Chapter: Maternal and Child Health Nursing : Prenatal Care
General examination of the ante-natal patients
General examination of the
ante-natal patients
The
general examination of the ante-natal patient is embarked upon after the
routine examinations have been completed. These are as follows:
The blood
pressure is checked and recorded, the weight and height are estimated and
documented, the urinalysis is checked and findings are noted and recorded. Any
abnormal finding is reported to the doctor and investigation of such
abnormality is done and necessary treatment accorded.
Preparation
Ensure
patient empties her bladder, Create some privacy by screening the patient,
Explain procedure to the patient, Patient removes all her clothes and
underwears, she then covers up with a wrapper or a sheet, the patient lies on
the couch in a dorsal position, the midwife communicates with her in an
understanding language and friendly approach that promotes adequate relaxation.
Procedure
Examination
is done by observing the patient from head to toes =appearance, gait, posture,
complexion.
The Head
Is
examined to note personal cleanliness, presence of dandruff and lice, untidy
hair-do, Abnormal swelling.
The Eyes: are observed for inflammation,
discharge, pallor,abnormal growth, and infection.
The Ears
They are
examined for: the location, the number, equality, cleanliness, abnormal
discharge and abnormal contour.
The Nose
The nose
is observed to note the size and shape and to detect:
discharge,
disease and abnormality.
The month
The lips
are examined for pallor: dryness, cracks and sores.
The mouth
is observed for bad breath and angular stomatities. The teeth are
examined for the
shape. dental hygiene
or sores, the tongue is examined for pallor dryness,
coatedness, sores
The face
The
countenance of the face is examined for puffiness which may be due to anemia,
malnutrition, chronic nephritis, nephrotic syndrome, pre-exlampsia.
The Neck
This is
observed for previous scar. It is palpated for any growth, distended jugular
veins, enlarged lymph glands
The Upper limbs
The upper
limbs are checked for:equality, abnormality.
The hands
are examined for: pallor and puffiness which can be elicited through a
handshake with the patient. The fingers are examined for shape, size, pallor,
abnormality and puffiness especially around the ring finger if she wears one.
The nail beds are also examined for pallor.
The
patient now assumes a sitting up position for the examination of the breasts.
The breasts
These are
first inspected for Shape, size, equality, cleanliness, abnormality, changes
due to pregnancy such as enlargement, pigmentation of primary areola, Montgomery
tubercules, appearance of secondary areola, visible engorged veins, The nipples
are examined for the shape, size,protactility.
The ducts
are tested for patency by expressing the breast fluid
Palpation
The
breast are each palpated. Any feeling of undue lump or irregular mass should be
reported to the doctor.
Advice
The
patient is advised on the Care of the breast which focus on
(a) The Diet: The type of food she should take
must be rich inprotein such as eggs, beans, fish meat, melon. minerals and
vitamins such as green vegetables, carrots eggs, fruits with plenty of fluids.
The quality of breast milk produced will depend on the quality of good intake.
(bBreast Hygiene: She is advised to pay
particular attention to breast care during bath times. The nipples should be
washed with soft cloth or cotton wool and mild soap.
They are
pulled out and later rolled between the thumb and index finger to get them
toughened the nipples are then dried firmly with a soft towel and little oil
such as kernel oil or olive oil is rubbed on them to soften them and prevent
crust formation.
(c)Expression of colostrums: Colostrums
is expressed from thebreasts from the 34th week of pregnancy in
order to maintain the potency of the ducts and thereby preventing breast engorgement
in the puerperium.
(d)Breast Support: She is
educated on the need to keep thebreasts well supported with good, adjustable,
firm, cotton material, wide strapped brassier which is large enough to
accommodate the breasts during the progressive enlargement of the breast.
The Back: While the woman is still in a
sitting up position, herback is examined for detection of – curvature of sp ine
e.g. scoliosis kyphosis, abnormal swelling e.g. lymphoma, lateral protrusion of
the abdomen as in case of multiple pregnancy. Sacral oedema and other
abnormalities such as spinal bifida occur.
The
patient is later told to lie back on the couch with the midwife assisting her,
so as to examine the abdomen.
The lower limbs
These are
examined for cleanliness: Athlete’s foot and foot drop, equality of legs and
toes, curvature of legs, pallor of the soles of feet, varicosity of the legs.
Each leg
is lifted up the fingers of the right hand are run under the posterior aspect
of the leg and thigh to confirm or exclude varicosity. Simultaneously, the
vulva is viewed quickly to note. Oedema, Varicose veins, excessive and
unhealthy vaginal discharge, warts, hair follicle infection, bleeding.
The
patient is then interviewed if she has any undue vaginal irritation or purulent
vaginal discharge.
To
demonstrate the presence of oedema in the ankle, the right thumb is pressed
against the pre-tibial area and quickly run over the pressed area to elicit any
pitting.
The
general examination is now completed and the woman dresses up. She is commended
where necessary and she enquires for clarification of any existing problem.
Patients
with abnormal findings are referred, All findings are recorded in the patients
ante-natal notes, Routine drugs are given e.g. (haematinics and antimalaria),
Appointment is given for the next visit and a thorough explanation is outlined
to this effect.
Investigations
Blood test – Hb estimation at booking, 28 –
32 weeks and after 36weeks before labour. More frequently if there is
abnormality. PCV, FBC are also checked. Rhesus factor genotype and blood group
are determined. Others are wasser man’s Khan test. VDRL, HIV.
Urinalysis: Test urine for glucose, albumin,
acetone. Furtherlaboratory test may be done if there are abnormalities
detected.If Rhesus positive antibody titre is checked at booking, 28, 32, 36
and before labour starts.
Vaginal
Examination is done at book or at least once during pregnancy. May be done
early for the following, - to diagnose pregnancy, exclude pelvic tumor, to
determine gestational age before 16 weeks.
X-ray may
be required to ascertain maturity Ultrasound scan
Doctor
may do pelvic assessment on all primigravidae between 36-38 weeks.
Abdominal examination
Aims: To observe signs of pregnancy,
to assess fetal sign andgrowth, To assess fetal health, to detect any deviation
from normal, to diagnose the location of fetal parts.
Preparation:
1.
Ensure that patient empties her bladder
2.
Let the patient lie in the supine position on the
couch, with one pillow under her head. Her arms should be by her sides to
prevent traction of abdominal muscles.
3.
Draw the screen in order to ensure privacy.
4.
Talk to the patient nicely to aid relaxation.
5.
The examiner’s arms and hands should be relaxed.
Three
ways of obtaining information required are: - Inspection, palpation,
Auscultation
Inspection: note the size and shape of the
abdomen
a. Size: Should correspond with the
supposed period of gestation.
If much
larger or smaller:-
·
Review the date of the last normal menses
·
Note the size of the patient. If dates are correct
but uterus is large, possibilities are: multiple pregnancy, polyhydramnios, a
large fetus, a fetus plus uterine fibroid.
b. Shape: Should be longitudinally ovoid.
This is clear in mostprimigravidae.
Round: is due to multiparity, transverse
lie, obesity,polyhydramnios.
In
addition to the above, note on inspection: Pigmentation, scars, striae
gravidarum, The quality of the muscles of abdomen and the contour.
c. Fetal Movement: This is
evidence that the fetus is alive. It alsoaids in the diagnosis of position as
the back will be on the opposite side where movement is seen.
d. Contour of the abdomen: (a)
Normal is dome –shape (b)Pendulous abdomen is common with multigravid woman.
(c) when lightening has taken place the uterus sag forward and uterus is more
prominent e.g. when standing. (d) Depression at the umbilical level suggest
occipito posterior (e) skin-scar, stiae gravidarum, Linea Nigera are observed.
Palpation;
Aim
·
To observe signs of pregnancy. To determine fundal
height Size and growth of the fetus. This should correspond with the period of
gestation.
·
To ascertain fetal parts of the fetus is in
different parts of the uterus, also the lie and attitude of the fetus.
·
Relationship of presenting part to the pelvis: how
to palpate the uterus. Detect any deviation from normal.
The hands
should be clean and warm, cold hands do not have necessary acute sense of touch
and tend to induce contraction of the abdominal muscles. Arms and hands should
be relaxed and the pads NOT THE TIPS of the fingers are used with delicate
precision moving smoothly over the abdomen without lifting them. Erratic and
sudden pressure and rough manipulation are irritating and can cause
contractions making detection of fetal parts impossible.
Abdominal
palpation is done by the following maneuvers: (though not by mean the order)
·
Estimation of fundal height
·
Fundal palpation – To determine the part of the fet
us in the fundus.
·
Lateral palpation
·
Pelvic palpation (lower pole palpation)
Fundal height:
Method: The ulnar border of the left hand
is placed at theupper border of the fundus in order to locate the highest point
of the fundus. As many fingers of the left, hand as can be accommodated are
laid flat between the upper border of the fundus and the xiphisternum. The
distance between fundus and xiphisternum is estimated in fingers breadth. At 36
weeks gestation no fingers can be inserted.
Using MC
Donald’s technique – A measuring tape tha t has centimeter is used. After
locating the fundal height, the zero end of the tape is paced on the symphysis
pubic and stretched to the height of fundus. The measurement on the tape is
recorded as the fundal height. It is more accurate between 20-31 weeks
gestation.
Fundal palpation: This
manoeuvre will help to determinewhether the presentation is cephalic or breech
and the lie longitudinal or transverse. In 95% of cases the breech will be in
the fundus and this denotes a cephalic presentation. When the head is in the
fundus, the presentation is breech. While facing the woman’s head “walk” up
both hands, one o n either side of the uterus and lay them flat on the fundus
of the uterus to feel what is lying there.
Lateral Palpation: This
maneuver is useful to locate thefetal back as an aid to diagnosis of position.
Method: while still facing the patient’s
head or feet, thehands are placed on both sides of the uterus at about
umbilical level. Pressure is applied with the palms of alternate hands to
differentiate the degree of resistance between the two sides of the uterus. One
hand is used to steady the uterus and press the fetus over towards the
examining hand which determines the presence of the broad resistant back or the
small parts that slip under the examining fingers.
By using
a rotary movement of the fingers:
·
The back may be mapped out as a continuous smooth
resistant mass from the breech down to the neck.
·
The limbs are noted as small irregularities which
are often felt to move.
Pelvic palpation: This is
the most important maneuver inabdominal palpation because of its value in the
diagnosis of presentation of the fetus, engagement of its fetal head and
disproportion between head and pelvis. It should not cause discomfort to the
women.
Method: The midwife stands on the
patient’s right with herthighs against the couch, her body, turned at the
waist, facing towards the women’s feet. Using both hands, the midwife finds out
what is in the lower pole of the uterus as follows:
The sides
of the uterus, just below the umbilical level are grasped snugly between the
palms of the hands, the fingers held close together, pointing downwards and
inwards. What ever is in the lower pole can then be held between both hands. In
most cases it is the head that is in the lower pole and is recongised as
follows:
·
It is smooth, round and hard.
·
It is ballotable (if not engaged).
·
It is separated from the trunk by a groove (the
neck)
Occasionally
it is the breech; which is
·
Less hard
·
More irregular
·
The lower limbs are nearer to it.
Pawlik’s grip
This
method of palpating the lower pole of the uterus is most effective when the
head is not engaged.
Method: The midwife, standing on the
patient’s right, faces thewoman’s head and using the right hand, grasps the
lower pole of
the
uterus with the thumb on the woman’s right side and the fingers on the left
side of the uterus. Fingers and thumb must be sufficiently far apart to
accommodate the fetal head.
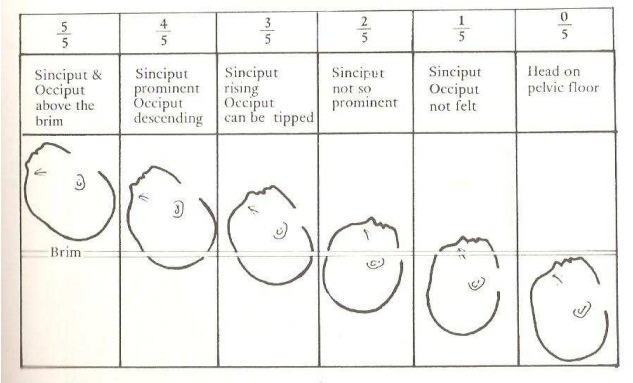
Engagement of the head
Definition
Engagement
means when the widest diameter of the presenting part has passed through the
pelvic brim. In some women engagement does not take place before term. In some
African women it occurs during the first stage of labour.
Recognition of engagement
·
The head or breech is not mobile
·
Less of the head will be felt per abdomen
Auscultation
The fetal
heart sounds are like the ticking of a watch under a pillow. The rate may be
double that of the mother’s heart beast observed at the wrist. About 140 beat
per minute.
Procedure
Place
Pinard’s stethoscope over the back of the fetus and support with the pinna of
the ear while the right hand feels maternal pulse at her wrist.
NOTE: All information obtained must be considered
in making diagnosis. If any information does not correspond, repeat and think
again.
Head fitting
From the
36 week onwards, it is essential to assess the pelvic capacity in every
pregnant woman. In a normal pelvic brim inclination of 600 the head
should engage from 36 week, but in some African women with pelvic inclination
of over 80 the head does not engage until labour has been in progress for some
hours.
The following methods of assessments are considered
1. Sitting the patient up.
Ensure
that the bladder is empty while patient lies on the couch, grasp the fetal head
with the right hand as in pawlik’s grip. Rest the ulna border of the examining
hand, with the 4th and last fingers on the symphysis pubis. The
woman is asked to sit up without assistant and to lean forwards for a short
time. Her diaphragm and abdominal muscles tend to press the fetus downwards.
The thumb, index and middle fingers feel the head go through the pelvis. Any
overlap (which is suggestive of cephalo – pelvic disproportion will be felt by
the fingers on the symphysis pubis)
2. With the Patient Standing: Let the
patient stand up with herfeet slightly apart. Face her and grasp fetal head
gently. Let her lean forward slightly holding the edge of the couch with both
hands. Push the head backward and downward gently. The titled pelvis makes the
entry through the pelvic brim ‘direct’ in the absence of cephalo -pelvic
disproportion.
Related Topics