Chapter: Clinical Dermatology: Disorders of pigmentation
Disorders with increased pigmentation (hypermelanosis)
Disorders
with increased pigmentation (hypermelanosis)
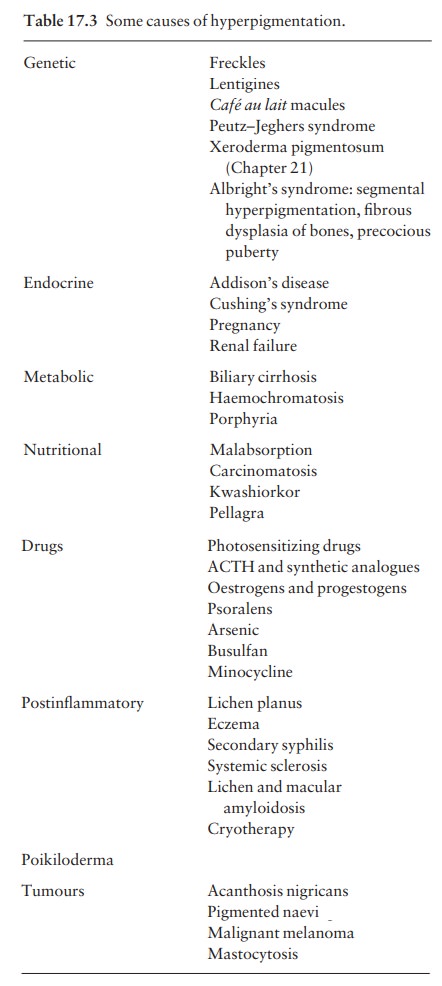
Some
of these disorders are listed in Table 17.3. The most common will be described
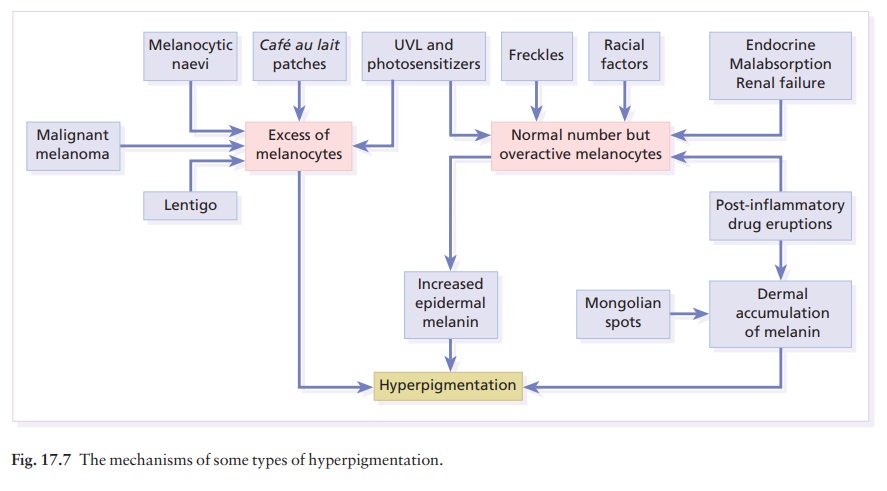
below and the mechan-isms involved are summarized in Fig. 17.7.
Freckles (ephelides)
Freckles
are so common that to describe them seems unnecessary. They are seen most often
in the red-haired or blond person as sharply demarcated light brown-ginger
macules, usually less than 5 mm in diameter. They multiply and become darker
with sun exposure.
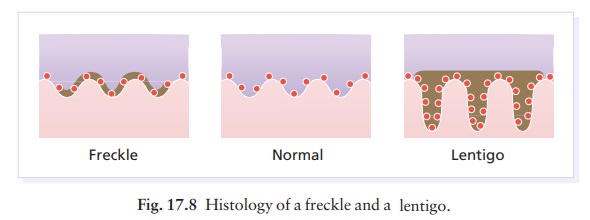
Increased
melanin is seen in the basal layer of the epidermis without any increase in the
number of melanocytes, and without elongation of the rete ridges (Fig. 17.8).
No treatment is necessary.
Melanotic macule of the lip
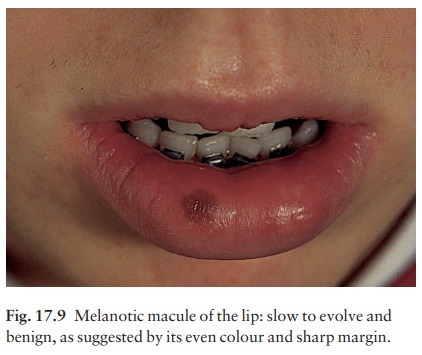
This
common lesion (Fig. 17.9) worries doctors but is benign. Its histology is
similar to that of a freckle (Fig. 17.8).
Lentigo
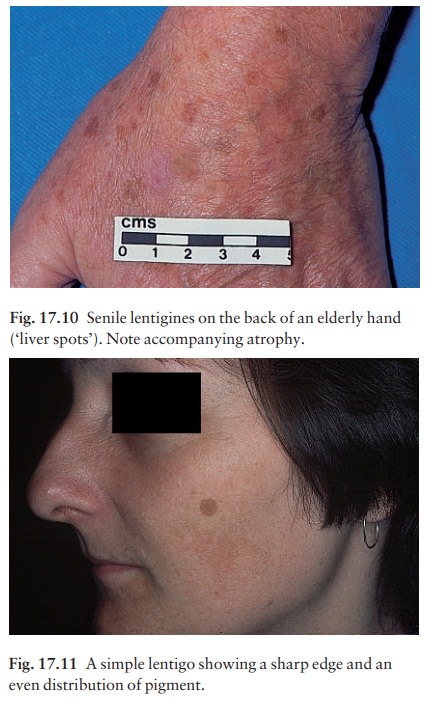
Simple and senile lentigines look alike. They are light or dark brown macules, ranging from 1 mm to 1 cm across. Although usually discrete, they may have an irregular outline. Simple lentigines arise most often in childhood as a few scattered lesions, often on areas not exposed to sun, including the mucous membranes. Senile or solar lentigines are common after middle age on the backs of the hands (‘liver spots’; Fig. 17.10) and on the face (Fig. 17.11) In contrast to freckles, lentigines have increased numbers of melanocytes. They should be distinguished from freckles, from junctional melanocytic naevi and from a lentigo maligna. Treatment is usually unnecessary but melanin-specific high energy lasers (e.g. pigmented lesion dye laser, 510 nm; Q-switched ruby laser, 694 nm; Q-switched alexandrite laser, 755 nm) are extremely effective for treating ugly lesions. Liver spots associ-ated with actinic damage lighten or clear with the daily application of 0.1% tretinoin cream (Formulary 1) or 3% hydroquinone (Formulary 1).
Conditions associated with multiple lentigines
Three
rare but striking syndromes feature multiple lentigines.
Peutz–Jeghers syndrome
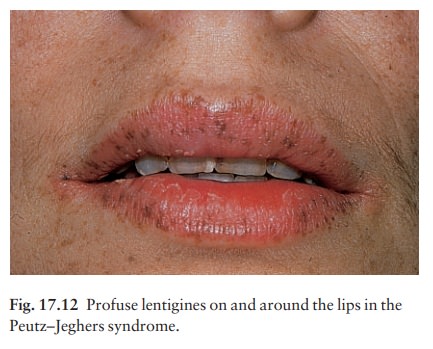
Profuse
lentigines are seen on and around the lips in this autosomal dominant condition
(Fig. 17.12). Scattered lentigines also occur on the buccal mucosa, gums, hard
palate, hands and feet. The syndrome is important because of its association
with polyposis of the small intestine, which may lead to recurrent
intussusception and, rarely, to malignant transformation of the polyps. Ten per
cent of affected women have ovarian tumours.
Cronkhite–Canada syndrome
This
consists of multiple lentigines on the backs of the hands and a more diffuse
pigmentation of the palms and volar aspects of the fingers. It may also
associate with gastrointestinal polyposis. Alopecia and nail abnormalities
complete the rare but characteristic clinical picture.
LEOPARD syndrome
This is an acronym for generalized Lentiginosis associ-ated with cardiac abnormalities demonstrated by ECG, Ocular hypertelorism, Pulmonary Stenosis, Abnormalgenitalia, Retardation of growth and Deafness.
Chloasma
Chloasma
is a patterned pigmentation of the face occurring in women during pregnancy or
when taking oral contraceptives. The areas of increased pigmenta-tion are well
defined, symmetrical and their edges are often scalloped (the mask of
pregnancy; Fig. 17.13). Most of the extra melanin lies in the epidermis, but
there is some in the dermis too, making treatment more difficult. If the area
is viewed under Wood’s light, an increase in contrast or in pigmentation
sug-gests mainly epidermal pigmentation, whereas loss of contrast suggests
dermal pigment. The light brown colour becomes darker after exposure to the
sun. The placenta may secrete hormones that stimulate melanocytes. Chloasma
should be differentiated from a phototoxic reaction to a scented cosmetic or to
a drug. Treatment is unsatisfactory, although some find bleaching agents that
contain hydroquinone helpful. The optimal effect is achieved with preparations
con-taining 2–5% hydroquinone, applied for 6–10 weeks. After this, maintenance
treatment should be with preparations containing no more than 2% hydro-quinone.
A sunscreen will make the pigmentation less obvious during the summer and will
minimize the chance of spread.

Endocrine hyperpigmentation
Addison’s disease
Hyperpigmentation
caused by the overproduction of ACTH is often striking. It may be generalized
or lim-ited to the skin folds, creases of the palms, scars and the buccal
mucosa.
Cushing’s syndrome
Increased
ACTH production may cause a picture like that of Addison’s disease. The
hyperpigmentation may become even more marked after adrenalectomy (Nelson’s
syndrome).
Pregnancy
There
is a generalized increase in pigmentation dur-ing pregnancy, especially of the
nipples and areolae, and of the linea alba. Chloasma may also occur. The nipples and areolae
remain pigmented after parturition.
Chronic renal failure
The
hyperpigmentation of chronic renal failure and of patients on haemodialysis is
caused by an increase in levels of pituitary melanotrophic peptides, normally
cleared by the kidney.
Porphyria
Formed
porphyrins, especially uroporphyrins, are pro-duced in excess in cutaneous
hepatic porphyria and congenital erythropoietic porphyria. These endogenous
photosensitizers induce hyperpigmenta-tion on exposed areas; skin fragility,
blistering, milia and hypertrichosis are equally important clues to the
diagnosis.
Nutritional hyperpigmentation
Any
severe wasting disease, such as malabsorption, AIDS, tuberculosis or cancer,
may be accompanied by diffuse hyperpigmentation. Kwashiorkor presents a mixed
picture of generalized hypopigmentation and patchy postinflammatory
hyperpigmentation, and in this condition the hair is red-brown or grey.
Chemicals causing hyperpigmentation
Table
16.2 lists drugs that commonly photosensitize. All can cause hyperpigmentation
of the exposed skin. Psoralens are used in the photochemotherapy of
pso-riasis and, more rarely, of
vitiligo.
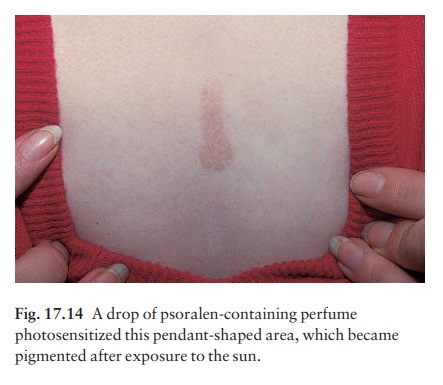
The
term ‘berloque dermatitis’ (Fig. 17.14) refers to a ‘pendant’ of
hyperpigmentation, often on the side of the neck, where cosmetics have been
applied which contain the photosensitizing 5-methoxypsoralen. Cosmetics for men
(pre- and aftershaves, etc.) are a thriving source of these.
Arsenic
is not used medically nowadays. Once it caused ‘raindrop’ depigmentation within
a diffuse bronzed hyperpigmentation.
Busulfan
and bleomycin, used to treat some forms of leukaemia, frequently cause diffuse
hyperpigmen-tation but may also cause brown streaks (flagellate
hyperpigmentation). Minocycline can leave blue-black drug deposits in inflamed
acne spots on the shins or on the mucosae. They can be removed successfully
with Q-switched ruby laser (694 nm) treatment.
Postinflammatory hyperpigmentation
This
is common after lichen planus. It is also a feature of systemic sclerosis and some types of cutaneous amyloidosis, and
is often an unwelcome sequel of cryotherapy.
Poikiloderma
Poikiloderma
is the name given to a triad of signs: reticulate pigmentation, atrophy and
telangiectasia. It is not a disease but a reaction pattern with many causes
including X-irradiation, photocontact reac-tions, and connective tissue and
lymphoreticular dis-orders. Congenital variants (Rothmund–Thomson syndrome,
Bloom’s syndrome and Cockayne’s syn-drome) associated with photosensitivity,
dwarfism and mental retardation also occur.
Related Topics