Chapter: Psychiatric Mental Health Nursing : Eating Disorders
Anorexia Nervosa
ANOREXIA NERVOSA
Onset and Clinical Course
Anorexia nervosa typically begins between 14 and 18 years of age.
In the early stages, clients often deny they have a neg-ative body image or
anxiety regarding their appearance. They are very pleased with their ability to
control their weight and may express this. When they initially come for
treatment, they may be unable to identify or to explain their emotions about
life events such as school or relationships with family or friends. A profound
sense of emptiness is common.
As the illness progresses, depression and lability in mood become more
apparent. As dieting and compulsive behaviors increase, clients isolate
themselves. This social isolation can lead to a basic mistrust of others and
even paranoia. Clients may believe their peers are jealous of their weight loss
and may believe that family and health care professionals are trying to make
them “fat and ugly.”
In long-term studies of clients with anorexia nervosa, Anderson and
Yager (2005) reported that 30% were well, 30% were partially improved, 30% were
chronically ill, and 10% had died of anorexia-related causes. Clients with the
lowest body weights and longest durations of illness tended to relapse most
often and have the poorest out-comes. Clients who abuse laxatives are at a
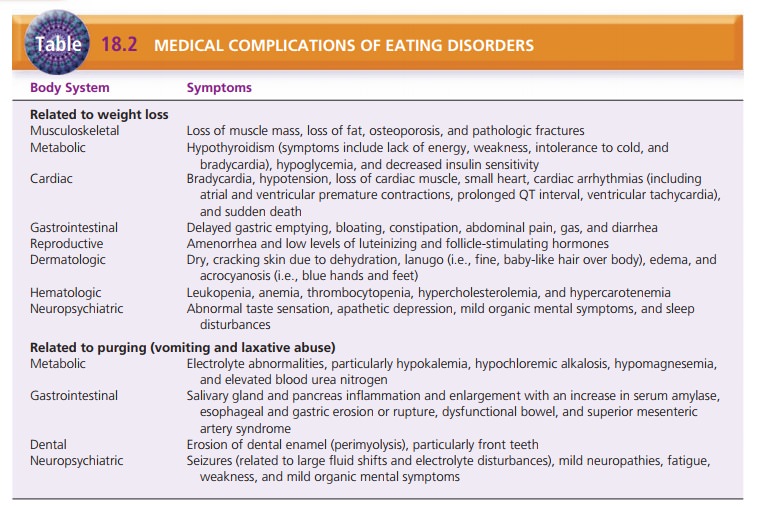
greater risk for medical complications. Table 18.2 lists common medical
complications of eating disorders.
Treatment and Prognosis
Clients with anorexia nervosa can be very difficult to treat
because they are often resistant, appear uninter-ested, and deny their
problems. Treatment settings include inpatient specialty eating disorder units,
partial hospitalization or day treatment programs, and outpa-tient therapy. The
choice of setting depends on the sever-ity of the illness, such as weight loss,
physical symptoms, duration of binging and purging, drive for thinness, body
dissatisfaction, and comorbid psychiatric conditions. Major life-threatening
complications that indicate the need for hospital admission include severe
fluid, electro-lyte, and metabolic imbalances; cardiovascular complica-tions;
severe weight loss and its consequences (Andreasen
Black, 2006); and risk for suicide. Short hospital stays are most
effective for clients who are amenable to weight gain, and gain weight rapidly
while hospitalized. Longer inpatient stays are required for those who gain
weight more slowly and are more resistant to gaining additional weight (Thiels,
2008). Outpatient therapy has the best success with clients who have been ill
for fewer than 6 months, are not binging and purging, and have parents likely
to participate effectively in family therapy. Cognitive behavior therapy can
also be effective in preventing relapse and improving overall outcomes.
Medical Management
Medical management focuses on weight restoration, nutri-tional
rehabilitation, rehydration, and correction of elec-trolyte imbalances. Clients
receive nutritionally balanced meals and snacks that gradually increase caloric
intake to a normal level for size, age, and activity. Severely malnour-ished
clients may require total parenteral nutrition, tube feedings, or
hyperalimentation to receive adequate nutri-tional intake. Generally, access to
a bathroom is supervised to prevent purging as clients begin to eat more food.
Weight gain and adequate food intake are most often the criteria for
determining the effectiveness of treatment.
Psychopharmacology
Several classes of drugs have been studied, but few have shown
clinical success. Amitriptyline (Elavil) and the anti-histamine cyproheptadine
(Periactin) in high doses (up to 28 mg/day) can promote weight gain in
inpatients with anorexia nervosa. Olanzapine (Zyprexa) has been used with
success because of its antipsychotic effect (on bizarre![]()
![]() body image distortions) and associated weight
gain. Fluoxetine (Prozac) has some effectiveness in preventing relapse in
clients whose weight has been partially or com-pletely restored (Andreasen
& Black, 2006); however, close monitoring is needed because weight loss can
be a side effect.
body image distortions) and associated weight
gain. Fluoxetine (Prozac) has some effectiveness in preventing relapse in
clients whose weight has been partially or com-pletely restored (Andreasen
& Black, 2006); however, close monitoring is needed because weight loss can
be a side effect.
Psychotherapy
Family therapy may be beneficial for families of clients younger
than 18 years. Families who demonstrate enmesh-ment, unclear boundaries among
members, and difficulty handling emotions and conflict can begin to resolve
these issues and improve communication. Family therapy also is useful to help
members to be effective participants in the client’s treatment. However, in a
dysfunctional family, significant improvements in family functioning may take 2
years or more.
Individual therapy for clients with anorexia nervosa may be
indicated in some circumstances; for example, if the family cannot participate
in family therapy, if the client is older or separated from the nuclear family,
or if the cli-ent has individual issues requiring psychotherapy. Therapy that focuses
on the client’s particular issues and circum-stances, such as coping skills,
self-esteem, self-acceptance, interpersonal relationships, assertiveness, can
improve overall functioning and life satisfaction. Cognitive– behavioral
therapy (CBT), long used with clients with bulimia, has been adapted for
adolescents and used successfully (Schmidt, 2008).
Related Topics