Chapter: Basic & Clinical Pharmacology : Special Aspects of Perinatal & Pediatric Pharmacology
Drug Use During Lactation
DRUG USE DURING LACTATION
Despite
the fact that most drugs are excreted into breast milk in amounts too small to
adversely affect neonatal health, thou-sands of women taking medications do not
breast-feed because of misperception of risk. Unfortunately, physicians
contribute heavily to this bias. It is important to remember that formula
feed-ing is associated with higher morbidity and mortality in all
socio-economic groups.
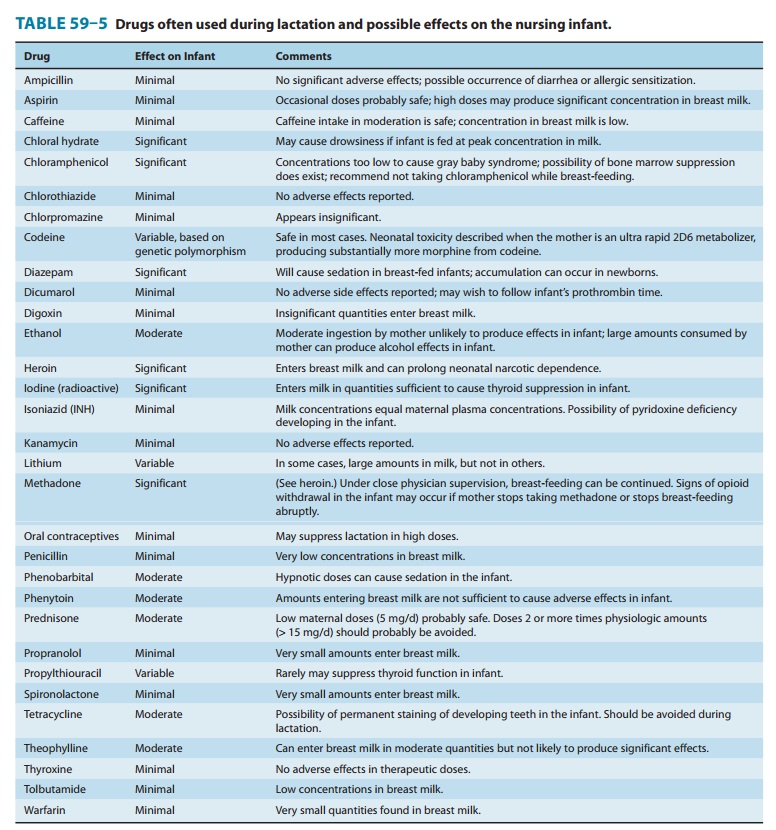
Most drugs
administered to lactating women are detectable in breast milk. Fortunately, the
concentration of drugs achieved in breast milk is usually low (Table 59–5).
Therefore, the total amount the infant would receive in a day is substantially
less than what would be considered a “therapeutic dose.” If the nursing mother
must take medications and the drug is a relatively safe one, she should
optimally take it 30–60 minutes after nursing and 3–4 hours before the next
feeding. This allows time for many drugs to be cleared from the mother’s blood,
and the concentra-tions in breast milk will be relatively low. Drugs for which
no data are available on safety during lactation should be avoided or
breast-feeding discontinued while they are being given.
Most
antibiotics taken by nursing mothers can be detected in breast milk.
Tetracycline concentrations in breast milk are approx-imately 70% of maternal
serum concentrations and present a risk of permanent tooth staining in the
infant. Isoniazid rapidly reaches equilibrium between breast milk and maternal
blood. The concentrations achieved in breast milk are high enough so that signs
of pyridoxine deficiency may occur in the infant if the mother is not given
pyridoxine supplements.
Most
sedatives and hypnotics achieve concentrations in breast milk sufficient to
produce a pharmacologic effect in some infants. Barbiturates taken in hypnotic
doses by the mother can produce lethargy, sedation, and poor suck reflexes in
the infant. Chloral hydrate can produce sedation if the infant is fed at peak
milk concentrations. Diazepam can have a sedative effect on the nurs-ing
infant, but, most importantly, its long half-life can result in significant
drug accumulation.
Opioids such as
heroin, methadone, and morphine enter breast milk in quantities potentially
sufficient to prolong the state of neonatal narcotic dependence if the drug was
taken chronically by the mother during pregnancy. If conditions are well
controlled and there is a good relationship between the mother and the
phy-sician, an infant could be breast-fed while the mother is taking methadone.
She should not, however, stop taking the drug abruptly; the infant can be
tapered off the methadone as the mother’s dose is tapered. The infant should be
watched for signs of narcotic withdrawal. Although codeine has been believed to
be safe, a recent case of neonatal death from opioid toxicity revealed that the
mother was an ultra rapid metabolizer of cytochrome 2D6 substrates, producing
substantially higher amounts of mor-phine. Hence, polymorphism in maternal drug
metabolism may affect neonatal exposure and safety. A subsequent case control
study has shown that this situation is not rare. The FDA has pub-lished a
warning to lactating mothers to exert extra caution while using painkillers
containing codeine.
Minimal use of alcohol
by the mother has not been reported to harm nursing infants. Excessive amounts
of alcohol, however, can produce alcohol effects in the infant. Nicotine
concentrations in the breast milk of smoking mothers are low and do not produce
effects in the infant. Very small amounts of caffeine are excreted in the
breast milk of coffee-drinking mothers.
Lithium enters breast
milk in concentrations equal to those in maternal serum. Clearance of this drug
is almost completely depen-dent upon renal elimination, and women who are
receiving lithium may expose the infant to relatively large amounts of the drug.
Radioactive
substances such as iodinated 125I
albumin and other forms of radioiodine can cause thyroid suppression in infants
and may increase the risk of subsequent thyroid cancer as much as tenfold.
Breast-feeding is contraindicated after large doses and should be withheld for
days to weeks after small doses. Similarly, breast-feeding should be avoided in
mothers receiving cancer chemotherapy or being treated with cytotoxic or
immuno-modulating agents for collagen diseases such as lupus erythemato-sus or
after organ transplantation.
Related Topics