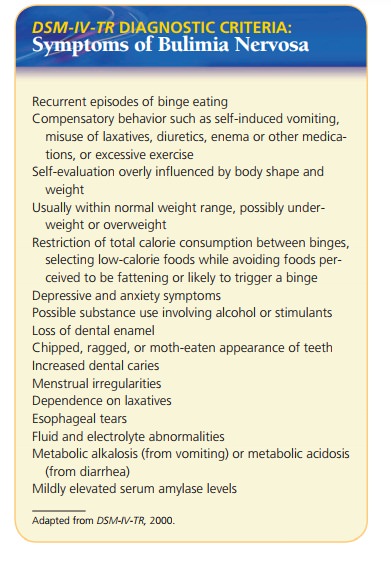
Chapter: Psychiatric Mental Health Nursing : Eating Disorders
Bulimia - Eating Disorders
BULIMIA
Onset and Clinical Course
Bulimia nervosa usually begins in late adolescence or early
adulthood; 18 or 19 years is the typical age of onset. Binge eating frequently
begins during or after dieting. Between binging and purging episodes, clients
may eat restrictively, choosing salads and other low-calorie foods. This
restric-tive eating effectively sets them up for the next episode of binging
and purging, and the cycle continues.
Clients with bulimia are aware that their eating behav-ior is
pathologic and go to great lengths to hide it from others. They may store food
in their cars, desks, or secret locations around the house. They may drive from
one fast-food restaurant to another, ordering a normal amount of food at each
but stopping at six places in 1 or 2 hours. Such patterns may exist for years
until family or friends discover the client’s behavior or until medical
complica-tions develop for which the client seeks treatment.
Follow-up studies with clients with bulimia show that 10 years
after treatment, 30% continued to engage in recurrent binge eating and purging
behaviors, whereas 38% to 47% were fully recovered (Anderson & Yager,
2005). One third of fully recovered clients relapse. Clients with a comorbid
personality disorder tend to have poorer outcomes than those without.
The death rate from bulimia is estimated at 3% or less.
Most clients with bulimia are treated on an outpatient basis. Hospital
admission is indicated if binging and purg-ing behaviors are out of control and
the client’s medical status is compromised. Most clients with bulimia have
near-normal weight, which reduces the concern about severe malnutrition—a
factor in clients with anorexia nervosa.
Treatment and Prognosis
Cognitive–Behavioral Therapy
CBT has been found to be the most effective treatment for bulimia.
This outpatient approach often requires a detailed manual to guide treatment.
Strategies designed to change the client’s thinking (cognition) and actions
(behavior) about food focus on interrupting the cycle of dieting, bing-ing, and
purging and altering dysfunctional thoughts and beliefs about food, weight,
body image, and overall self-concept. CBT enhanced with assertiveness training
and self-esteem enhancement has produced positive results (Schmidt et al.,
2007).
Psychopharmacology
Since the 1980s, several controlled studies have been conducted to
evaluate the effectiveness of antidepres-sants to treat bulimia. Drugs, such as
desipramine (Nor-pramin), imipramine (Tofranil), amitriptyline (Elavil),
nortriptyline (Pamelor), phenelzine (Nardil), and fluox-etine (Prozac) were
prescribed in the same dosages used to treat depression . In all the studies,
the antidepressants were more effective than were the place-bos in reducing
binge eating. They also improved mood and reduced preoccupation with shape and
weight. Most of the positive results, however, were short term, with about one
third of clients relapsing within a 2-year period (Agras, 2006).
Related Topics