Chapter: Clinical Dermatology: Drug eruptions
Drug eruptions Presentation: Some drugs and the reactions they can cause
Presentation
Some
drugs and the reactions they can cause
Experience
helps here, together with a knowledge of the reactions most likely to be caused
by individual drugs, and also of the most common causes of the vari-ous
reaction patterns. Any unusual rash should be suspected of being a drug
reaction, and approached along the lines listed in Table 22.2.
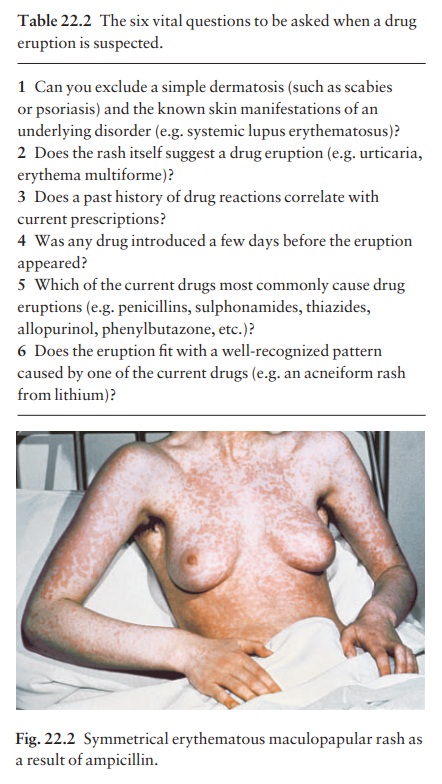
Antibiotics
Penicillins and sulphonamides are among the drugs most commonly causing allergic reactions. These are often morbilliform (Fig. 22.2), but urticaria and ery-thema multiforme are common too. Viral infections are often associated with exanthems, and many rashes are incorrectly blamed on an antibiotic when, in fact, the virus was responsible.
Most patients with infec-tious mononucleosis develop a morbilliform rash if ampicillin
is administered. Penicillin is a common cause of severe anaphylactic reactions,
which can be life-threatening. Minocycline can accumulate in the tissues and
produce a brown or grey colour in the mucosa, sun-exposed areas or at sites of
inflamma-tion, as in the lesions of acne. Minocycline can rarely cause the
hypersensitivity syndrome reaction, hepati-tis, worsen lupus erythematosus, or
elicit a transient lupus-like syndrome.
Penicillamine
Like
penicillin itself, this can cause morbilliform erup-tions or urticaria, but the
drug has also been incrim-inated as a cause of haemorrhagic bullae at sites of
trauma, of the extrusion of elastic tissue through the skin, and of pemphigus.
Oral contraceptives
Reactions
to these are less common now that their hormonal content is small. The hair
fall that may fol-low stopping the drug is like that seen after pregnancy
(telogen effluvium;). Chloasma, hirsutism, ery-thema nodosum, acne and photosensitivity
are other reactions.
Gold
This
frequently causes rashes. Its side-effects range from pruritus to morbilliform
eruptions, to curious papulosquamous eruptions such as pityriasis rosea or
lichen planus. Erythroderma, erythema nodosum, hair fall and stomatitis may
also be provoked by gold.
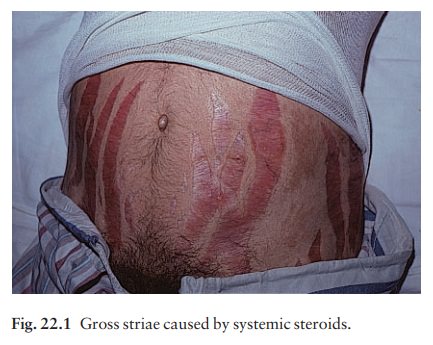
Steroids
Cutaneous
side-effects from systemic steroids include a ruddy face, cutaneous atrophy,
striae (Fig. 22.1), hirsutism, an acneiform eruption and a susceptibility to
cutaneous infections, which may be atypical.
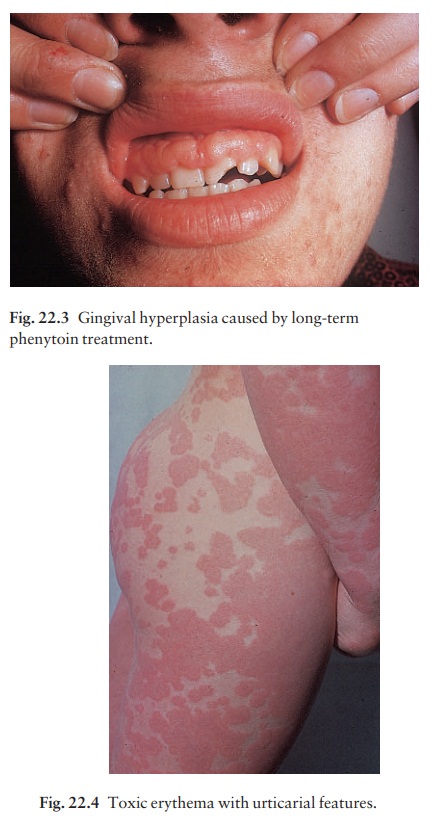
Anticonvulsants
There
may be cross-reactivity between phenytoin, carbamazepine and phenobarbitol.
Skin reactions are common and include erythematous, morbilliform, urticarial
and purpuric rashes. Toxic epidermal necro-lysis, erythema multiforme, exfoliative
dermatitis, the hypersensitivity syndrome reaction and a lupus
erythematosus-like syndrome are rare. A phenytoin-induced pseudolymphoma
syndrome has also been described in which fever and arthralgia are accom-panied
by generalized lymphadenopathy and hepatos-plenomegaly and, sometimes, some of
the above skin signs. Long-term treatment with phenytoin may cause gingival
hyperplasia (Fig. 22.3) and coarsening of the features as a result of
fibroblast proliferation.
Highly active antiretroviral drugs
The
long-term use of highly active antiretroviral drugs (HAART) has been commonly
associated with lipody-strophy, producing a gaunt facies with sunken cheeks.
Related Topics