Chapter: Clinical Dermatology: Disorders of pigmentation
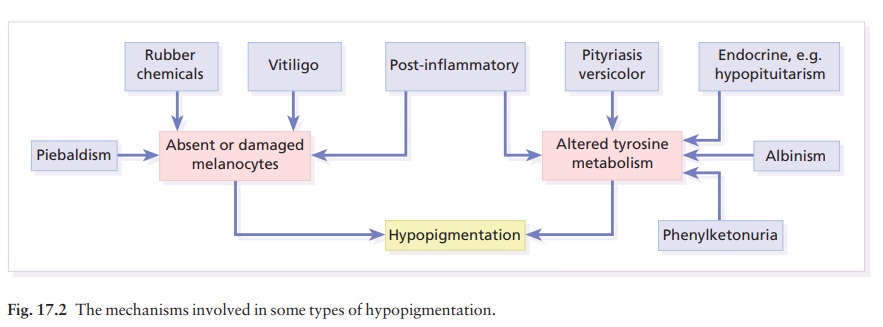
Decreased melanin pigmentation
Decreased
melanin pigmentation
Some
conditions in which there is a lack of melanin are listed in Table 17.2.
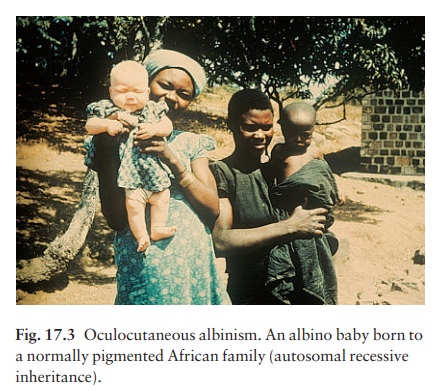
Oculocutaneous albinism
In
this condition, little or no melanin is made either in the skin and eyes
(oculocutaneous albinism) or in the eyes alone (ocular albinismanot discussed
further here). The prevalence of albinism of all types ranges from 1 in 20 000
in the USA and UK to 5% in some communities.
Cause
The hair bulb test (see Investigations) separates oculocutaneous albinism into two main types: tyrosinase-negative and tyrosinase-positive.
Roughly equal
numbers of the two types are found in most communities, both being inherited as
autosomal recessive traits. This explains how children with two albino parents
can sometimes themselves be normally pigmented, the genes being complementary
in the double heterozygote (Fig. 17.3).
The
tyrosinase gene lies on chromosome 11q14-q21. More than 20 allelic variations have
been found there in patients with tyrosinase-negative albinism. The gene for
tyrosinase-positive human albinism has been mapped to chromosome 15q11-q13. It
probably encodes for an ion channel protein in the melanosome involved in the
transport of tyrosine.
Presentation and course
The
whole skin is white and pigment is also lacking in the hair, iris and retina
(Fig. 17.3). Albinos have poor sight, photophobia and a rotatory nystagmus. As
they grow older tyrosinase-positive albinos gain a little pigment in their
skin, iris and hair. Negroid skin becomes yellow-brown and the hair becomes
yellow. Albinos may also develop freckles. Sunburn is common on unprotected
skin. As melanocytes are present, albinos have non-pigmented melano-cytic naevi
and may develop amelanotic malignant melanomas.
Complications
In the tropics these unfortunate individuals develop numerous sun-induced skin tumours even when they are young, confirming the protective role of melanin.
Differential diagnosis
Piebaldism
and vitiligo are described below.
Investigations
Prenatal
diagnosis of albinism is now possible but may not be justifiable in view of the
good prognosis. A biopsy from fetal skin, taken at 20 weeks, is examined by
electron microscopy for arrested melanosome development.
The
hair bulb test, in which plucked hairs are incubated in dihydroxyphenylalanine,
distinguishes tyrosinase-positive from tyrosinase-negative types. Those whose
hair bulbs turn black (tyrosine-positive) are less severely affected.
Treatment
Avoidance
of sun exposure, and protection with opaque clothing, wide-brimmed hats and
sunscreen creams (Formulary 1), are essential and allow albinos in temperate
climates to live a relatively normal life. Early diagnosis and treatment of
skin tumours is critical. In the tropics the outlook is less good and the
termination of affected pregnancies may be considered.
Piebaldism
These
patients often have a white forelock of hair and patches of depigmentation
lying symmetrically on the limbs, trunk and central part of the face,
especially the chin. The condition is present at birth and is inherited as an
autosomal dominant trait. A genetic abnormal-ity in mice (dominant white
spotting) provided the clue that allowed the human piebaldism gene to be mapped
to chromosome 4q12, where the KIT pro-tooncogene lies. This encodes
the tyrosine kinase transmembrane cellular receptor on certain stem cells;
without this they cannot respond to normal signals for development and migration.
Melanocytes are absent from the hypopigmented areas. The depigmen-tation, often
mistaken for vitiligo, may improve with age. There is no effective treatment.
Waardenburg’s syndrome includes piebaldism (with a white forelock in 20% of
cases), hypertelorism, a prominent inner third of the eyebrows, irides of
different colour and deafness.
Phenylketonuria
This
rare metabolic cause of hypopigmentation has a prevalence of about 1 : 25 000.
Hypopituitarism
The
skin changes here may alert an astute physician to the diagnosis. The
complexion has a pale, yellow tinge; there is thinning or loss of the sexual
hair; the skin itself is atrophic. The hypopigmentation is caused by a
decreased production of pituitary melan-otrophic hormones .
Vitiligo
The
word vitiligo comes from the Latin word vitellus, which
means ‘veal’ (pale, pink flesh). It is an acquired circumscribed
depigmentation, found in all races; its prevalence may be as high as 0.5–1%;
its inheritance is polygenic.
Cause and types
There
is a complete loss of melanocytes from affected areas. There are two main
patterns: a common gener-alized one and a rare segmental type. Generalizedvitiligo,
including the acrofacial variant, usually startsafter the second decade. There
is a family history in 30% of patients and this type is most frequent in those
with autoimmune diseases such as diabetes, thyroid disorders and pernicious
anaemia. It is postulated that in this type melanocytes are the target of a
cell-mediated autoimmune attack. Segmental vitiligo is restricted
to one part of the body, but not necessarily to a dermatome. It occurs earlier
than generalized vitiligo, and is not associated with autoimmune dis-eases.
Trauma and sunburn can precipitate both types.
Clinical course
Generalized
type. The sharply defined, usually sym-metrical (Fig. 17.4),
white patches are especially common on the backs of the hands, wrists, fronts
of knees, neck and around body orifices. The hair of the scalp and beard may
depigment too. In Caucasoids, the surrounding skin is sometimes hyperpigmented.

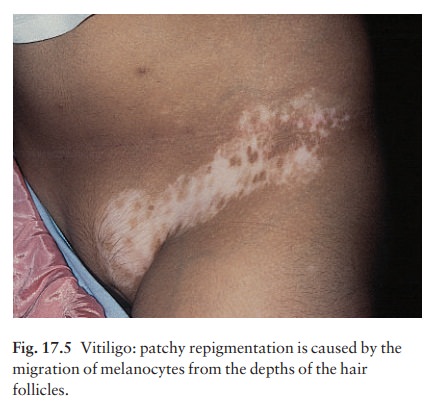
The
course is unpredictable: lesions may remain static or spread; occasionally they
repigment spontan-eously from the hair follicles.
Segmental
type. The individual areas look like thegeneralized type but
their segmental distribution is striking. Spontaneous repigmentation occurs
more often in this type than in generalized vitiligo (Fig. 17.5).
Differential diagnosis
Contact
with depigmenting chemicals, such as hydroquinones and substituted phenols in
the rubber industry, should be excluded. Pityriasis versicolor must be considered; its fine scaling and less
The patches of piebaldism are present at birth.
Sometimes leprosy must be excludedaby sens-ory testing and a general
examination. Other tropical diseases that cause patchy hypopigmentation are
leishmaniasis, yaws and pinta.
Treatment
Treatment
is unsatisfactory. Recent patches may respond to a potent or very potent
topical steroid, applied for 1–2 months. After this, the strength should be
gradually tapered to a mildly potent steroid for maintenance treatment. Some patients
improve with psoralens (trimethylpsoralen or 8-methoxypsoralen, in a dosage of
0.4–0.6 mg/kg body weight), taken 1–2 h before graduated exposure to natural
sunshine or to artificial UVA (PUVA;). Narrow band (311 nm) UVB may also be
effective. Therapy is given 2–3 times weekly for at least 6 months; new lesions
seem to respond best. Autologous skin grafts are becoming popular in some
centres although they remain experimental. The two most common pro-cedures are
minigrafting (implants of 1 mm grafts from unaffected skin) and suction blister
grafting (using the epidermal roofs of suction blisters from unaffected skin
for grafting). Melanocyte and stem cell transplants, in which single cell
suspensions are made from unaffected skin and applied to dermab-raded
vitiliginous skin, are also being investigated. The use of these techniques may
be limited by cost, and by the development of vitiligo (Köbner pheno-menon) at
donor sites.
As a general rule, established vitiligo is best left untreated in most white people, although advice about suitable camouflage preparations (Formulary 1) to cover unsightly patches should be given. Sun avoidance and screening preparations (Formulary 1) are needed to avoid sunburn of the affected areas and a heightened contrast between the pale and dark areas. Black patients with extensive vitiligo can be completely and irreversibly depigmented by creams containing the monobenzyl ether of hydroquinone.
The
social implications of this must be discussed and carefully considered, and
written consent given before such treatment is undertaken.
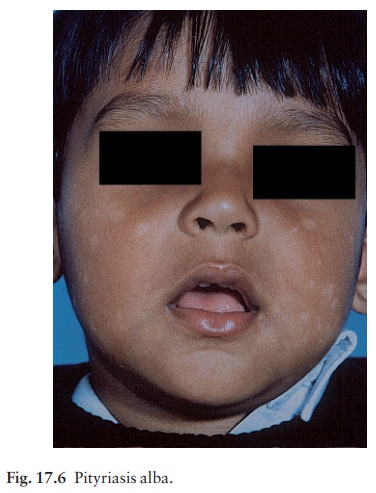
Postinflammatory depigmentation
This
may follow eczema, psoriasis, sarcoidosis, lupus erythematosus and, rarely,
lichen planus. It may also result from cryotherapy or a burn. In general, the
more severe the inflammation, the more likely pigment is to decrease rather
than increase in its wake. These prob-lems are most significant in Negroids or
Asians. With time, the skin usually repigments. Pityriasis alba is common on
the faces of children. The initial lesion is probably a variant of eczema
(pinkish with fine scal-ing), which fades leaving one or more pale, slightly
scaly, areas (Fig. 17.6). Exposure to the sun makes the patches more obvious.
White hair
Melanocytes
in hair bulbs become less active with age and white hair (canities) is a
universal sign of ageing. Early greying of the hair is seen in the rare
premature ageing syndromes, such as Werner’s syndrome, and in autoimmune
conditions such as pernicious anaemia, thyroid disorders and Addison’s disease.
Related Topics