Chapter: Essentials of Psychiatry: Professional Ethics and Boundaries
Ethical Behavior and its Relationship to the Professional Attitude
Ethical Behavior and its
Relationship to the Professional Attitude
The term professional
derives from medieval times, when scholastics were expected to “profess” their
belief in a doctrine (Dyer, 1988, p. 17). In modern times, a professional is
expected to be a learned person who has acquired special knowledge of a subject
that is of vital importance for the welfare of the community. Having expertise
is not enough, however. A professional is also obliged to adhere to certain
societal responsibilities that are founded upon a code of ethical behavior and
an attitude of service to those in need. A professional commitment to ethical
behavior and service must take precedence over monetary compensation (Dyer,
1988, p. 16). All physicians, including psychiatrists, are bound by such a
cove-nant – a sacred vow to place patient well-being before other
consid-erations (Webb, 1986). In Western medical tradition, this obligation
primarily derives from the teachings of Hippocrates in the 5th cen-tury BC.
Hippocrates’ Oath is the predominant pledge recited at the graduation exercises
at American medical schools (Dickstein et
al., 1991), and contains three of the six core principles of modern
medi-cal ethics: beneficence, nonmalfeasance, and confidentiality:
I will follow that system of regimen which
according to my ability and judgment, I consider for the benefit of my
patients, and abstain from whatever is deleterious and mischievous…. With
purity and holiness I will pass my life and practice my Art…. Into whatever houses
I enter, I will go into them for the benefit of the sick, and will abstain from
every voluntary act of mischief and corruption; and, further, from the
seduction of females or males, of freemen and slaves. Whatever, in connection
with my professional practice or not, in connection with it, I see or hear, in
the life of men, which ought not to be spoken of abroad, I will not divulge, as
reckoning that all such should be kept secret (Hippocrates, 1929).
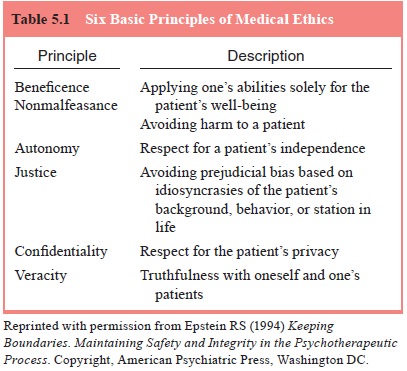
The other three general principles of medical
ethics include autonomy, justice and veracity (see Table 5.1 for a description
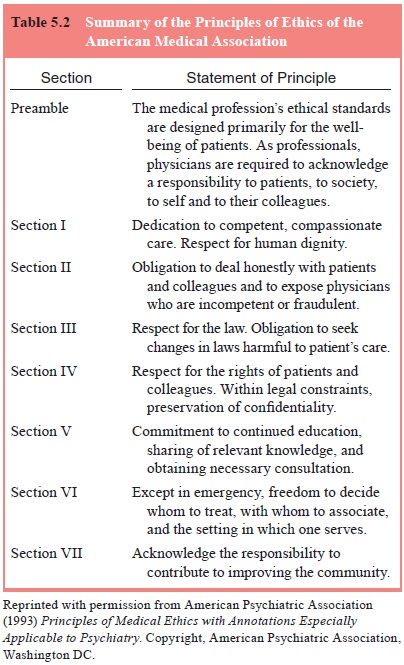
and summary of all six ethical principles; Epstein 1994, p. 20). The American
Psychiatric Association (APA) (1973) adopted the Amer-ican Medical
Association’s (AMA) Principles of Medical
Ethics, publishing it along with special annotations applicable for
psychi-atric practice. The APA has produced six revisions of these
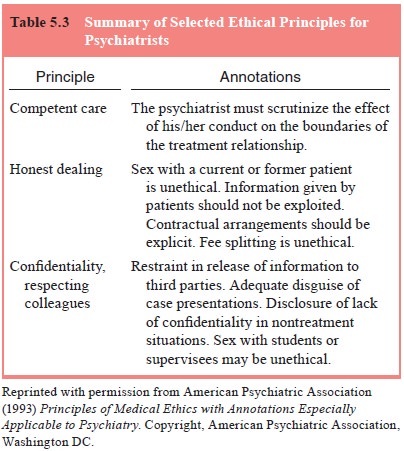
annota-tions. The seven sections of the AMA principles are summarized in Table
5.2. Table 5.3 summarizes some of the salient ethical annota-tions for
psychiatrists (American Psychiatric Association, 1993).
The World Psychiatric Association (World
Psychiatric As-sociation [WPA] 1999–2002; World Psychiatric Association Ethi-cal
Statements, 2000) developed and approved ethical guidelines, starting with the
Declaration of Hawaii in 1977, galvanized by concerns about the abuse of
psychiatry. A long process of inves-tigation within the domain of professional
ethics provided the foundation for the Declaration of Madrid that was endorsed
by the General Assembly of the WPA in 1996. In its final form, the Dec-laration
of Madrid included seven general guidelines that focused on the aims of
psychiatry. They are summarized as follows:
· Psychiatry’s
concern should be to provide the best treatment and rehabilitation for persons
with mental disorders, consist-ent with scientific knowledge, ethical
principles, and with the least possible restriction on the freedom of the
patient.
· Psychiatrists
have a duty to keep abreast of scientific devel-opments. Psychiatrists trained
in research should seek to ad-vance the frontiers of knowledge.
· The
psychiatrist–patient relationship must be based on mu-tual trust and respect,
and should allow the patient to make free and informed decisions. The
psychiatrist has a duty to accept the patient as a partner in the therapy and
to empower the patient with necessary information for rational treatment
decisions.
· Psychiatrists should consult with families of incapacitated pa-tients to safeguard the human dignity and the legal rights of the patient. Treatment should not be given against the patient’s will, unless withholding treatment would endanger the life of the patient or others. Treatment must always be in the best interest of the patient.
· Psychiatrists
performing assessments, especially when re-tained by a third party, have a duty
to inform the person being examined about the purpose of the intervention, the
use of the findings, and the possible repercussions of the assessment.
· Unless
there is a threat of serious harm to the patient or other persons,
psychiatrists should keep all patient information in confidence, and use such
information only for the purpose of helping the patient. Psychiatrists are
prohibited from making use of such information for personal, financial, or
academic benefits.
· It is
unethical to conduct research that is not in accordance with the canons of
science. Research activities should be approved by an appropriate and ethically
constituted oversight commit-tee. Because of the vulnerability of psychiatric
patients, ex-tra caution and strict ethical standards should be employed to
safeguard patients’ autonomy, patients’ mental and physical integrity, and the
selection of population groups.
An appendix in the Declaration of Madrid includes
addi-tional guidelines on specific ethical issues in psychiatry, includ-ing the
following (World Psychiatric Association, 1999–2000; World Psychiatric
Association Ethical Statements, 2000):
WPA Guidelines on Euthanasia
The physician’s role, first and foremost, is to
promote health, re-duce suffering, and protect life. The psychiatrist, whose
patients may include those who are severely incapacitated or incompetent to
reach an informal decision, should be particularly careful about actions that
could lead to the death of individuals who cannot protect themselves because of
disability, and should be vigilant to the possibility that a patient’s views
could be distorted by mental illness such as depression. In such situations,
the psychiatrist’s role is to treat the illness.
WPA Guidelines on Torture
A psychiatrist should not take part in any process
of mental or physical torture even when authorities attempt to force their involvement
in such acts. Furthermore, a psychiatrist should not participate under any
circumstances in legally authorized executions, nor participate in assessments
of competency to be executed.
WPA Guidelines on Sex Selection
It is unethical for a psychiatrist to participate
in decisions to terminate pregnancy for the purpose of sex selection.
WPA Guidelines on Organ Transplantation
Psychiatrists should seek to protect their patients
and help them exercise self-determination to the fullest extent possible. The
role of the psychiatrist is to clarify the issues surrounding organ do-nations
and to deal with the religious, cultural, social and family factors to ensure
that informed and proper decisions be made by all concerned.
WPA Guidelines on Genetic Research and Counseling in Psychiatric Patients
Psychiatrists
participating in genetic research should be mindful that the ramifications of
genetic information are not limited to the individual subject or patient but
can lead to far-reaching repercussions and consequences that can have a
negative and dis-ruptive effect on the larger family or community.
Psychiatrists are ethically obligated to observe proper practice, avoid the
risks associated with premature disclosure, misinterpretations, or mis-use of
genetic information, and should never advise a pregnant woman with mental
disorders to get an abortion based on the medical or genetic basis of her
mental illness. They should not re-fer patients to genetic testing unless there
are satisfactory levels of quality assurance and adequate genetic counseling
available to the patient.
Further
guidelines on the relationship between psychia-trists and the media, ethnic
discrimination, ethnic cleansing, and genetic research and counseling were
endorsed by the WPA General Assembly in 1999.
WPA Guidelines on Ethnic Discrimination and Ethnic Cleansing
The
Madrid Declaration defines ethnic discrimination as basi-cally racist, as it
fails to accept diversity and humanity’s common heritage. In its most malignant
form, ethnic cleansing is a crime against humanity. In this regard,
psychiatrists should not discrim-inate nor help to discriminate against
patients on ethnic grounds, nor be involved in any activity that promotes
ethnic cleansing.
WPA Guidelines on Psychiatrists Addressing the Media
It is
important that psychiatrists use the media in an affirmative way for a variety
of goals that promote good mental health care, such as advocating for the
destigmatization of mental disorder and mental patients. In all their interactions
with the media, psychiatrists are obliged to advocate for the mentally ill and
to maintain the dignity of the profession. Psychiatrists should be mindful of
the effect of their statements on the public perception of the profession and
patients, and abstain from making state-ments or undertaking public activities
that may be demeaning to either. Patients’ confidentiality should be
maintained, and the sensationalization of mental illness should be avoided.
Regarding the disclosure of research findings, psychiatrists should be
cau-tious to report only results that are generally accepted by experts, and to
convey the presentation of such results in a way that serves patients’ welfare
and dignity.
Related Topics