Chapter: Psychiatric Mental Health Nursing : Eating Disorders
Etiology - Eating Disorders
ETIOLOGY
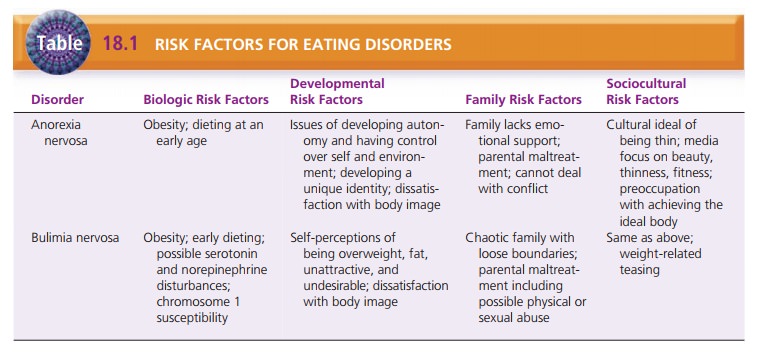
A specific cause for eating disorders is unknown. Initially,
dieting may be the stimulus that leads to their development. Biologic
vulnerability, developmental problems, and family and social influences can
turn dieting into an eating disor-der (Table 18.1). Psychologic and physiologic
reinforcement of maladaptive eating behavior sustains the cycle (Anderson &
Yager, 2005).
Biologic Factors
Studies of anorexia nervosa and bulimia nervosa have shown that
these disorders tend to run in families. Genetic vulnerability also might
result from a particular personal-ity type or a general susceptibility to
psychiatric disorders. Or it may directly involve a dysfunction of the
hypothala-mus. A family history of mood or anxiety disorders (e.g.,
obsessive–compulsive disorder) places a person at risk for an eating disorder
(Anderson & Yager, 2005).
Disruptions of the nuclei of the hypothalamus may pro-duce many of
the symptoms of eating disorders. Two sets of nuclei are particularly important
in many aspects of hunger and satiety
(satisfaction of appetite): the lateral hypothalamus and the ventromedial
hypothalamus. Defi-cits in the lateral hypothalamus result in decreased eating
and decreased responses to sensory stimuli that are impor-tant to eating.
Disruption of the ventromedial hypothala-mus leads to excessive eating, weight
gain, and decreased responsiveness to the satiety effects of glucose, which are
behaviors seen in bulimia.
Many neurochemical changes accompany eating dis-orders, but it is
difficult to tell whether they cause or result from eating disorders and the
characteristic symp-toms of starvation, binging, and purging. For example,
norepinephrine levels rise normally in response to eating, allowing the body to
metabolize and to use nutrients. Norepinephrine levels do not rise during
starvation, however, because few nutrients are available to metabo-lize.
Therefore, low norepinephrine levels are seen in clients during periods of
restricted food intake. Also, low epinephrine levels are related to the
decreased heart rate and blood pressure seen in clients with anorexia.
Increased levels of the neurotransmitter serotonin and its
precursor tryptophan have been linked with increased satiety. Low levels of
serotonin as well as low platelet levels of monoamine oxidase have been found
in clients with bulimia and the binge and purge subtype of anorexia ner-vosa
(Anderson & Yager, 2005); this may explain binging behavior. The positive
response of some clients with buli-mia to treatment with selective serotonin
reuptake inhibi-tor antidepressants supports the idea that serotonin levels at
the synapse may be low in these client
Developmental Factors
Two essential tasks of adolescence are the struggle to develop
autonomy and the establishment of a unique iden-tity. Autonomy, or exerting
control over oneself and the environment, may be difficult in families that are
overpro-tective or in which enmeshment
(lack of clear role bound-aries) exists. Such families do not support members’
efforts to gain independence, and teenagers may feel as though they have little
or no control over their lives. They begin to control their eating through severe
dieting and thus gain control over their weight. Losing weight becomes
reinforc-ing: by continuing to lose, these clients exert control over one
aspect of their lives.
It is important to identify potential risk factors for developing
eating disorders so that prevention programs can target those at greatest risk.
Adolescent girls who express body dissatisfaction are most likely to experience
adverse outcomes, such as emotional eating, binge eating, abnormal attitudes
about eating and weight, low self-esteem, stress, and depression.
Characteristics of those who developed an eating disorder included disturbed
eat-ing habits; disturbed attitudes toward food; eating in secret;
preoccupation with food, eating, shape, or weight; fear of losing control over
eating; and wanting to have a completely empty stomach (Cave, 2009).
The need to develop a unique identity, or a sense of who one is as
a person, is another essential task of adolescence. It coincides with the onset
of puberty, which initiates many emotional and physiologic changes. Self-doubt
and confu-sion can result if the adolescent does not measure up to the person
she or he wants to be.
Advertisements, magazines, and movies that feature thin models
reinforce the cultural belief that slimness is attractive. Excessive dieting
and weight loss may be the way an adolescent chooses to achieve this ideal. Body image is how a person perceives his or her body, that is, a mental self-image. For most people,
body image is consis-tent with how others view them. For people with anorexia
nervosa, however, body image differs greatly from the per-ception of others.
They perceive themselves as fat, unattractive, and undesirable even when they
are severely underweight and malnourished. Body
image disturbance occurs when there is an extreme discrepancy between one’s
body image and the perceptions of others and extreme dissatisfaction with one’s
body image.
Self-perceptions of the body can influence the devel-opment of
identity in adolescence greatly and often per-sist into adulthood.
Self-perceptions that include being overweight lead to the belief that dieting
is necessary before one can be happy or satisfied. Clients with bulimia nervosa
report dissatisfaction with their bodies as well as the belief that they are
fat, unattractive, and undesirable. The binging and purging cycle of bulimia
can begin at any time—after dieting has been unsuccessful, before the severe
dieting begins, or at the same time as part of a “weight loss plan.”
Family Influences
Girls growing up amid family problems and abuse are at higher risk
for both anorexia and bulimia. Disordered eating is a common response to family
discord. Girls growing up in families without emotional support often try to
escape their ![]()
![]() negative emotions. They place an intense focus
outward on something concrete: physical appearance. Disordered eating becomes a
distraction from emotions.
negative emotions. They place an intense focus
outward on something concrete: physical appearance. Disordered eating becomes a
distraction from emotions.
Childhood adversity has been identified as a significant risk
factor in the development of problems with eating or weight in adolescence or
early adulthood. Adversity is defined as physical neglect, sexual abuse, or
parental mal-treatment that includes little care, affection, and empathy as
well as excessive paternal control, unfriendliness, or overprotectiveness.
Sociocultural Factors
In the United States and other Western countries, the media fuels
the image of the “ideal woman” as thin. The culture equates beauty,
desirability, and, ultimately, hap-piness with being very thin, perfectly
toned, and physi-cally fit. Adolescents often idealize actresses and models as
having the perfect “look” or body even though many of these celebrities are
underweight or use special effects to appear thinner than they are. Books,
magazines, dietary supplements, exercise equipment, plastic surgery advertisements,
and weight loss programs abound; the dieting industry is a billion-dollar
business. The culture considers being overweight a sign of laziness, lack of
self-control, or indifference; it equates pursuit of the “perfect” body with
beauty, desirability, success, and will power. Thus, many women speak of being
“good” when they stick to their diet and “bad” when they eat desserts or
snacks.
Pressure from others also may contribute to eating dis-orders.
Pressure from coaches, parents, and peers and the emphasis placed on body form
in sports such as gymnas-tics, ballet, and wrestling can promote eating
disorders in athletes. Parental concern over a girl’s weight and teasing from
parents or peers reinforces a girl’s body dissatisfac-tion and her need to diet
or control eating in some way. Studies in the United States and Europe conclude
that bul-lying and peer harassment are also related to an increase in
disordered eating habits (Eisenberg & Neumark-Sztainer, 2008; Sweetingham
& Walter, 2008).
Related Topics