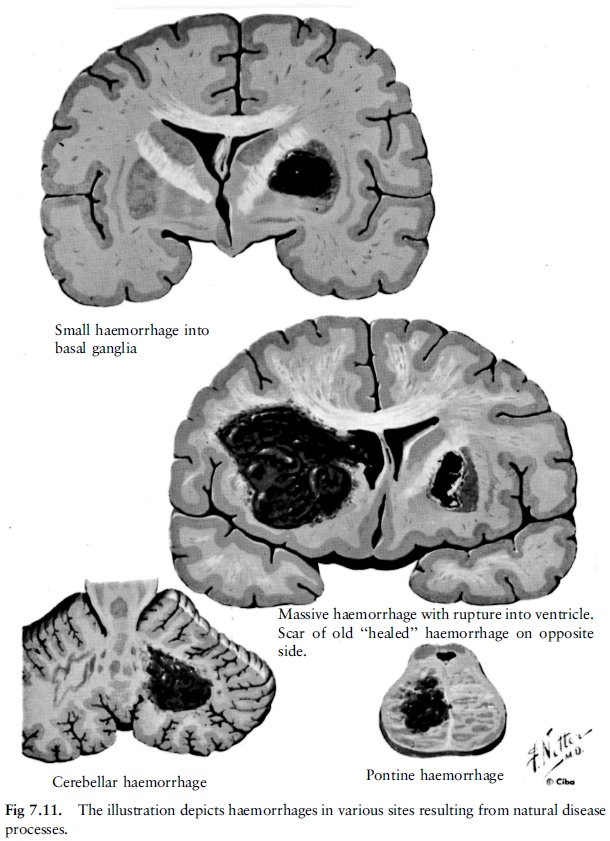
high blood pressure), causing them to rupture. This produces extensive
haemorrhage in the brain substance, known as a stroke. This type of stroke is
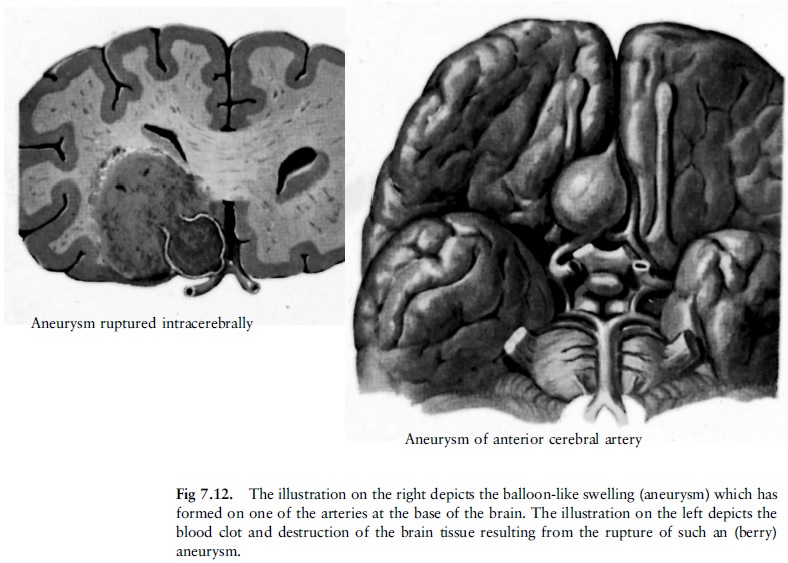
more likely to occur in the elderly (fig 7.11). Abnormalities of the arteries
at or near the base of the brain (in the subarachnoid space) can weaken the
arterial walls. At these weak spots the wall balloons outwards in a berry-like
fashion, called a berry aneurysm (fig 7.12). A berry aneurysm can rupture
spontaneously, producing an extensive arterial subarachnoid haemorrhage that
can spread from the base of the brain upwards along the sides of the brain in
the subarachnoid space.
If one of these berry aneurysms forms on a
branch of an artery in the deeper parts of the brain, this rupture will produce
a haemorrhage in the substance of the brain (fig 7.12). Rupture of a berry
aneurysm occurs in a younger age-group.
Injury to the head following vehicle and industrial accidents, assaults, and firearm wounding is a very common cause of death and of long-term morbidity and disability, and frequently becomes a demanding medico-legal issue in both criminal prosecutions and civil actions and in disciplinary hearings.
The unique anatomy of the scalp, skull, and intra-cranial structures influence the nature and consequences of wounding following the application of force. This force can be applied directly or transmitted to the head along the vertebral column, for example after falling from a height and then landing upright on the feet. Although there is enough space in the skull to permit differential movement between skull and brain, the skull is relatively rigid and the brain only just fits into the three skull compartments. Therefore the brain can only attempt, to a limited degree, to compensate for an increase in its own size, such as occurs with cerebral oedema or haemorrhage into the substance of the brain. This is done by the displacement of fluid from the ventricles of the brain before increasing intra-cranial pressure interferes with the circulation of blood through the brain causing further cerebral oedema and displacement (herniation) of portions of brain tissue from one compartment to another of the cranium or downward into the foramen magnum (a big opening in the base of the skull), further impeding brain function. Increased pressure between the brain and the encasing skull from a space-occupying mass such as a haemorrhage, can in turn cause the fatal cycle of cerebral ischaemia, anoxic cerebral cellular changes, cerebral oedema and further ischaemic changes. (Ischaemia is the term used to describe a deficiency of blood in a body part.)
Neurones (nerve cells) are particularly
susceptible to diminished oxygen supply, whatever the cause, and the ensuing
cellular damage is soon irreversible. The different specialised neurones have
different oxygen requirements. Hence ``recovery'' from a general period of
cerebral ischaemia (or any other cause of general anoxia) can be accompanied by
changes in cerebral function ranging from the most subtle of personality or
behavioural changes to epileptic seizures or gross defects expressed clinically
as widespread paralysis, and death, all of this depending on the extent and duration
of the oxygen deprivation.
Brain damage can also result from the direct effects of projectiles, knives, or bone fragments being driven into the substance of the brain.
This may cause the disruption of tissues due to
ensuing haemorrhage or subsequent infection in the underlying structures via
breaches in the covering tissues. Linear fractures of the base of the skull,
even in the absence of any wound in the overlying skin, may involve an air
sinus (the term ``sinus'' means a hollow space), where potentially pathogenic
bacteria (frequently resident in these sinuses) may readily pass to the
underlying linings (meninges) of the brain and, in their new and more
favourable breeding environment, cause meningitis (inflammation of the
meninges) or an abscess.
The consequences of the rapid acceleration of the head on the vertebral pivot as a result of some force as compared with the result of the application of that same force to a head that is still, may differ greatly. In the former case there is usually an immediate disturbance of neuronal function followed by loss of consciousness. In the latter case extensive damage to the scalp and skull may not be accompanied by immediate loss of consciousness and the patient may be able to recall events up to the time of injury and relate them before lapsing into unconsciousness as a result of the delayed effects of the injury.
The function of nerve cells is affected not only
by trauma and its consequences but also equally dramatically and often
similarly by a variety of therapeutic drugs, the abuse of drugs, natural
disease processes such as diabetes, and primary and secondary spreading of
cancerous tumours of the brain. Many of these conditions can be caused by a
fall, a motor-vehicle accident, or assault, and can add to the diagnostic
problem, namely to determine what caused the specific clinical picture.
The effects of alcoholic intoxication can
closely resemble a post-concussional state, and that the two cannot be easily
differentiated, has been a bitter lesson taught by experience; the answer is to
keep the patient under observation. This is particularly problematic when a
person was involved in an accident and apprehended for driving under the influence
of alcohol. Many people have died because a treatable head injury was confused
with intoxication. It happened that a driver once, after having been carefully
medically examined for ``driving under the influence'', was subsequently taken
into custody. One hour later the driver was seen to be ``sleeping'' deeply by
someone who had returned to the cells on an unrelated matter. An examination
revealed blood-stained fluid issuing from his ear - a sign of a possible fracture of the base of
the skull. The person was immediately transferred to a neurosurgical ward and
an emergency operation to evacuate an acute extradural haemorrhage was
successful. The blood-alcohol concentration was also far in excess of the
statutory level. This was thus a case where the suspect appeared to be ``under
the influence'' when he was apprehended, but had previously sustained
intracranial bleeding, which only presented later.
Certain prescription medications to inhibit
blood clotting, chronic alcohol-ism, and cerebral atrophy, can considerably
increase the effect of even a trivial force to the head and thus the risk of
brain injury. The fact that even in the most serious brain injuries there might
be no outwardly visible evidence of violence, compounds the problems of the
medical practitioner. Furthermore, clinical manifestation of brain damage may
only appear many hours after the injury was sustained; this is often the case with
a subdural haemorrhage. Or such a haemorrhage may follow a lucid interval
subsequent to a period of unconsciousness due to concussion; during the period
of lucidity the victim appears to have recovered from the effects of the
injury.
It is these very real problems, especially in a
busy hospital trauma unit, which raise the question whether all head-injury
patients (except those with very minor head injuries) should not undergo X-rays
of the skull, or other more sophisticated investigations. No wonder, then, that
Bernard Knight (1996) one of the best-known medico-legal authors, a
barrister-at-law and consultant pathologist, is of the opinion that head
injuries ``constitute one of the most difficult problems in the realms of
accident medicine both from the technical and medico-legal points of view. Many
actions for negligence have arisen from failure to view head injuries with
sufficient concern. The doctor's procedure when dealing with a head injury must
be coloured by his regard not only for his patients' welfare but also for
possible medico-legal complications at a later date. Even if he considered that
the clinical state does not warrant further investigation, it is most unwise to
proceed other than with the greatest caution.''
In hospital practice, one of the most important
facts to be determined is whether the patient was unconscious for any period of
time, however short. If it is likely that this was the case, it would be most
unwise to discharge the patient. Wherever possible, the patient should be admitted
for at least 24 hours so that the onset of symptoms and signs of a latent
condition such as a sub- or extradural haemorrhage can be observed. These
conditions are usually readily remediable if the diagnosis is made timeously.
It is customary to issue a ``head-injury warning card'' to a patient's relative
or friend to inform the person of what action to take should the patient's
condition deteriorate after discharge. It would serve little purpose to issue
such a card to the patient himself, who may not be in a position to respond to
such a warning, should the need arise. It must also be remembered that an X-ray
of the head will only indicate fractures. Brain injury may be present even
though there is no fracture. Special investigations, such as a CT-scan, will be
required to diagnose this. However, it is not always practical to perform this.