Chapter: Ophthalmology: Lacrimal System
Disorders of the Lower Lacrimal System
Disorders of the Lower Lacrimal System
Dacryocystitis
Inflammation of the lacrimal sac is themost frequentdisorder
of the lowerlacrimal system. It is usually the result of obstruction of the
nasolacrimal duct and is unilateral in
most cases.
Acute Dacryocystitis
Epidemiology: The disorder most frequently affects adults between the agesof
50 and 60.
Etiology: The cause is usually astenosis
within the lacrimal sac. The retentionof tear fluid leads to infection from
staphylococci, pneumococci, Pseudo-monas,
or other pathogens.
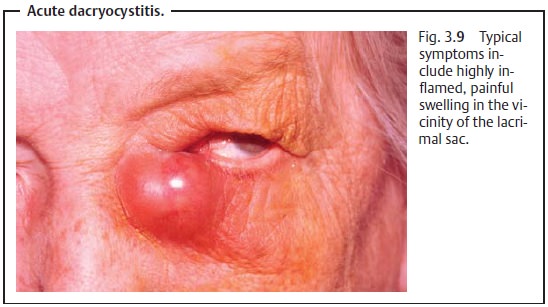
Symptoms: Clinical symptoms include highly inflamed, painfulswelling inthe vicinity of the lacrimal sac (Fig. 3.9) that may be accompanied by malaise, fever, and involvement of the regional lymph nodes. The pain may be referred asfar as the forehead and teeth. An abscess in the lacrimal sac may form in advanced disorders; it can spontaneously rupture the skin and form a drain-ing fistula.
Acute inflammation that has spread to the
surrounding tissue of the eyelids and cheek entails a risk of sepsis and
cavernous sinus thrombo-sis, which is a life-threatening complication.
Diagnostic considerations: Radiographic contrast studies or digital sub-straction
dacryocystography can visualize the obstruction for preoperative planning.
These studies should be avoided during the acute phase of the dis-order because
of the risk of pathogen dissemination.
Differential diagnosis:
❖ Hordeolum (small, circumscribed, nonmobile inflamed swelling).
❖ Orbital cellulitis (usually associated with reduced motility of
the eyeball).
Treatment: Acute casesare treated withlocal and
systemic antibioticsaccording to the specific pathogens detected. Disinfectant compresses (such as a
1:1000 Rivanol solution) can also positively influence the clinical course of
the disorder. Pus from a fluctuating
abscess is best drained through a stab
inci-sion following cryoanesthesia with a refrigerant spray.
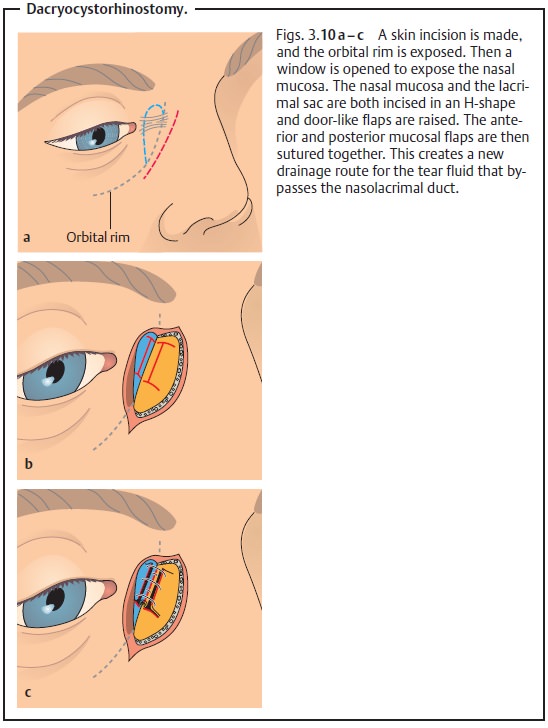
Treatment after acute symptoms have
subsided often requires
surgery (dacryocystorhinostomy; Figs. 3.10a – c) to achieve persistent relief. Also known as
a lower system bypass, this operation involves opening the lateral wall of the
nose and bypassing the nasolacrimal duct to create a direct con-nection between
the lacrimal sac and the nasal mucosa.
Chronic Dacryocystitis
Etiology: Obstruction of the nasolacrimal duct is often secondary to
chronicinflammation of the connective tissue or nasal mucosa.
Symptoms and diagnostic considerations: Theinitial
characteristicofchronic dacryocystitis is increased lacrimation. Signs of inflammation are not usually
present. Applying pressure to the inflamed lacrimal sac causes largequantities of transparent mucoid pus to
regurgitate through the punctum.
Chronic inflammation of the lacrimal sac can
lead to a serpiginous cor-neal ulcer.
Treatment: Surgical intervention is the only effective treatment in the
vastmajority of cases. This involves either a dacryocystorhinostomy (creation
of a direct connection between the lacrimal sac and the nasal mucosa; see Figs.
3.10a – c) or removal of the
lacrimal sac.
Neonatal Dacryocystitis
Etiology: Approximately 6% of newborns have a stenosis of the mouth of
thenasolacrimal duct due to a persistent
mucosal fold (lacrimal fold or valve of Hasner). The resulting retention of
tear fluid provides ideal growth conditions for bacteria, particularly
staphylococci, streptococci, and pneumococci.
Symptoms and diagnostic considerations: Shortly after birth (usuallywithin two to four
weeks), pus is secreted from the puncta.
The disease con-tinues subcutaneously and pus collects in the palpebral
fissure. The conjunc-tiva is not usually involved.
Differential diagnosis:
❖ Gonococcal conjunctivitis and inclusion conjunctivitis (see
Fig. 4.3).
❖ Silver catarrh (harmless conjunctivitis with slimy mucosal
secretion fol-lowing Credé’s method of prophylaxis with silver nitrate).
Treatment: During the first few weeks,the infant should be monitored forspontaneous opening of the stenosis. During
this period, antibiotic and
anti-inflammatory eyedrops and nose drops (such as erythromycin and
xylo-metazoline 0.5% for infants) are administered.
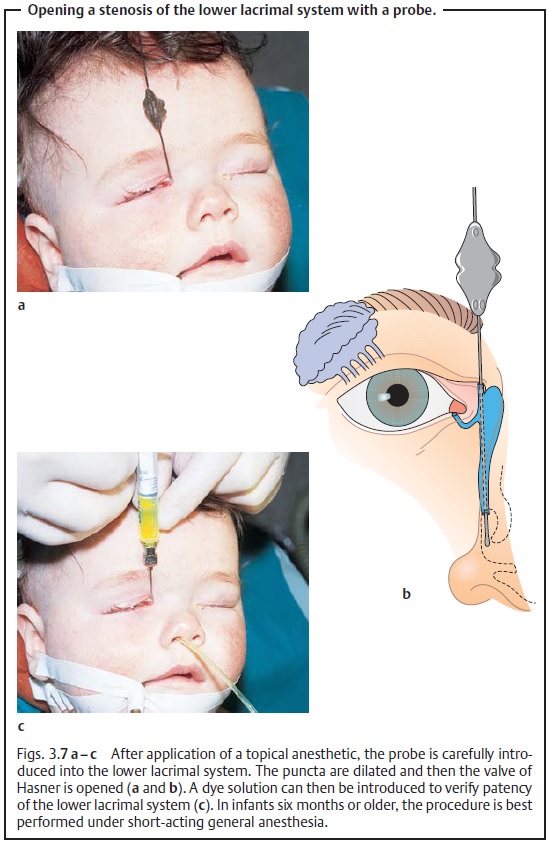
If symptoms persist, irrigationorprobingunder
short-acting general anes-thesia may be indicated (see Figs. 3.7a – c).
Often massaging the region several times daily
while carefully applying pressure to the lacrimal sac will be sufficient to
open the valve of Hasner and eliminate the obstruction.
Canaliculitis
Definition
This usually involves inflammation of the canaliculus.
Epidemiology and etiology: Genuine canaliculitisisrare.Usually
a stricturewill be present and the actual inflammation
proceeds from the conjunctiva. Actinomycetes (fungoid bacteria) often cause
persistent purulent granular concrements that are difficult to express.
Symptoms and diagnostic considerations: The canaliculus region is swol-len, reddened,
and often tender to palpation. Pus or granular concrements can be expressed.
Treatment: The disorder is treated with antibiotic eyedrops and
ointmentsaccording to the specific pathogens detected in cytologic smears.
Successful treatment occasionally requires surgical incision of the
canaliculus.
Tumors of the Lacrimal Sac
Epidemiology: Tumors of the lacrimal sac arerarebut areprimarily
malig-nant when they do occur. They include papillomas, carcinomas, and
sar-comas.
Symptoms and diagnostic considerations: Usually the tumors cause uni-lateral painless
swelling followed by dacryostenosis.
Diagnostic considerations: The irregular and occasionally bizarre form ofthe structure in
radiographic contrast studies is typical. Ultrasound, CT, MRI, and biopsy all
contribute to confirming the diagnosis.
Differential diagnosis: Chronic dacryocystitis (see above), mucocele of theethmoid
cells.
Treatment: The entire tumor should be removed.
Related Topics