Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Infections in the Immunocompromised Patient
Diagnosis and Treatment - Infections in the Immunocompromised Patient
DIAGNOSIS
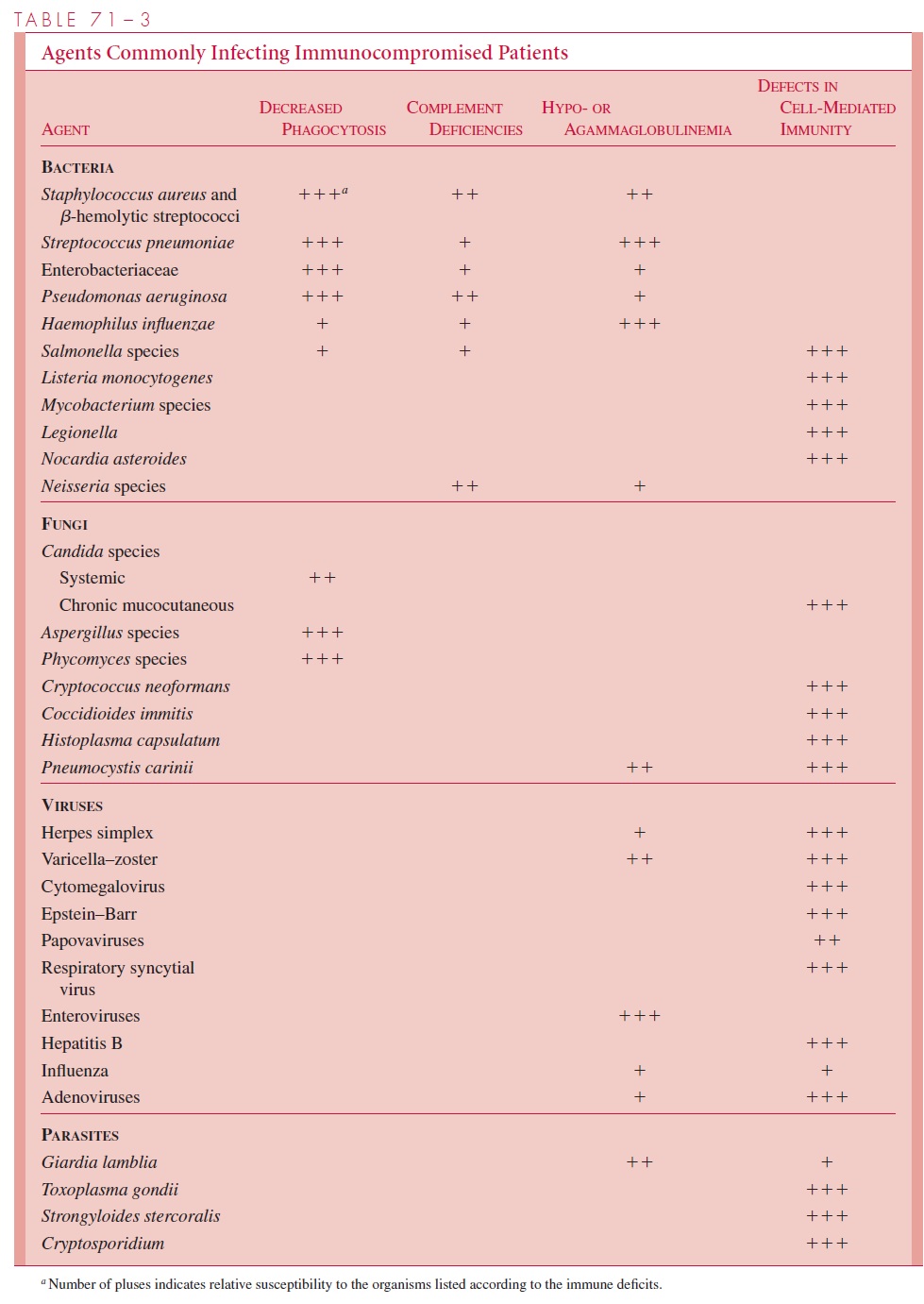
Clinical recognition and treatment of infections in the immunocompromised patient areoften difficult, because the infection may be relatively silent due to impairment of the immune response. Laboratory diagnosis can also be difficult, because many of the organismsinvolved require special culture media and grow slowly (Table 71–3); others such asPneumocystis carinii cannot be grown at all. The increased involvement of low-virulenceorganisms commonly found in the normal flora may make it difficult to distinguish colonizationfrom infection. Thus, isolation of C. albicans from the urine or the pharynx doesnot prove that it is the cause of a concurrent renal abscess or pneumonitis. Diagnosticprocedures such as biopsy of involved organs are often needed to identify the causativeagent.
TREATMENT
Successful treatment of infections in the compromised host depends on recognition of the deficit, early diagnosis, and prompt intervention. This requires identification of the organ-isms most likely to be involved in the infection. The index of suspicion must be very high, because the signs and symptoms of infection that are seen in immunocompetent in-dividuals may be lacking. For example, in neutropenia the clinical signs of infection (eg, abscess formation) may not be apparent when the patient is first seen because of lack of reaction to the disease. It is thus usually necessary to initiate antimicrobic treatment be-fore results of culture and antibiotic susceptibility tests are available. Broad-spectrum an-timicrobic coverage is used initially and replaced with narrower spectrum agents, when the etiologic agent and its susceptibility are known, to reduce the risk of superinfection. In general, bactericidal antimicrobics are needed to control infections when host defenses are inadequate, and with severe infections a combination of synergistic agents may be necessary to provide increased bactericidal action.
Patients with neutropenia have high rates of infection, and mortality may be as high as 20 to 30% if bacteremia develops. Therefore, short-term prophylactic antibiotic treat-ment has been advocated for neutropenic patients and can be effective in preventing infection until the neutrophil count improves. Selection of resistant organisms and “breakthrough” bacteremia as a result of overwhelming infection are major risks of these strategies in these susceptible patients, and the physician must be alert to the possibility of superinfection with other pathogens during treatment.
Neutropenia can be ameliorated by the use of cytokines (eg, granulocyte-colony stim-ulating factor). There is increasing attention to prevention of opportunistic infections in patients disposed to them. For example, patients undergoing bone marrow transplantation may receive prophylactic acyclovir or ganciclovir to prevent herpesvirus and cy-tomegalovirus infection. AIDS patients receive prophylactic trimethoprim – sulfamethoxa-zole to prevent P. carinii pneumonia as well as toxoplasmosis.
Related Topics