Chapter: Essentials of Psychiatry: Psychiatric Classification
DSM-IV-TR Classification and Diagnostic Codes
DSM-IV-TR Classification and
Diagnostic Codes
The “DSM-IV-TR Classification of Mental Disorders’’
refers to the comprehensive listing of the official diagnostic codes,
catego-ries, subtypes and specifiers (see below). It is divided into vari-ous
“diagnostic classes’’ which group disorders together based on common presenting
symptoms (e.g., mood disorders, anxiety disorders), typical age-at-onset (e.g.,
disorders usually first diag-nosed in infancy, childhood and adolescence), and
etiology (e.g., substance-related disorders, mental disorders due to a general
medical condition).
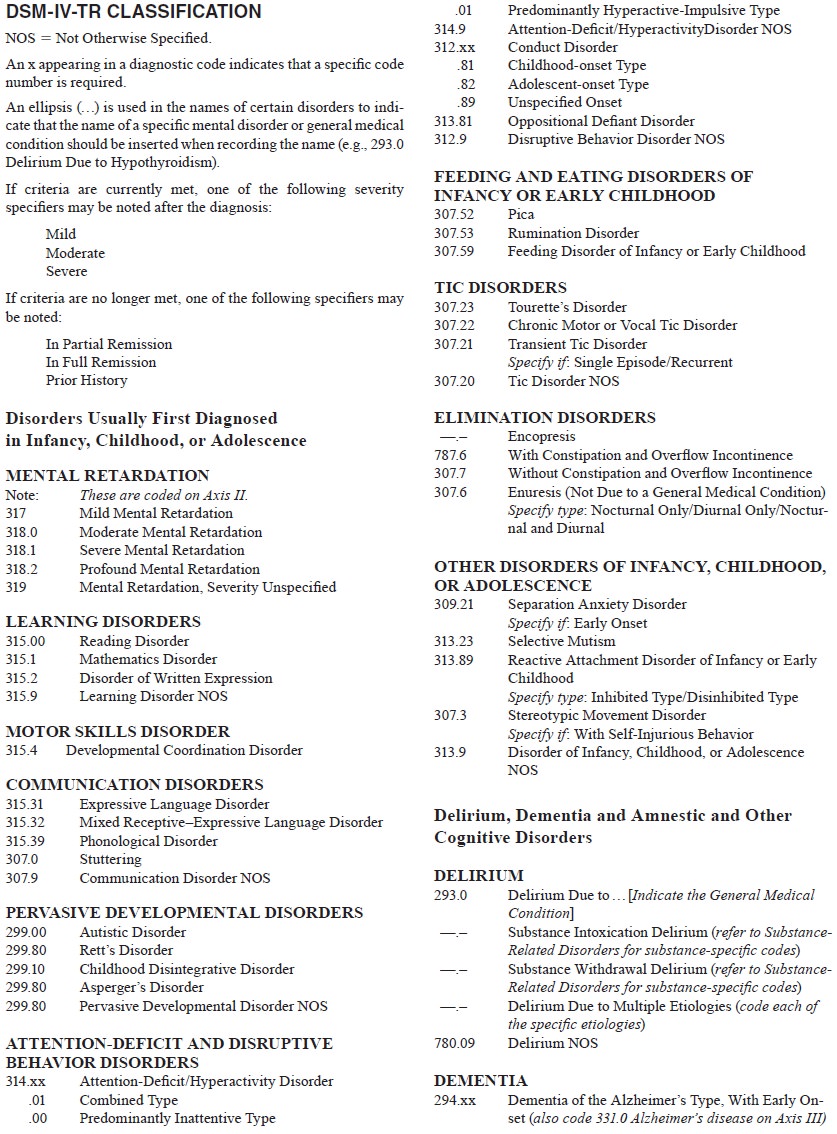
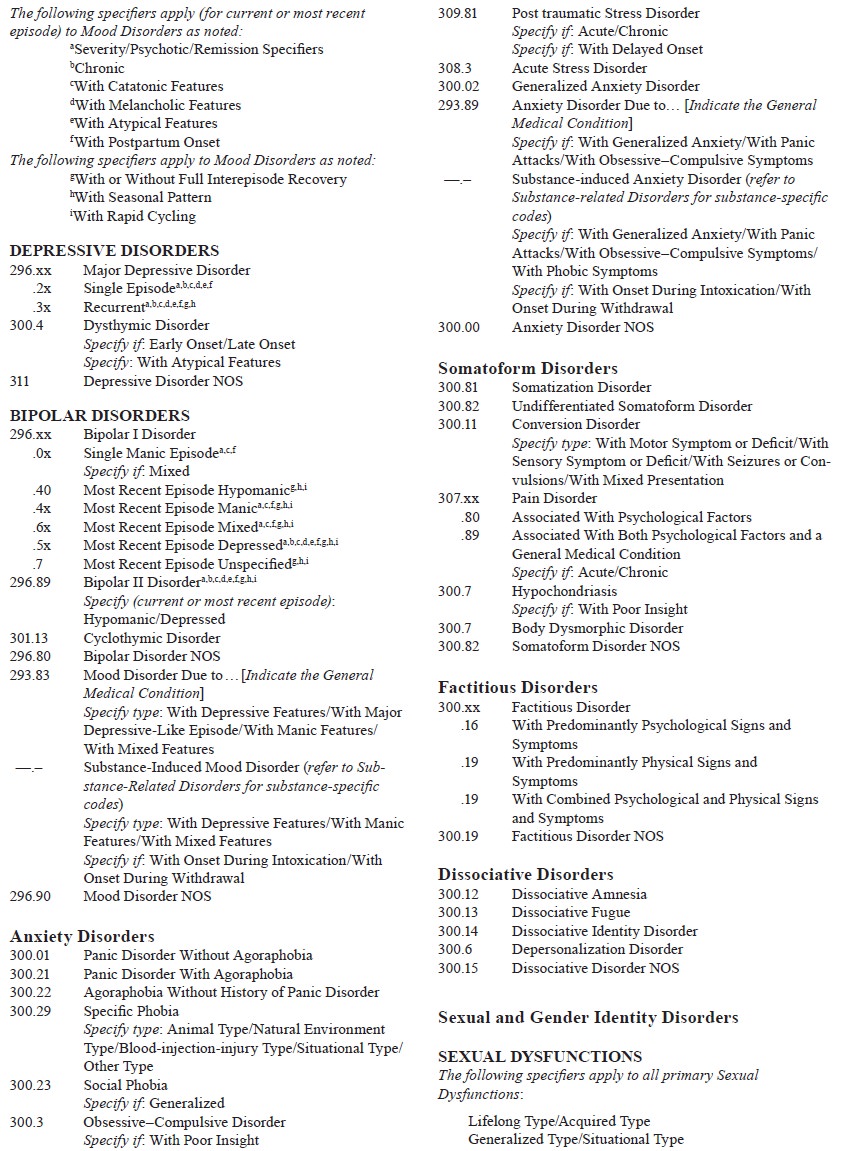
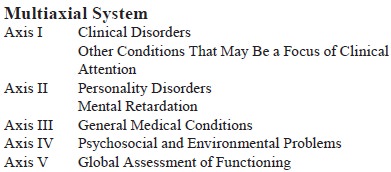
The diagnostic codes listed in the DSM-IV are derived from the International Classifi cation of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), the official coding system for reporting morbidity and mortality in the USA. That is the reason why the codes go from 290.00 to 319.00; they are actually de-rived from the mental disorders section of a much larger coding system for all medical disorders that extends from 001 to 999. Clinicians working in the USA are required to use ICD-9-CM in order to receive reimbursement from both government agencies (e.g., Medicare and Medicaid) and private insurers.
Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence
The classification begins with disorders usually
first diagnosed in infancy, childhood, or adolescence. The provision for a
separate section for so-called childhood disorders is only for convenience.
Although most individuals with these disorders present for clinical attention
during childhood or adolescence, it is not uncommon for some of these
conditions to be diagnosed for the first time in adulthood (e.g.,
attention-deficit/hyperac-tivity disorder). Moreover, many disorders included
in other sections of the DSM-IV have an onset during childhood (e.g., major
depressive disorder). Thus, a clinician evaluating a child or adolescent should
not only focus on those disorders listed in this section but also consider
disorders from throughout the DSM-IV. Similarly, when evaluating an adult, the
clinician should also consider the disorders in this section since many of them
persist into adulthood (e.g., stuttering, learning disorders, tic disorders).
The first set of disorders included in this
diagnostic class (mental retardation, learning and motor skills disorders, and
communication disorders). While they are not, strictly speak-ing, regarded as
mental disorders, they are included in the DSM-IV-TR to facilitate differential
diagnosis and to increase recognition of these conditions among mental health
profes-sionals. Autism and other pervasive developmental disorders are
characterized by gross qualitative impairment in social re-latedness, in
language, and in repertoire of interests and ac-tivities. Disorders covered include
autistic disorder, Asperger’s disorder, Rett’s disorder and childhood
disintegrative disorder. Attention-deficit/hyperactivity disorder and other
disruptive behavior disorders are grouped together because they are all
characterized (at least in their childhood presentations) by dis-ruptive
behavior.
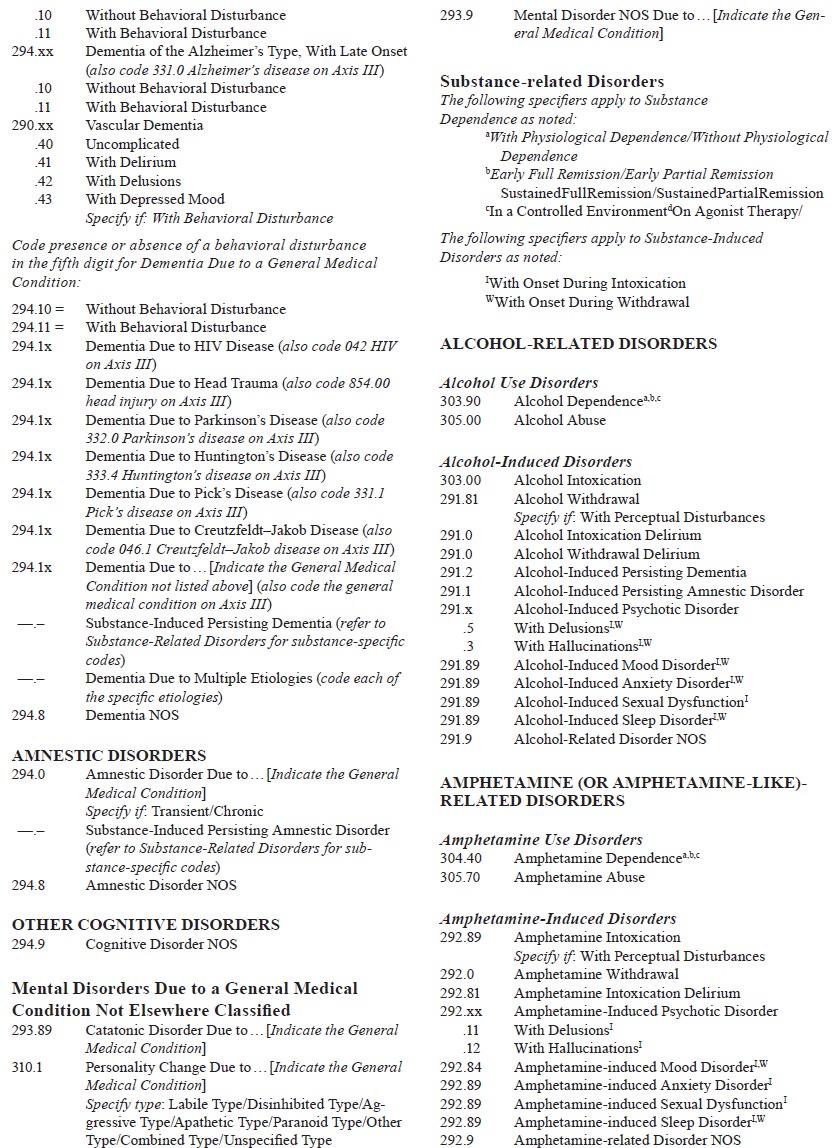
Delirium, Dementia, Amnestic Disorder and Other Cognitive Disorders
In the previous DSM-III-R, delirium, dementia,
amnestic dis-order and other cognitive disorders were included in a section
called “organic mental disorders’’, which contained disorders that were due to
either a general medical condition or substance use. In DSM-IV-TR, the term organic was eliminated because of the
implication that disorders not included in that section (e.g., schizophrenia,
bipolar disorder) did not have an organic compo-nent (Spitzer et al., 1992). In fact, virtually all
mental disorders have both psychological and biological components, and to
des-ignate some disorders as organic and the remaining disorders as nonorganic
reflected a reductionistic mind–body dualism that is at odds with our
understanding of the multifactorial nature of the etiological underpinnings of
disorders.
DSM-IV-TR replaced each unitary organic mental
disor-der (e.g., organic mood disorder) with its two component parts: mood
disorder due to a general medical condition and sub-stance-induced mood
disorder. Because of their central roles in the differential diagnosis of
cognitive impairment, delirium, dementia and amnestic disorder are contained within
the same diagnostic class in DSM-IV-TR.
Whereas both delirium and dementia are
characterized by multiple cognitive impairments, delirium is distinguished by
the presence of clouding of consciousness, which is manifested by an inability
appropriately to maintain or shift attention. DSM-IV-TR includes three types of
delirium: delirium due to a general medical condition, substance-induced
delirium and delirium due to multiple etiologies.
Dementia is characterized by clinically significant
cog-nitive impairment in memory that is accompanied by impair-ment in one or
more other areas of cognitive functioning (e.g., language, executive
functioning). DSM-IV-TR includes several types of dementia based on etiology,
including dementia of the Alzheimer’s type, vascular dementia, a variety of
dementia due to general medical and neurological conditions (e.g., human
immunodeficiency virus infection, Parkinson’s disease), sub-stance-induced
persisting dementia and dementia due to mul-tiple etiologies.
In contrast to dementia, amnestic disorder is
characterized by clinically significant memory impairment occurring in the
ab-sence of other significant impairments in cognitive functioning. DSM-IV-TR
includes amnestic disorder due to a general medical condition and substance-induced
persisting amnestic disease.
Mental Disorders Due to a General Medical Condition Not Elsewhere Classified
This diagnostic class includes all of the specific
mental disorders due to a general medical condition.. In DSM-IV-TR, most of the
mental disorders due to a general medical condition have been distributed
throughout the various diagnostic classes alongside their “nonorganic’’
counterparts in the classification. For exam-ple, mood disorder due to a
general medical condition and sub-stance-induced mood disorder are included in
the mood disorders section of DSM-IV-TR. Two specific types of mental
disorderdue to a general medical condition (i.e., catatonic disorder due to a
general medical condition and personality change due to a general medical
condition) are physically included in this diag-nostic class.
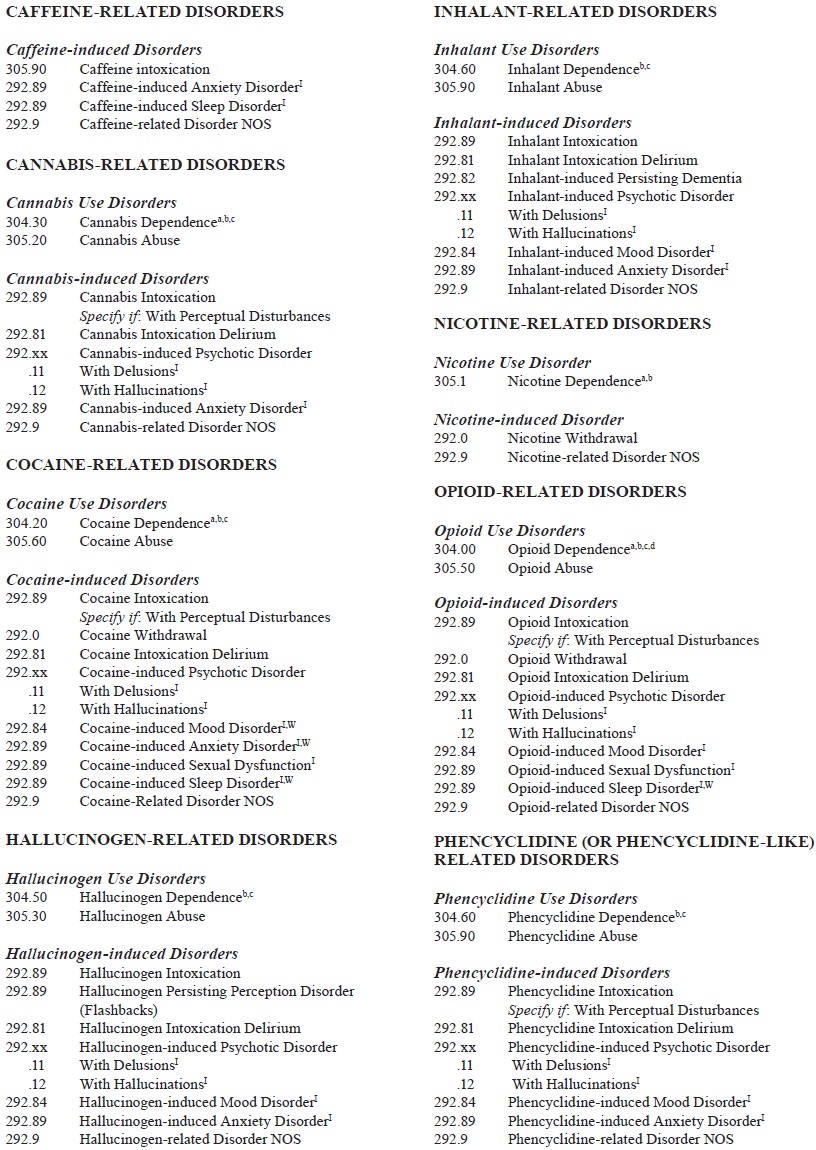
Substance-related Disorders
The term substance
in DSM-IV has a broader meaning than merely a drug of abuse. It also includes
medication side effects and the consequences of toxin exposure. Two types of
substance-related disorders are included in DSM-IV-TR: substance use dis-orders
(dependence and abuse), which describe the maladaptive nature of the pattern of
substance use; and substance-induced disorders, which cover psychopathological
processes caused by the direct effects of substances on the central nervous
system. Criteria sets for substance dependence, substance abuse, sub-stance
intoxication and substance withdrawal that apply across all drug classes are
included before the substance-specific sec-tions of DSM-IV.
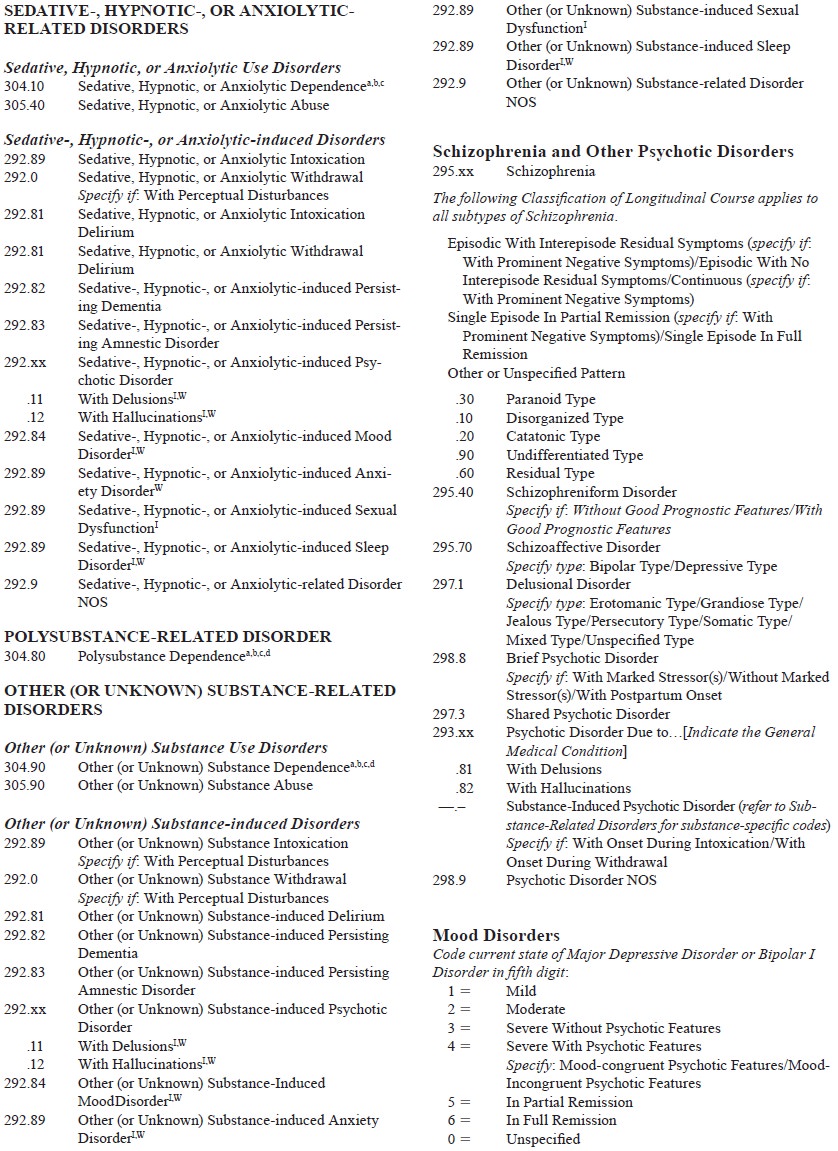
Schizophrenia and Other Psychotic Disorders
The title of this diagnostic class is potentially
misleading for two reasons: 1) there are other disorders that have psychotic
features that are not included in this diagnostic class (e.g., mood disorders
with psychotic features, delirium) and 2) it may incorrectly imply that the
other psychotic disorders included in this section are re-lated in some way to
schizophrenia (which is only true for schizo-phreniform disorder and possibly
schizoaffective disorder). In-stead, what ties together all of the disorders in
this diagnostic class is the presence of prominent psychotic symptoms. Included
here are schizophrenia, schizophreniform disorder, schizoaffec-tive disorder,
delusional disorder, shared psychotic disorder and brief psychotic disorder..
It should be noted that the definition of the term psychosis has been used in different
ways historically and is not even used consistently across the various
categories in the DSM-IV-TR. The most restrictive definition of psychosis (used
in substance-induced psychotic disorder) requires a break in reality testing
such that the person has delusions or hallucinations with no in-sight into the
fact that the delusions or hallucinations are caused by taking drugs.
Mood Disorders
This diagnostic class includes disorders in which
the predomi-nant disturbance is in the individual’s mood. Although the term mood is broadly defined to include
depression, euphoria, anger and
anxiety, the DSM-IV-TR generally restricts mood distur-bances to depressed,
elevated, or irritable mood.
The mood disorders section begins with the criteria
for mood episodes (major depressive episode, manic episode, hy-pomanic episode,
mixed episode), which are the building blocks for the episodic mood disorders.
The codable mood disorders come next and are divided into the depressive
disorders (i.e., major depressive disorder and dysthymic disorder, and the
bi-polar disorders (i.e., bipolar I disorder, bipolar II disorder and
cyclothymic disorder). Finally, the many specifiers that provide important
treatment-relevant information close this section. Several so-called
“subthreshold mood disorders’’ (i.e., they are characterized by depression but
fall short of meeting the diag-nostic criteria for either major depressive
disorder or dysthymicdisorder) are included in DSM-IV-TR appendix B, for Criteria
Sets and Axes Provided for Further Study. These include minor depressive
disorder, brief recurrent depressive disorder, mixed anxiety depressive
disorder, postpsychotic depressive disorder of schizophrenia and premenstrual
dysphoric disorder.
Anxiety Disorders
The common element joining these disparate
categories together is the fact that the anxiety is a prominent part of their
clinical presentation. This grouping has been criticized because of evi-dence
suggesting that at least some of the disorders are likely to be etiologically
distinct from the others. Most particularly, obses-sive–compulsive disorder and
post traumatic stress disorder seem to share little in common with the other
anxiety disorders. In fact, separate diagnostic classes for stress-related
disorders (that would also include adjustment disorders and perhaps
dissocia-tive disorders) and for obsessive–compulsive spectrum disorders (which
might also include trichotillomania, tic disorders, hypo-chondriasis, body
dysmorphic disorder and other disorders char-acterized by compulsive behavior)
have been proposed.
Somatoform Disorders
This diagnostic class includes disorders in which
the defining feature is a physical complaint or bodily concern that is not
better accounted for by a general medical condition or another mental disorder.
These disorders can be divided into three groups based on the focus of the
individual’s concerns: 1) focus on the physical symptoms themselves
(somatization disorder, undifferentiated somatoform disorder, pain disorder and
conversion disorder); 2) focus on the belief that one has a serious physical
illness (hypo-chondriasis); and 3) focus on the belief that one has a defect in
physical appearance (body dysmorphic disorder).
Factitious Disorders
This diagnostic class contains only one disorder:
factitious disorder, which describes presentations in which the individual
intentionally produces or feigns physical or psychological symp-toms in order
to fulfill a psychological need to assume the sick role. Factitious disorder
should always be distinguished from malingering, in which the individual
similarly pretends to have physical or psychological symptoms. The difference
is that in malingering, the person’s motivation is to achieve some external
gain (e.g., disability benefits, lessening of criminal responsibility, shelter
for the night). For this reason, unlike factitious disorder, malingering is not
considered a mental disorder.
Dissociative Disorders
The common element to this group of disorders is
the symptom of dissociation, which is defined as a disruption in the usually
integrated functions of consciousness, memory, identity and per-ception. Four
specific disorders are included: dissociative amne-sia, dissociative fugue,
dissociative identity disorder and deper-sonalization disorder.
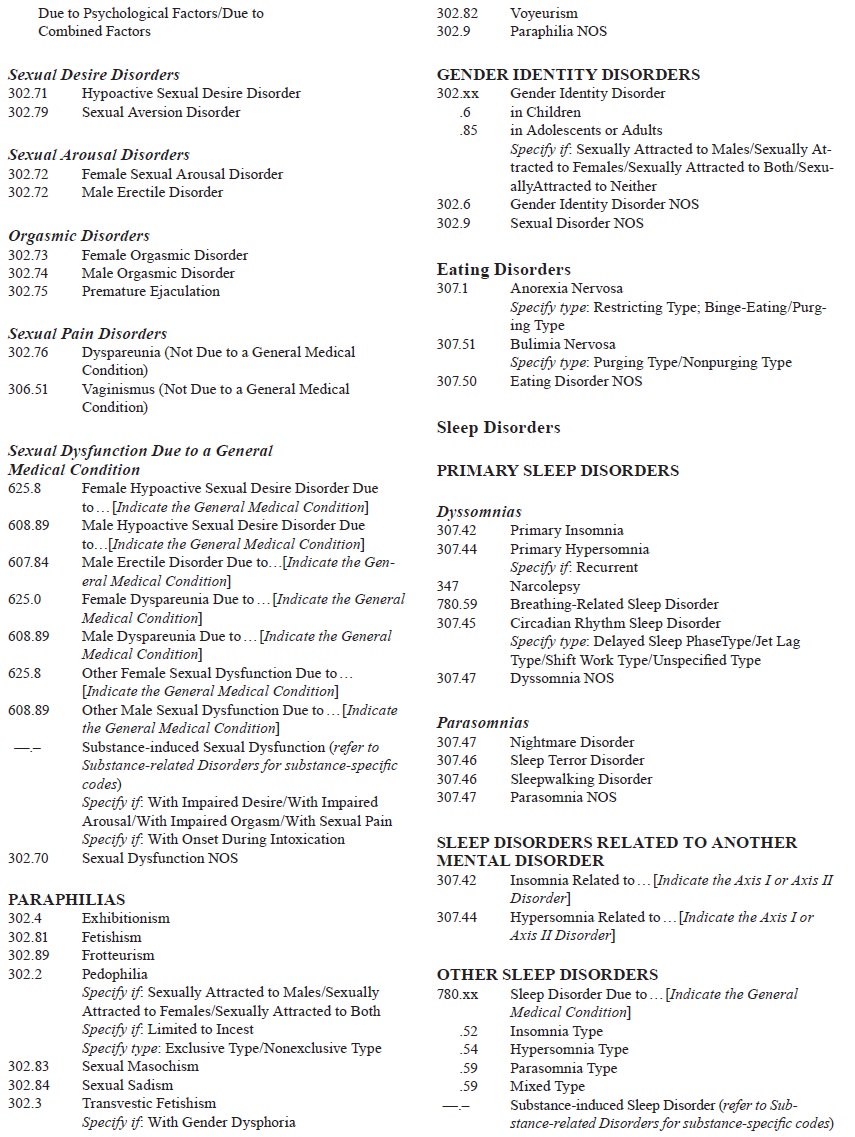
Sexual and Gender Identity Disorders
This diagnostic class contains three relatively
disparate types of disorders, linked together only by virtue of their
involvement in human sexuality. Sexual dysfunctions refer to disturbances in
sexual desire or functioning, paraphilias refer to unusual sexual preferences
that interfere with functioning (or in the case of preferences that involve
harm to others like pedophilia, merely acting on those preferences), and gender
identity disorder refers to a serious conflict between one’s internal identity
of maleness and femaleness (gender identity) and one’s anatomical sexual
characteristics.
Eating Disorders
Although the name of this diagnostic class focuses
on the fact that the disorders in this section are characterized by abnormal
eating behavior (refusal to maintain adequate body weight in the case of
anorexia nervosa and discrete episodes of uncontrolled eating of excessively
large amounts of food in the case of bulimia nervosa), of near equal importance
is the individual’s pathological overem-phasis on body image. A third category,
which is being actively researched but has not been officially added to the
DSM-IV-TR, is binge-eating disorder (included in the appendix of Criteria Sets
and Axes Provided for Further Study). Like bulimia nervosa, in-dividuals with
binge-eating disorder have frequent episodes of binge-eating. However, unlike
bulimia nervosa, these individu-als do not do anything significant to
counteract the effects of their binge-eating (i.e., they do not purge, use
laxatives or diet pills, or excessively exercise).
Sleep Disorders
Sleep disorders are grouped into four sections on
the basis of presumed etiology (primary, related to another mental disor-der,
due to a general medical condition, and substance-induced). Two types of
primary sleep disorders are included in DSM-IV-TR: dyssomnias (problems in
regulation of amount and quality of sleep) and parasomnias (events that occur
during sleep). The dyssomnias include primary insomnia, primary hypersomnia,
circadian rhythm sleep disorder, narcolepsy and breathing-re-lated sleep
disorder, whereas the parasomnias include nightmare disorder, sleep terror
disorder and sleepwalking disorder.
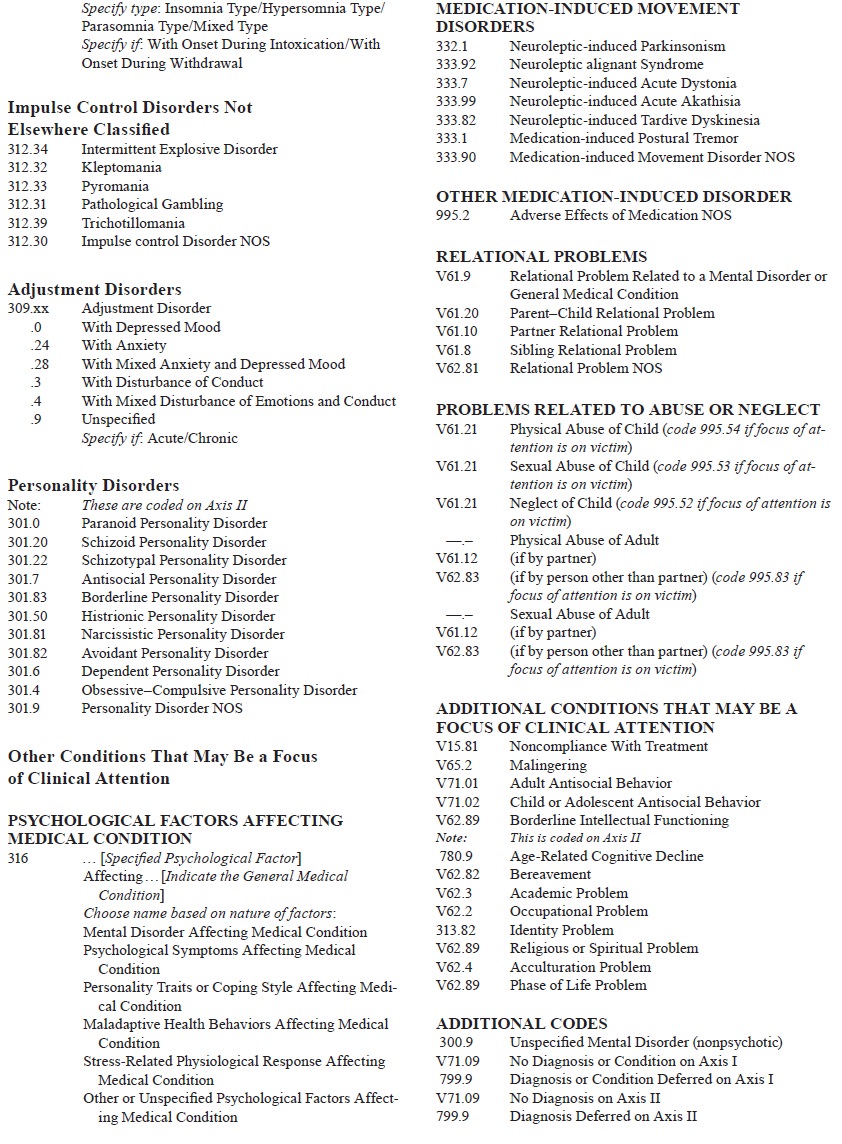
Impulse Control Disorders Not Elsewhere Classified
As is suggested by the title of this diagnostic
grouping, no one diagnostic class in DSM-IV comprehensively includes all of the
impulse control disorders. A number of disorders characterized by impulse
control problems are classified elsewhere (e.g., con-duct disorder,
attention-deficit/hyperactivity disorder, opposi-tional-defiant disorder,
delirium, dementia, substance-related disorders, schizophrenia and other
psychotic disorders, mood disorders, antisocial and borderline personality
disorders). What ties together the disorders in this class is that they present
with clinically significant impulsive behavior and that they are not better
accounted for by one of the mental disorders included in other parts of
DSM-IV-TR. Five such disorders are included here: intermittent explosive
disorder, pathological gambling, pyroma-nia, kleptomania and trichotillomania.
Adjustment Disorders
All DSM-IV categories (except NOS categories) take
priority over adjustment disorder. This category is intended to apply to
maladaptive reactions to psychosocial stressors that do not meet the criteria
for any specific DSM-IV-TR disorder.
Personality Disorders
This diagnostic class is for personality patterns
that significantly deviate from the expectations of the person’s culture, are
perva-sive and lead to significant impairment or distress. Ten specific
personality disorders are included in DSM-IV: paranoid per-sonality disorder
(pervasive distrust and suspiciousness of oth-ers), schizoid personality
disorder (detachment from social re-lationships and a restricted expression of
emotions), schizotypal personality disorder (acute discomfort with close
relationships, perceptual distortions and eccentricities of behavior),
antisocial personality disorder (disregard for the rights of others),
border-line personality disorder (instability of personal relationships,
instability of self-image and marked impulsivity), histrionic per-sonality
disorder (extensive emotionality and attention seeking), narcissistic
personality disorder (grandiosity, need for admira-tion and lack of empathy),
avoidant personality disorder (social inhibition, feelings of inadequacy and
hypersensitivity to nega-tive evaluation), dependent personality disorder
(excessive need to be taken care of), and obsessive–compulsive personality
dis-order (preoccupation with orderliness, perfectionism, and mental and
personal control at the expense of flexibility, openness and efficiency).
Other Conditions That May Be a Focus of Clinical Attention
This section of DSM-IV is for problems that are not
mental disor-ders but that may be a focus of attention for treatment by a
mental health professional. Psychological
factors affecting medical con-dition is intended to allow the psychiatrist
to note the presence of psychological
factors (e.g., Axis I or II disorder) that adversely affect the course of a
general medical condition, including fac-tors that interfere with treatment and
factors that constitute health risks to the individual. Six specific medication-induced movement disorders are also included because of their impor-tance
in treatment and differential diagnosis; five are related to neuroleptic
administration and one (medication-induced postural tremor) is most often
associated with the use of lithium carbon-ate. Although these are best
considered medical conditions, by DSM-IV-TR convention they are coded on Axis
I.
Relational problems include parent–child, partner
and sibling relational problems. Relational problem related to a men-tal
disorder or general medical condition applies to situations in which one member
of the relational unit has a mental disorder or a general medical condition. In
such situations, the relational dynamics can negatively affect the individual’s
condition or vice versa (or both). Problems
related to abuse or neglect (physical abuse, sexual abuse and child
neglect.
Related Topics