Chapter: Essentials of Psychiatry: Electroconvulsive Therapy
Electroconvulsive Therapy(ECT)
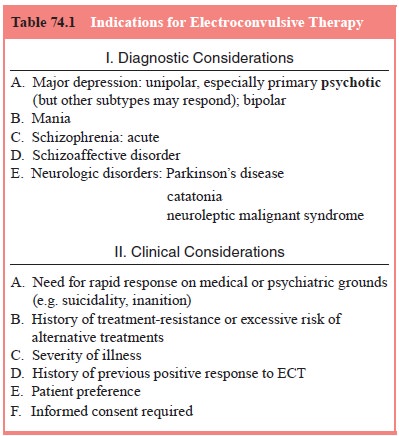
Indications
for ECT(Electroconvulsive Therapy)
General Considerations
In contrast
to its origins as a treatment of schizophrenia, ECT today is generally utilized
more frequently in patients with depression, es-pecially psychotic depression
and in the elderly. Mania and schizo-phrenia account for most of the remainder
of convulsive therapy use. The indications have been most clearly spelled out
by the American Psychiatric Association on ECT (American Psychiatric
Associa-tion, 1990, 2001), which identified “primary ” and “secondary” use of
convulsive therapy. Primary indications are those for which ECT may
appropriately be used as a first-line treatment. These include situations where
the patient’s medical or psychiatric condition re-quires rapid clinical
response, where the risk of alternative treat-ments is excessive, or where, based
on past history, response to ECT or nonresponse to medications is anticipated.
If these conditions are not met, medication or other alternative treatment is
recommended first, with ECT reserved for cases of nonresponse to adequate
trial(s), unacceptable adverse effects of the alternative treatment, or
deterio-ration of the patient’s condition, increasing the urgency of the need
for response (American Psychiatric Association, 2001). These gen-eral
principles in turn require individualized interpretation in the presence of
specific psychiatric and medical disorders. Even where ECT is not used as
treatment of first choice, its introduction sooner in the decision tree rather
than being reserved as a “last resort” may spare the patient multiple
unsuccessful medication trials, thereby avoiding months of suffering and
possibly reducing the likelihood of treatment resistance (American Psychiatric
Association, 2001). Modern diagnostic and clinical considerations in the
recommenda-tion of ECT are summarized in Table 74.1.
ECT in Depression
It is
well established that major depression is a heterogeneous dis-order,
encompassing mildly ill, functioning outpatients, as well as profoundly
disturbed, dysfunctional, or often psychotic inpatients. Along this spectrum,
ECT appears higher in the treatment hier-archy for the more severe presenting
depression, usually defined by the presence of neurovegetative signs,
psychosis, or suicidality (Abrams, 1982; American Psychiatric Association,
2000, 2001).
While
there are no absolute rules, severely melancholic or psychotically depressed
patients are often appropriate candidates for ECT as treatment of first choice,
whereas more moderately ill individuals might not be considered for ECT until
adequate medication trials have failed.
Predictors of Response
The
literature describes an overall response rate to ECT of 75 to 85% in depression
(Crowe, 1984; O’Connor et al., 2001).
Efforts to delineate subtypes of depression particularly responsive to ECT have
yielded inconsistent results. ECT is most likely to be helpful in an acute
episode of severe depression of relatively brief duration (Rich et al., 1984). Combined data from two
simulated-ECT-controlled trials (Brandon et
al., 1984; Buchan et al., 1992)
identified the presence of delusions and psychomotor retardation as predictive
of preferential response.
Psychotic
depression, increasingly recognized as a distinct subtype of mood disorder that
responds poorly to antidepressants alone, has emerged as a powerful indication
for ECT (Potter et al., 1991;
Petrides et al., 2001). In this
subgroup, ECT is at least as effec-tive as a combination trial of
antidepressant and antipsychotic med-ications. On balance, the evidence
supports the early use of ECT in psychotic depression, particularly in lieu of
prolonged, complicated medication trials that may be poorly tolerated,
especially in the el-derly (Khan et al.,
1987; Potter et al., 1991; Sackeim,
1993).
While bipolar (discussed below) and unipolar depressions are equally responsive to ECT (American Psychiatric Associa-tion, 2002), response may be less likely with secondary than primary depression, in both adults (Kramer, 1982; Zorumski et al., 1986; Zimmerman et al., 1986a), including the elderly
Bipolar Disorder
ECT is an
extremely effective and rapidly acting treatment for both acute mania and
bipolar depression (American Psychiatric Association, 2002). However, it is
infrequently used for mania, because of the availability of pharmacological
strategies. Nonetheless, ECT has been repeatedly endorsed as an accepted
second- or third-line treatment for acute manic episodes, particularly in cases
of medication resistance, in patients of all ages (NIH/NIMH, 1985; Goodwin and
Jamison, 1990; Mukherjee et al.,
1994; Van Gerpen et al., 1999;
American Psychiatric Association,
2002). In medical emergencies associated with mania, ECT can be regarded as a
treatment of first choice (American Psychiatric Association, 2002). The same is
true for medical conditions accompanying acute mania (including pregnancy,
discussed later) that contraindicate or render intolerable the use of
psychotropic medications.
There is
little information on which manic patients benefit most from ECT or on optimal
ECT treatment in mania. Bipolar depression responds as well as unipolar
depression to ECT, in both adult and geriatric patients (American Psychiatric
Association, 2002). Hypomania or mania is a risk of using ECT for depression in
bipolar patients, but this is not different from the experience with any
antidepressant treatment in this disorder (Gormley et al., 1998; American Psychiatric Association, 2001, 2002).
Schizophrenia
Among the
changes undergone by convulsive therapy over its 60-year history, few are as
striking as those associated with its use in chronic psychotic illness. ECT has
evolved from a treatment of first choice to often a treatment of last resort
for DSM-IV schizo-phrenia. However, the efficacy of ECT for depressive symptoms
associated with psychotic illness is reflected in recent nationwide data
showing the use of convulsive therapy in almost 12% of patients with recurrent
major depression comorbid with schizo-phrenia (Olfson et al., 1998), a utilization rate higher than that seen in
uncomplicated recurrent depressive disorder.
The
American Psychiatric Association Task Force on ECT (American Psychiatric
Association, 2001) and the Canadian Psy-chiatric Association (Enns and Reiss,
1992) identified a role for ECT as a second-line treatment for selected
patients with schizo-phrenia, particularly when associated with a brief
duration of ill-ness and/or affective symptoms.
It has
been consistently found that the schizophrenic patients most likely to respond
to ECT are those with good prognosis signs: mood disturbances, short duration
of illness, predominance of positive rather than negative symptoms, and
overexcitement (Fink and Sackeim, 1996). The potential respon-siveness of acute
psychotic symptoms in schizophrenia to ECT is more emphatically stated in the
2001 revision of the American Psychiatric Association Task Force Report
compared with the previous edition, based on research conducted and compiled in
the intervening decade (Fink and Sackeim, 1996).
Other Axis I Disorders
As
reiterated in the Surgeon General’s report on mental health (US Department of
Health and Human Services, 1999), ECT has no demonstrated efficacy in
dysthymia, substance abuse, or anxi-ety disorder. Nonetheless, ECT may play a
role when the sever-ity of a secondary major depression is severe and/or treatment
refractory (American Psychiatric Association, 2001). In such cir-cumstances,
ECT can be expected to improve the comorbid mood component, leaving the
underlying primary disorder untreated; in some circumstances, removal of the
burden of overlying de-pression may indirectly benefit the underlying disorder.
In the face of a potentially ECT-responsive major depressive episode, the
presence of a nonmood Axis I disorder, even substance abuse, should not
constitute a contraindication to the use of convulsive therapy (Olfson et al., 1998; American Psychiatric
Association, 2001).
Axis II Disorders
There are
no evidence-based biological treatments for DSM-IV Axis II personality
disorders, including ECT. Given the high incidence of comorbid, often
treatment-refractory depression that accompanies Axis II pathology, ECT has
been used in per-sonality disordered patients, with inconsistent – but
generally negative – reports of success, for many years.
Neurologic Disorders
Only 1%
of patients admitted with a primary diagnosis other than a mood disorder or
schizophrenia are treated with ECT in this country (Thompson et al., 1994). Nonetheless, individuals
with neurologic or other medical problems often suffer from primary or secondary
mood or motor disorders that are ECT-responsive.
Catatonia
Over the
past decade, benzodiazepines have emerged as the phar-macological treatment of
choice for catatonia (Rosebush et al.,
1992; Ungavari et al., 1994).
However, in medication-unrespon-sive patients, prolonged drug trials with
continuing clinical de-terioration can be avoided in favor of a course of ECT
(Ungavari et al., 1994). Reflecting
current understanding of the syndrome and
its treatment, Fricchione (1989) recommended that “given the significant
morbidity and mortality associated with catatonia, ECT should be considered if
an expeditious 48- to 72-hour ben-zodiazepine trial is unsuccessful”. As a
practical point, given the now-common initial use of benzodiazepines in this
condition, the catatonic patient may come to ECT with an initially elevated
seizure threshold, and treatment parameters should be adjusted accordingly
(Fink, 2002).
Other Neurologic Illness
The
remaining neurological indications for ECT can be consid-ered to fall into two
major categories: 1) those for which, as with any medical illness, ECT is
considered for treatment of a sec-ondary depression when benefit–risk analysis
favors ECT over antidepressant medications and 2) those for which ECT may play
a special role by virtue of its unique actions compared with alter-native
treatment options.
In the
first category are such conditions as poststroke depression (Murray et al., 1986; Currier et al., 1992) and mood disturbance in
the context of brain trauma, tumor, or dementia (Hsiao et al., 1987; Liang et al.,
1988; Kohler and Burock, 2001). Medication may be difficult to tolerate by
these neurologically ill patients, tilting the potential benefit–risk ratio in
favor of ECT (Price and McAllister, 1989).
Potential
contraindications to ECT are very few and rarely are absolute (American
Psychiatric Association, 2001). Although ECT generally should not be performed
in the pres-ence of raised intracranial pressure, it has been given safely even
in the face of brain tumors and other mass lesions (Hsiao et al., 1987; Fried and Mann, 1988; Abrams, 1991; Kohler and Burock, 2001) with special steps taken
to protect against the ECT-associated hemodynamic changes; intracranial
pres-sure may be reduced with the use of oral or parenteral steroids (Beale et al., 1997).
Other Considerations in the Use of ECT
It can be
appreciated that while accurate psychiatric diagno-sis is essential to
prioritize treatment options, it is far from the only consideration for the
clinician weighing the advantages and potential problems of prescribing ECT
(American Psychiatric Association, 2001). Two often-related variables are the
patient’s state of physical health and age. A large number of individuals
receiving ECT in this country are elderly, many of whom are physically
compromised.
Two
general points should be made about the use of ECT in the elderly: 1) the
physiological changes associated with ECT – cardiovascular (elevated blood
pressure, arrhythmias), cognitive (confusion, memory loss), risk of traumatic
injury to bones and teeth – that are benign and easily tolerated in young and
middle-aged patients are prominent sources of potential ECT-associated
morbidity in geriatric patients, and 2) the safety of ECT is appreciably
enhanced if the foregoing effects on the older body, whether healthy or
diseased, are anticipated and con-trolled. For example, Casey and Davis (1996)
noted that a “rigor-ous falls prevention protocol” helped protect their elderly
ECT patients from a potentially dangerous complication seen in ear-lier studies
The very
limited use of modern ECT in young people is generally reserved for cases of
depression or mania complicated by medication resistance or the need for an
urgent clinical re-sponse. Nonetheless, where ECT is utilized in younger
patients, its efficacy and safety appear comparable to those in adults (Rey and
Walter, 1997; Cohen et al., 2000).
A special
physical health challenge to the treatment of mental disorders is presented by
pregnancy. Guidelines for the administration of ECT in the pregnant patient,
incorporating measures such as intravenous hydration, avoidance of
hyperven-tilation and nonessential anticholinergic medication, measures against
gastric reflux, proper positioning of the patient during treatment, and uterine
and fetal cardiac monitoring, have been developed and incorporated into modern
practice (American Psychiatric Association, 2001).
Pretreatment Evaluation
Once the
decision has been made to proceed with a course of ECT, specific steps are
taken by the treatment team to maximize the benefits and minimize the risks. In
some instances these pro-cedures are part of the initial work-up, and the
results may influ-ence treatment decisions, as when certain psychiatric or
physical disorders are ruled in or out.
The
psychiatrist will want to make use of appropriate consultants, especially
representing the fields of anesthesiol-ogy and, when indicated, internal
medicine (often cardiology) or obstetrics. Given the current regulatory
climate, the physician needs to be aware of local requirements regarding the
need for second opinions or other pretreatment procedures in certain
cir-cumstances, or to arrange for guardianship or court proceedings where the
patient’s capacity to consent to ECT is in question, to assure that the
initiation of treatment is not unduly delayed.
Psychiatric Considerations
The
pre-ECT evaluation is a good time to confirm psychiatric diagnosis, including
Axis II and III. In many settings, a specific ECT consultation may be helpful
in evaluating the patient for a potentially ECT-responsive disorder and
weighing the various treatment options (Klapheke, 1997). Input from nursing and
other professional staff that have been working with the patient should be
factored in. Should the indications for ECT remain present, baseline
assessments of mental status including evaluation of suicidality, orientation
and memory will help monitor changes in both therapeutic and adverse effects
over the course of treatment. The history and effects of previous treatment
with ECT should be obtained. Also, this time, decisions must be made regarding
ongoing psychotropic medications particularly those increasing the risk of
toxicity in combination with ECT, for example lithium and those affecting
seizure threshold, such as benzodiazepines and anticonvulsants – and steps
instituted to adjust, taper, or dis-continue these medications, when
appropriate.
Other Medical Considerations
History and physical examination should focus on the cardiovas-cular and neurological systems, the areas of greatest risk. The consulting internist, anesthesiologist, or other physician should advise the treatment team regarding cardiovascular risk of ECT and the need for any modifications in treatment technique, such as medications to moderate hemodynamic changes (Dolinski and Zvara, 1997). Appropriate pretreatment optimization and moni toring of medical conditions that may be affected by ECT, such as diabetes, should be arranged at this time.
In the
uncomplicated situation, the routine laboratory work-up for ECT is that
indicated for any procedure involving general anesthesia: complete blood count,
serum electrolyte levels and electrocardiogram (ECG)
(American Psychiatric
Association, 2001; Chaturvedi et al., 2001). Chest X-ray is often obtained as
well. The need for further pretreatment work-up, such as serum chemistries,
urinalysis, HIV antibody titers and medication blood concentrations, is
determined on an individual basis (Lafferty et al., 2001). Given a normal
neurologic and fundoscopic examination, computerized tomography (CT) or
magnetic resonance imaging (MRI) of the brain is not indicated.
Lumbosacral
spine films, historically routine prior to institution of muscle relaxation in
the ECT premedication protocol, have become optional for many patients. This
remains appropriate for older patients with a history of or at risk for
osteoporosis, and for any patient with a history of bone trauma. A formal
anesthesiology consultation should result in an assignment of the degree of
anesthesia risk and recommendations for any necessary modification in the ECT
protocol (Folk et al., 2000). A personal or family history of anesthesia
complications may call for special assessment. The condition of dentition
should be routinely assessed to avoid the treatment-associated risk of
aspiration or fracture of loose teeth or bridgework.
Informed Consent
Among the
unique features of ECT compared with other standard psychiatric treatments is
the requirement for written informed consent by the patient or legal guardian
or other substitute. Guidelines regarding the content of a standard informed
consent form for ECT have been published (American Psychiatric Asso-ciation,
2001). Supplemental information regarding ECT for pa-tients and their families
in a variety of media is also available and its distribution is encouraged
(Fink, 1999; American Psychiatric Association, 2001).
The
NIH/NIMH Consensus Development Conference on ECT (1985) emphasized that
informed consent is a process that continues throughout the treatment course.
Given the transient cognitive impairments common in depression and during an
ECT course, it is particularly necessary to maintain a dialogue with the
patient as treatment progresses to assure that all of the patient’s questions
and concerns are addressed, even if repetitive discourse ensues. With
appropriate modification of the presenta-tion of information, including use of
nonverbal demonstration of the procedure, even patients with mental retardation
often can make informed decisions about consent for ECT (Van Waarde et al., 2001).
Related Topics