Chapter: Medical Surgical Nursing: Health Care Delivery and Nursing Practice
Expanded Nursing Roles
Expanded Nursing Roles
Professional nursing is
adapting to meet changing health needs and expectations. One such adaptation is
through the expanded role of the nurse, which has developed in response to the
need to improve the distribution of health care services and to decrease the
cost of health care. NPs, clinical nurse specialists (CNSs), cer-tified
nurse-midwives, and certified registered nurse anesthetists are identified as
advanced practice nurses. The nurse who func-tions in an advanced practice role
provides direct care to patients through independent practice, practice within
a health care agency, or collaboration with a physician. Specialization has
evolved within the expanded roles of nursing as a result of the recent
explosion of technology and knowledge.
Nurses may receive
advanced education in such specialties as family, critical care, coronary care,
respiratory care, oncologic care, maternal and child health care, neonatal
intensive care, rehabili-tation, trauma, rural health, and gerontologic
nursing, to name just a few. With the expanded role of the nurse, various
titles have emerged that attempt to specify the functions as well as the
edu-cational preparation of nurses, although functions are less distinct than
in previous years. In medical-surgical nursing, the most sig-nificant of these
titles arenurse practitioner and clinical nurse spe-cialist, and the more
recent title of advanced practice nurse, whichencompasses
both NPs and CNSs.
Initially the
educational preparation for NPs was in certificate programs. Most states now
require both NPs and CNSs to have a graduate-level education. The two programs,
which originally differed significantly in scope and in their definition of
role com-ponents, now have many similarities and areas of overlap.
NPs are, for the most
part, prepared as generalists (eg, pediatric NP, geriatric NP). They define
their role in terms of direct provi-sion of a broad range of primary health
care services to patients and families. The focus is on providing primary
health care to patients and collaborating with other health professionals. NPs
practice in both acute and nonacute care settings. The 1997 Balanced Budget Act
provided for NPs to receive direct Medicare reimbursement. In addition, in some
states—and with new legislation possibly nationwide—NPs have prescriptive
authority (Boyd, 2000).
CNSs, on the other hand,
are prepared as specialists who prac-tice within a circumscribed area of care
(eg, cardiovascular CNS, oncology CNS). They define their role as having five
major com-ponents: clinical practice, education, management, consultation, and
research. Studies have shown that in reality the CNS focus is often on the
education and consultation roles: education and counseling of patients and
families and education, counseling, and consultation with nursing staff. Some
states have granted CNSs prescriptive authority if they have the required
educational preparation. CNSs practice in a variety of settings, including the
community and the home, although most practice in acute care settings.
Recently, CNSs have been identified by many nursing leaders as ideal case
managers. They have the educational back-ground and the clinical expertise to
organize and coordinate ser-vices and resources to meet the patient’s health
care needs in a cost-effective and efficient manner.
With advanced practice
roles has come a continuing effort by professional nursing organizations to
define more clearly the practice of nursing. Nurse practice acts have been
amended to give nurses the authority to perform functions that were previ-ously
restricted to the practice of medicine. These functions in-clude diagnosis
(nursing), treatment, performance of selected invasive procedures, and
prescription of medications and treat-ments. The board of nursing in each state
stipulates regulations regarding these functions. The board defines the
education and experience required and determines the clinical situations in
which a nurse may perform these functions.
In general, initial
care, ambulatory health care, and anticipa-tory guidance are all becoming
increasingly important in nursing practice. Advanced practice roles enable
nurses to function inter-dependently with other health care professionals and
to establish a more collegial relationship with physicians. As changes in
health care continue, the role of advanced practice nurses, especially in
primary care settings, is expected to increase in terms of scope,
re-sponsibility, and recognition.
COLLABORATIVE PRACTICE
Throughout this we have
explored the changing role of nursing. Many references have been made to the
significance of the nurse as a member of the health care team. As the unique
competencies of nurses are becoming more clearly articulated, there is
increasing evidence that nurses provide certain health care services distinct
to the profession. However, nursing continues to recognize the importance of collaboration
with other health care disciplines in meeting the needs of patients.
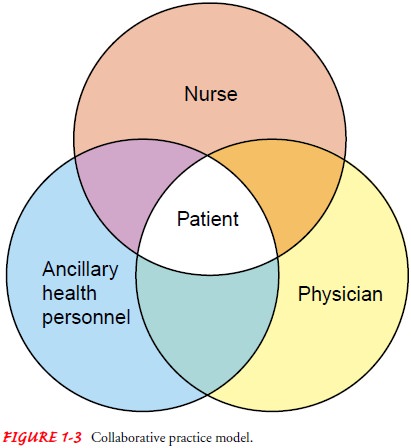
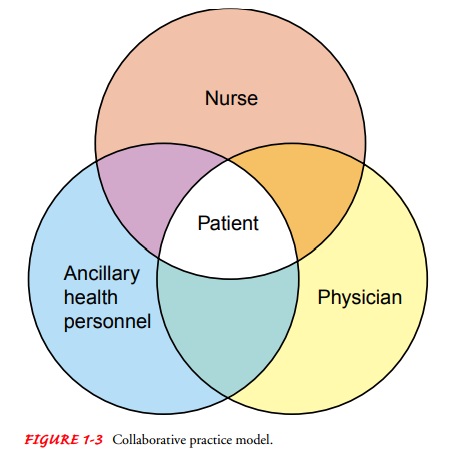
Some institutions use
the collaborative practice model (Fig. 1-3). Nurses, physicians, and ancillary
health personnel function within a decentralized organizational structure,
collaboratively making clinical decisions. A joint practice committee, with
rep-resentation from all care providers, may function at the unit level to
monitor, support, and foster collaboration. Collaborative prac-tice is further
enhanced with integration of the clinical record and with joint patient care
record reviews.
The collaborative model,
or a variation of it, should be a primary goal for nursing—a venture that
promotes shared participation, re-sponsibility, and accountability in a health
care environment that is striving to meet the complex health care needs of the
public.
Related Topics