Chapter: Essentials of Psychiatry: Professional Ethics and Boundaries
Components of the Coherent Psychiatric Frame
Components of the Coherent
Psychiatric Frame
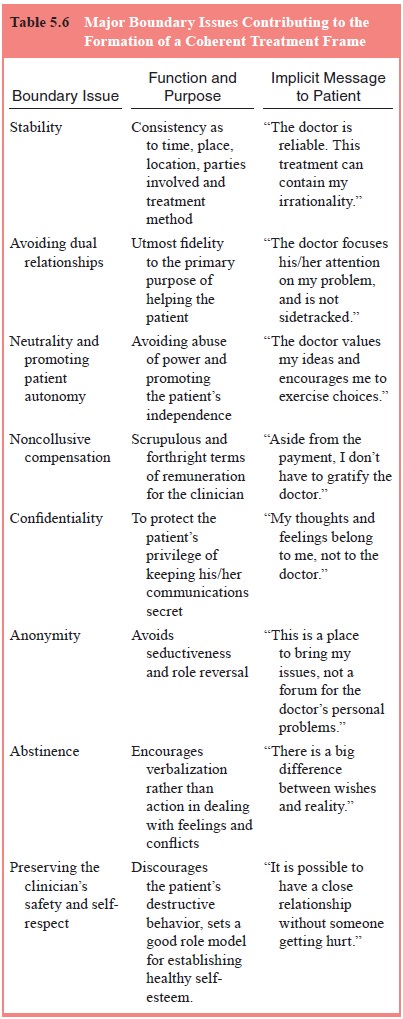
The purpose of the therapeutic frame is to protect
the patient’s safety and to promote recovery. It is the therapist’s
responsibility to structure the frame through word and deed. Langs (1984–1985)
stressed that a healthy and secure therapeutic environment is predicated on
reducing variability and uncertainty in the treatment setting as much as
possible. Table 5.6 summarizes the major boundary factors comprising the
coherent treatment frame. Careful attention to these boundary issues can assist
treating psychiatrists to communicate defining messages that strengthen the
differentiation of role and identity between patient and practitioner.
The diversity of opinion regarding optimal methods
of treatment for specific psychiatric disorders makes it very dif-ficult to
devise a set of specific guidelines that are appropriate for psychiatrists
adhering to a wide spectrum of theoretical orientations. Dyer (1988, pp. 45–57)
emphasized how problem-atic it is to define a comprehensive ethical system,
whether it is based on a set of specific rules (deontological ethics), on a
list of values and goals (teleological ethics), or from consideration of the
emotional and practical consequences of a given course of action
(consequentialist ethics). A parallel dilemma exists when it comes to defining
psychiatric boundaries. For this reason, guidelines for psychiatrists should
enhance patient safety, fos-ter adherence to established clinical principles,
and help to avoid specific consequences that are detrimental to either patient or
practitioner. Such an approach is consistent with an intensifying interest in
reducing preventable medical error. In his seminal work on human error, Reason
(1990, p. 69) outlined three major types of performance as a way to address the
sources of preventable human error. These categories include rule-based
performance, skill-based performance and knowledge-based performance. As an
example, Reason described how the use of inadvisable rules leads to rare but
preventable collisions at sea, citing studies re-porting how experienced
maritime pilots expose themselves and others to unnecessary and potentially
serious risk by allowing their own vessel to navigate too closely to adjacent
ships even when there is plenty of sea room to avoid such proximity:
The confidences these and other experienced
operators have in their ability to get themselves out of trouble can maintain
inad-visable rule behavior. This is particularly so when a high value is
attached to recovery skills and where the deliberate courting of a moderate
degree of risk is seen as a necessary way of keep-ing these skills sharp.
With regard to rule-based procedures for reducing
error in psychiatric practice, each boundary issue can be exam-ined from the
point of view of clearly indicated
procedures, relatively risky procedures
and contraindicated procedures (Epstein, 1994, pp. 113–117). In the
ensuing discussion of com-ponents of the psychiatric frame, lists of these
various types of procedures are adapted from Epstein’s earlier work on
boundaries (Epstein, 1994, pp. 119–236).
Riskier procedures that fall into the “gray zone” are not necessarily unethical or unsound. However, psychiatrists engag-ing in such activities should be aware of the circumstances under which they increase or reduce the chance for injury either to the patient or themselves. For example, under most conditions, it is probably unwise to attempt psychiatric treatment of one’s next-door neighbor. Nevertheless, practitioners living in remote areas or working in confined ethnic communities might, as a matter of practicality, be forced to treat such a patient for whom no reason-able alternative exists. The hazard of no treatment may outweigh other factors in the situation. However, the fact that psychiatrists sometimes must treat patients under risky circumstances does not mean they should disregard the increased hazard they areassuming or forget about optimal treatment standards, just as the exigencies of battlefield surgery do not obviate the need to strive for aseptic technique.
Psychiatrists should safeguard against any
semblance of inappropriate behavior even if the activity can be justified as
seem-ingly harmless. For example, seeking social activities with patients
outside of the treatment setting can be interpreted by patients or their family
members as seductive. Gutheil and Gabbard (1993) have emphasized that the very
appearance of undue familiarity with a patient may, in and of itself, hamper
successful defense against false allegations of professional wrongdoing.
Related Topics