Chapter: Introduction to Human Nutrition: Food Safety: A Public Health Issue of Growing Importance
Food-borne viruses
Food-borne viruses
It is only in recent years that the role of viruses as etiological agents of food-borne illness have emerged. Difficulties in attributing viral illness to food have mainly been due to the diagnostic difficulties in detecting viruses in an implicated food and under-reporting owing to the mild nature of illness in many cases. A report from the US Centers for Disease Control (CDC) in 2000, on surveillance of food-borne disease outbreaks from 1993 to 1997, revealed that viruses accounted for 6% of all food-borne out-breaks and 8% of cases. Hepatitis A accounted for the majority of these, followed by norovirus. Data pub-lished by the European Food Safety Authority (EFSA) revealed that viruses accounted for 10.2% of all food-borne outbreaks reported during 2006. Caliciviruses (including norovirus) accounted for the majority (61.7%) of these food-borne viral outbreaks.
Food-borne viruses are generally enteric, being transmitted by the fecal–oral route. However, trans-mission by person-to-person contact and via con-taminated water is common. Hepatitis A and norovirus are more commonly transmitted via foods than other food-borne viruses. The most important food-borne viruses are hepatitis A, norovirus, astrovirus, and rotavirus. These are discussed in detail below.
Hepatitis A virus
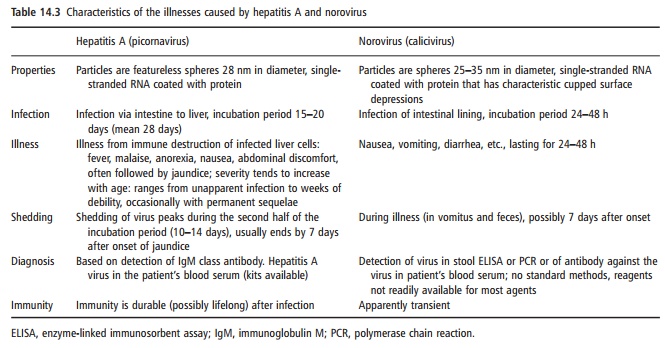
Hepatitis A is one of the more severe food-borne diseases. The illness results from immune destruction of infected liver cells, and a few weeks of debility are common (Table 14.3). It is a member of the picornaviruses.
Infections are more likely to be asymptomatic or mild in young children than in adolescents or adults. The virus can be shed in feces for up to 14 days before the onset of illness. It is therefore possible for an infected food handler with poor personal hygiene (hand-washing, in particular) to contaminate food during this period. The virus may be shed in the feces for 1–2 weeks after onset of symptoms.
Food becomes contaminated with this virus via infected persons or via fecally contaminated water, as is usual with shellfish. Examples of other foods impli-cated in hepatitis A outbreaks are oysters, raw mussels, drinking water, bakery products and caviar. Hepatitis A has been shown to be more heat resistant than most enteric viruses and is also quite resistant to drying. The virus is susceptible to chlorination treatment, however, and water-borne hepatitis A outbreaks have been linked to untreated water.
Noroviruses
Norovirus was the first enteric virus reported to be food-borne. It was formerly known as Norwalk-like virus (NLV) or small round structured virus (SRSV) and has recently been classified as a member of the calicivirus family. Noroviruses are difficult to detect, especially from foods.
Exposure is by contact with infected individuals or fecally contaminated water or other materials. Shell-fish (bivalve molluscs) have been the predominant food vehicle. Shellfish beds may frequently become contaminated with human feces from sewage dis-charges. Aerosolization of vomitus-containing virus particles has been proposed as another mode of trans-mission of the virus and may also be a source of food contamination. Sensitive detection assays have now revealed that shedding of the virus in feces may con-tinue for up to a week after the illness subsides.
Astroviruses
Under the electron microscope, astroviruses appear as small, round viruses that have surface projections resembling a five- or six-pointed star (Greek astron, star). The illness differs from the norovirus in that the incubation period is longer (3–4 days), the duration of illness is longer (often lasting for 7–14 days), and vomiting is less common, with diarrhea being the predominant symptom. In addition, the very young (<1 year) appear to be the most susceptible group, whereas norovirus affects all age groups. Astrovirus outbreaks have been reported to occur in crèches, schools, hospital wards, and nursing homes, but in many cases there was no well-defined mode of trans-mission. One large outbreak linked to contaminated food from a common supplier occurred in Osaka, Japan, in 1991, affecting 4700 teachers and pupils from 14 schools in the city.
Rotaviruses
Serogroup A rotaviruses are the single most impor-tant cause of infantile gastroenteritis worldwide, affecting an estimated 130 million infants and causing 873 000 deaths every year. The rotavirus genome consists of 11 segments of double-stranded RNA surrounded by a double-shelled viral capsid. When examined by electron microscopy, the double-shelled particles resemble a wheel-like structure morphologi-cally (Latin rota, wheel). The incubation period of the illness is 1–3 days, and the illness is characterized by fever, vomiting, and diarrhea. Although the majority of rotavirus infections involve infants, outbreaks of food-borne, and water-borne disease affecting all age groups have been reported, albeit infrequently.
Other viruses
Picornaviruses other than hepatitis A can also be transmitted by the food-borne route. Polioviruses are transmitted by food but virulent strains of this agent are now extremely rare. Coxsackie virus and echovi-rus have been associated with food-borne outbreaks, but data are limited. Hepatitis E has been linked to a number of water-borne outbreaks but there has been no association with food. One food-borne outbreak of parvovirus linked to consumption of cockles has been reported.
Related Topics