Chapter: Medical Physiology: General Principles of Gastrointestinal Function- Motility, Nervous Control, and Blood Circulation
Gastrointestinal Blood Flow- ÔÇťSplanchnic CirculationÔÇŁ
Gastrointestinal Blood Flow- ÔÇťSplanchnic CirculationÔÇŁ
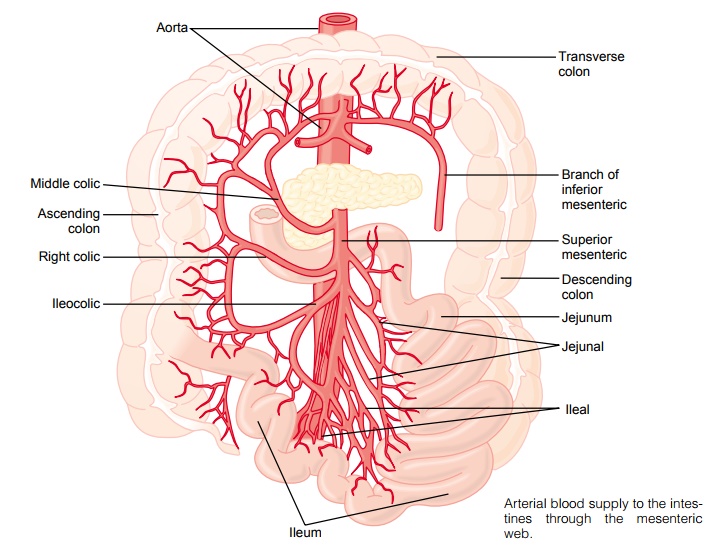
The blood vessels of the gastrointestinal system are part of a more extensive system called the splanchniccirculation, shown in Figure 62ÔÇô6. It includes the bloodflow through the gut itself plus blood flows through the spleen, pancreas, and liver. The design of this system is such that all the blood that courses through the gut, spleen, and pancreas then flows immediately into the liver by way of the portal vein. In the liver, the blood passes through millions of minute liver sinusoids and finally leaves the liver by way of hepatic veins that empty into the vena cava of the general circulation. This flow of blood through the liver, before it empties into the vena cava, allows the reticuloendothelial cells that line the liver sinusoids to remove bacteria and other particulate matter that might enter the blood from the gastrointestinal tract, thus preventing direct transport of potentially harmful agents into the remainder of the body.
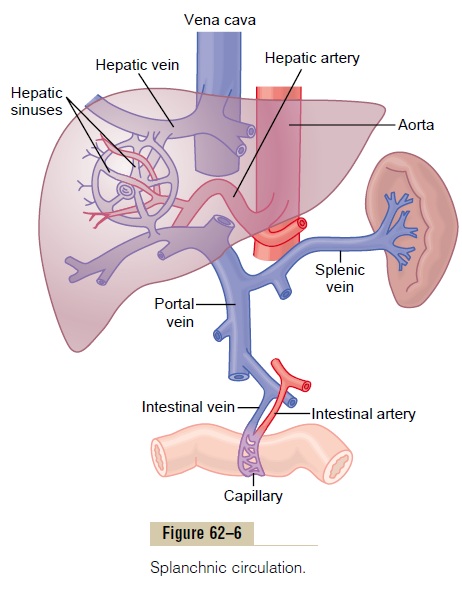
The nonfat, water-soluble nutrients absorbed from the gut (such as carbohydrates and proteins) are trans-ported in the portal venous blood to the same liver sinusoids. Here, both the reticuloendothelial cells and the principal parenchymal cells of the liver, the hepaticcells, absorb and store temporarily from one half tothree quarters of the nutrients. Also, much chemical intermediary processing of these nutrients occurs in the liver cells. Almost all of the fats absorbed from the intestinal tract are not carried in the portal blood but instead are absorbed into theintestinal lymphatics and then conducted to the sys-temic circulating blood by way of the thoracic duct, bypassing the liver.
Anatomy of the Gastrointestinal Blood Supply
Figure 62ÔÇô7 shows the general plan of the arterial blood supply to the gut, including the superior mesen-teric and inferior mesenteric arteries supplying the walls of the small and large intestines by way of an arching arterial system. Not shown in the figure is the celiac artery, which provides a similar blood supply to the stomach.
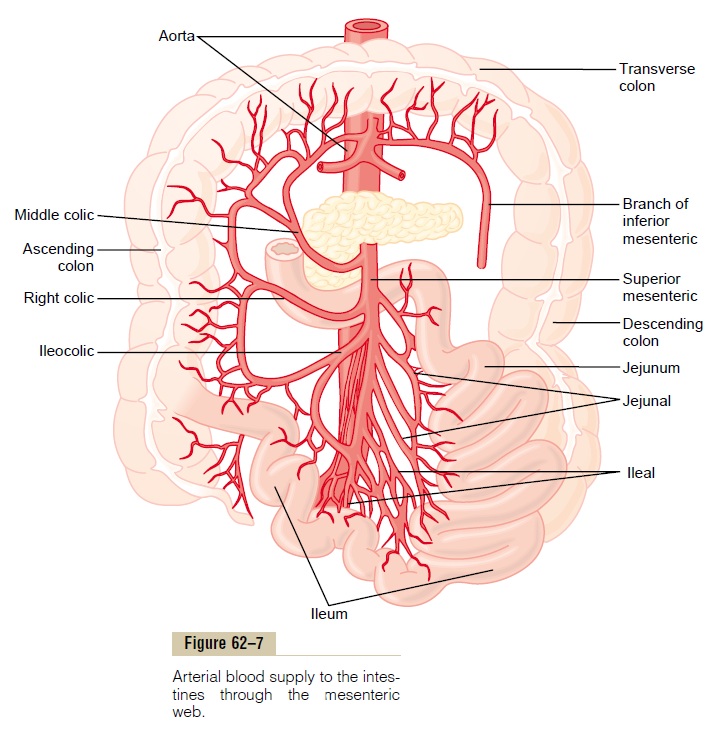
On entering the wall of the gut, the arteries branch and send smaller arteries circling in both directions around the gut, with the tips of these arteries meeting on the side of the gut wall opposite the mesenteric attachment. From the circling arteries, still much smaller arteries penetrate into the intestinal wall and spread (1) along the muscle bundles, (2) into the intes-tinal villi, and (3) into submucosal vessels beneath the epithelium to serve the secretory and absorptive functions of the gut.
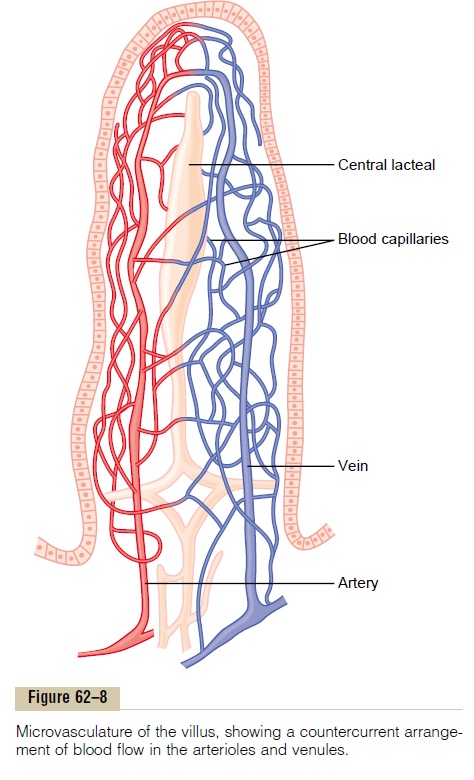
Figure 62ÔÇô8 shows the special organization of the blood flow through an intestinal villus, including a small arteriole and venule that interconnect with a system of multiple looping capillaries. The walls of the arterioles are highly muscular and are highly active in controlling villus blood flow.
Effect of Gut Activity and Metabolic Factors on Gastrointestinal Blood Flow
Under normal conditions, the blood flow in each area of the gastrointestinal tract, as well as in each layer of the gut wall, is directly related to the level of local activity. For instance, during active absorption of nutri-ents, blood flow in the villi and adjacent regions of the submucosa is increased as much as eightfold. Likewise, blood flow in the muscle layers of the intestinal wall increases with increased motor activity in the gut. For instance, after a meal, the motor activity, secretory activity, and absorptive activity all increase; likewise, the blood flow increases greatly but then decreases back to the resting level over another 2 to 4 hours.
Possible Causes of the Increased Blood Flow During Gastroin-testinal Activity. Although the precise cause or causesof the increased blood flow during increased gastroin-testinal activity are still unclear, some facts are known.
First, several vasodilator substances are released from the mucosa of the intestinal tract during the digestive process. Most of these are peptide hormones, including cholecystokinin,vasoactive intestinal peptide, gastrin, and secretin. These same hormones controlspecific motor and secretory activities of the gut.
Second, some of the gastrointestinal glands also release into the gut wall two kinins, kallidin and bradykinin, at the same time that they secrete theirsecretions into the lumen. These kinins are powerful vasodilators that are believed to cause much of the increased mucosal vasodilation that occurs along with secretion.
Third, decreased oxygen concentration in the gut wall can increase intestinal blood flow at least 50 to 100 per cent; therefore, the increased mucosal and gut wall metabolic rate during gut activity probably lowers the oxygen concentration enough to cause much of the vasodilation. The decrease in oxygen can also lead to as much as a fourfold increase of adenosine, a well-known vasodilator that could be responsible for much of the increased flow.
Thus, the increased blood flow during increased gas-trointestinal activity is probably a combination of many of the aforementioned factors plus still others yet undiscovered.
ÔÇťCountercurrentÔÇŁ Blood Flow in the Villi. Note in Figure62ÔÇô8 that the arterial flow into the villus and the venous flow out of the villus are in directions opposite to each other, and that the vessels lie in close apposi-tion to each other. Because of this vascular arrange-ment, much of the blood oxygen diffuses out of the arterioles directly into the adjacent venules without ever being carried in the blood to the tips of the villi. As much as 80 per cent of the oxygen may take this short-circuit route and therefore not be available for local metabolic functions of the villi. The reader will recognize that this type of countercurrent mechanism in the villi is analogous to the countercurrent mecha-nism in the vasa recta of the kidney medulla.
Under normal conditions, this shunting of oxygen from the arterioles to the venules is not harmful to the villi, but in disease conditions in which blood flow to the gut becomes greatly curtailed, such as in circula-tory shock, the oxygen deficit in the tips of the villi can become so great that the villus tip or even the whole villus suffers ischemic death and can disintegrate. Therefore, for this reason and others, in many gas-trointestinal diseases the villi become seriously blunted, leading to greatly diminished intestinal absorptive capacity.
Nervous Control of Gastrointestinal Blood Flow
Stimulation of the parasympathetic nerves going to the stomach and lower colon increases local blood flow atthe same time that it increases glandular secretion. This increased flow probably results secondarily from the increased glandular activity and not as a direct effect of the nervous stimulation.
Sympathetic stimulation, by contrast, has a direct effect on essentially all the gastrointestinal tract to cause intense vasoconstriction of the arterioles with greatly decreased blood flow. After a few minutes of this vasoconstriction, the flow often returns almost to normal by means of a mechanism called ÔÇťautoregula-tory escape.ÔÇŁ That is, the local metabolic vasodilator mechanisms that are elicited by ischemia become pre-potent over the sympathetic vasoconstriction and, therefore, redilate the arterioles, thus causing return of necessary nutrient blood flow to the gastrointestinal glands and muscle.
Importance of Nervous Depression of Gastrointestinal Blood Flow When Other Parts of the Body Need Extra Blood Flow. Amajor value of sympathetic vasoconstriction in the gut is that it allows shut-off of gastrointestinal and other splanchnic blood flow for short periods of time during heavy exercise, when increased flow is needed by the skeletal muscle and heart. Also, in circulatory shock, when all the bodyÔÇÖs vital tissues are in danger of cel-lular death for lack of blood flowÔÇöespecially the brain and the heartÔÇösympathetic stimulation can decrease splanchnic blood flow to very little for many hours.
Sympathetic stimulation also causes strong vaso-constriction of the large-volume intestinal and mesen-teric veins. This decreases the volume of these veins,thereby displacing large amounts of blood into other parts of the circulation. In hemorrhagic shock or other states of low blood volume, this mechanism can provide as much as 200 to 400 milliliters of extra blood to sustain the general circulation.
Related Topics