Chapter: Medical Surgical Nursing: Perspectives in Transcultural Nursing
Culturally Mediated Characteristics
Culturally Mediated Characteristics
Nurses should be aware
that patients act and behave in a variety of ways, in part because of the
influence of culture on behaviors and attitudes. However, although certain
attributes and attitudes are frequently associated with particular cultural
groups, as de-scribed in the following pages, it is important to remember that
not all people from the same cultural background share the same behaviors and
views. Although the nurse who fails to consider a patient’s cultural
preferences and beliefs is considered insensitive and possibly indifferent, the
nurse who assumes that all members of any one culture act and behave in the
same way runs the risk of stereotyping people. The best way to avoid
stereotyping is to view each patient as an individual and to find out the
patient’s cultural preferences. A thorough culture assessment using a cul-ture
assessment tool or questionnaire (see later discussion) is very beneficial.
SPACE AND DISTANCE
People tend to regard
the space in their immediate vicinity as an extension of themselves. The amount
of space they need between themselves and others to feel comfortable is a
culturally deter-mined phenomenon.
Because nurses and patients usually are not consciously aware of their personal space requirements, they frequently have diffi-culty understanding different behaviors in this regard.
For example, one patient may
perceive the nurse sitting close to him or her as an expression of warmth and
care; another patient may per-ceive the nurse’s act as a threatening invasion
of personal space. Research reveals that people from the United States, Canada,
and Great Britain require the most personal space between themselves and
others, whereas those from Latin America, Japan, and the Middle East need the
least amount of space and feel comfortable standing close to others.
If patients appear to position themselves too close or too far away, the
nurse should consider cultural preferences for space and distance. Ideally,
patients should be permitted to assume a position that is comfortable to them
in terms of personal space and distance. Because a significant amount of
communication during nursing care requires close physical contact, the nurse
should be aware of these important cultural differences and consider them when
de-livering care (Davidhizar, Dowd, & Newman-Giger, 1999).
EYE CONTACT
Eye contact is also a culturally determined behavior. Although most
nurses have been taught to maintain eye contact when speak-ing with patients,
some people from certain cultural backgrounds may interpret this behavior
differently. Some Asians, Native Americans, Indo-Chinese, Arabs, and
Appalachians, for example, may consider direct eye contact impolite or
aggressive, and they may avert their own eyes when talking with nurses and
others whom they perceive to be in positions of authority. Some Native
Americans stare at the floor during conversations, a cultural be-havior
conveying respect and indicating that the listener is paying close attention to
the speaker. Some Hispanic patients maintain downcast eyes as a sign of
appropriate deferential behavior toward others on the basis of age, gender,
social position, economic sta-tus, and position of authority. Being aware that
whether a person makes eye contact may be a result of the culture from which
they come will help the nurse understand a patient’s behavior and pro-vide an
atmosphere in which the patient can feel comfortable.
TIME
Attitudes about time
vary widely among cultures and can be a barrier to effective communication
between nurses and patients. Views about punctuality and the use of time are
culturally deter-mined, as is the concept of waiting. Symbols of time, such as
watches, sunrises, and sunsets, represent methods for measuring the duration
and passage of time (Giger & Davidhizar, 1999; Spector, 2000).
For most health care providers, time and promptness are ex-tremely
important. For example, nurses frequently expect patients to arrive at an exact
time for an appointment, despite the fact that the patient is often kept
waiting by health care providers who are running late. Health care providers
are likely to function accord-ing to an appointment system in which there are
short intervals of perhaps only a few minutes. For patients from some cultures,
how-ever, time is a relative phenomenon, with little attention paid to the
exact hour or minute. Some Hispanic people, for example, consider time in a
wider frame of reference and make the primary distinction between day and
night. Time may also be determined according to traditional times for meals,
sleep, and other activities or events. For people from some cultures, the
present is of the greatest importance, and time is viewed in broad ranges
rather than in terms of a fixed hour. Being flexible in regard to schedules is
the best way to accommodate these differences.
Value differences also
may influence a person’s sense of prior-ity when it comes to time. For example,
responding to a family matter may be more important to a patient than meeting a
sched-uled health care appointment. Allowing for these different views is
essential in maintaining an effective nurse-patient relationship. Scolding or
acting annoyed at a patient for being late undermines the patient’s confidence
in the health care system and might re-sult in further missed appointments or
indifference to health care suggestions.
TOUCH
The meaning people associate with touching is culturally deter-mined to
a great degree. In some cultures (eg, Hispanic, Arab), male health care
providers may be prohibited from touching or examining certain parts of the
female body. Similarly, it may be inappropriate for females to care for males.
Among many Asian Americans, it is impolite to touch a person’s head because the
spirit is believed to reside there. Therefore, assessment of the head or
evaluation of a head injury requires alternative approaches. The patient’s
culturally defined sense of modesty must also be considered when providing nursing
care. For example, some Jew-ish and Islamic women believe that modesty requires
covering their head, arms, and legs with clothing.
COMMUNICATION
Many aspects of care may be influenced by the diverse cultural
perspectives held by the health care providers, patient, family, or significant
others. One example is the issue of informed consent and full disclosure. In
general, a nurse may argue that patients have the right to full disclosure
about their disease and prognosis and may feel that advocacy means working to
provide that dis-closure. Family members of some cultural backgrounds may
be-lieve it is their responsibility to protect and spare the patient, their
loved one, the knowledge of a terminal illness. Similarly, patients may, in
fact, not want to know about their condition and may ex-pect their family
members to “take the burden” of that knowl-edge and related decision-making
(Kudzma, 1999). The nurse should not decide that the family or patient is
simply wrong or that the patient must know all details of his or her illness.
Simi-lar concerns may be noted when patients refuse pain medication or
treatment because of cultural beliefs regarding pain or belief in divine
intervention or faith healing. Determining the most ap-propriate and ethical
approach to patient care requires an explo-ration of the cultural aspects of
these situations. Self-examination by the nurse and recognition of one’s own
cultural bias and world view, as discussed earlier, will play a major part in
helping the nurse to resolve cultural and ethical conflicts. The nurse must
promote open dialogue and work with the patient, family, physi-cian, and other
health care providers to reach the culturally ap-propriate solution for the
patient.
OBSERVANCE OF HOLIDAYS
People from all cultures
celebrate civil and religious holidays. Nurses should familiarize themselves
with major holidays for members of the cultural groups they serve. Information
about these important celebrations is available from various sources, including
religious organizations, hospital chaplains, and patients themselves. Routine
health appointments, diagnostic tests, surgery, and other major procedures
should be scheduled to avoid those holidays a patient identifies as
significant. Efforts should also be made to accommodate patients and family or
significant others, when not contraindicated, as they perform holiday rituals
in the health care setting.
DIET
The cultural meanings associated with food vary widely but usu-ally
include one or more of the following: relief of hunger; pro-motion of health
and healing; prevention of disease or illness; expression of caring for
another; promotion of interpersonal closeness among individuals, families,
groups, communities, or nations; and promotion of kinship and family alliances.
Food may also be associated with solidification of social ties; celebra-tion of
life events (eg, birthdays, marriages, funerals); expression of gratitude or
appreciation; recognition of achievement or ac-complishment; validation of
social, cultural, or religious ceremo-nial functions; facilitation of business
negotiations; and expression of affluence, wealth, or social status.
Culture determines which
foods are served and when they are served, the number and frequency of meals,
who eats with whom, and who is given the choicest portions. Culture also
determines how foods are prepared and served; how they are eaten (with
chopsticks, hands, or fork, knife, and spoon); and where people shop for their
favorite food items (eg, ethnic grocery stores, spe-cialty food markets).
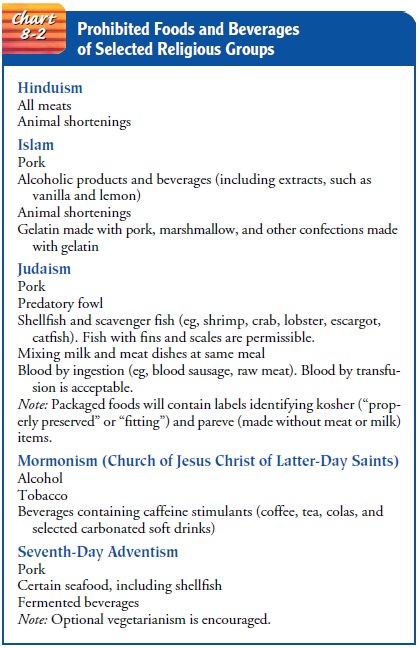
Religious practices may include fasting (eg, Mormons, Catholics,
Buddhists, Jews, Muslims), abstaining from selected foods at particular times
(eg, Catholics abstain from meat on Ash Wednesday and on Fridays during Lent),
and considerations for medications (eg, Muslims may prefer to use
non-pork-derived in-sulin). Practices may also include the ritualistic use of
food and beverages (eg, Passover dinner, consumption of bread and wine during
religious ceremonies). Chart 8-2 summarizes some dietary practices of selected
religious groups.
Many groups tend to feast, often in the company of family and friends, on selected holidays. For example, many Christians eat large dinners on Christmas and Easter and consume other traditional high-calorie, high-fat foods, such as seasonal cookies, pastries, and candies. These culturally-based dietary practices are especially significant in the care of patients with diabetes, hy-pertension, gastrointestinal disorders, and other conditions in which diet plays a key role in the treatment and health mainte-nance regimen.
BIOLOGIC VARIATIONS
Along with psychosocial adaptations, nurses must also consider the
physiologic impact of culture on patient response to treat-ment, particularly
medications. Data have been collected for many years regarding differences in
the effect some medications have on persons of diverse ethnic or cultural
origins. Genetic predispositions to different rates of metabolism cause some
pa-tients to be prone to overdose reactions to the “normal dose” of a
medication, while other patients are likely to experience a greatly reduced
benefit from the standard dose of the medication. An antihypertensive agent,
for example, may work well for a white male client within a 4-week time span but
may take much longer to work or not work at all for an African-American male
patient with hypertension. General polymorphism—variation in response to
medications resulting from patient age, gender, size, and body composition—has
long been acknowledged by the health care community (Kudzma, 1999). Culturally
competent medication administration requires that consideration of ethnicity
and related factors such as values and beliefs regarding the use of herbal
sup-plements, dietary intake, and genetic factors can affect the effec-tiveness
of treatment and compliance with the treatment regimen (Giger & Davidhizar,
1999; Kudzma, 1999).
COMPLEMENTARY AND ALTERNATIVE THERAPIES
Interventions for
alterations in health and wellness vary among cultures. Interventions most
commonly used in the United States have been labeled as conventional medicine by the Na-tional Institutes of Health (n.d.).
Other names for conventional medicine were allopathy, Western medicine, regular
medicine, mainstream medicine, and biomedicine. Interest in interven-tions that
are not an integral part of conventional medicine prompted the National
Institutes of Health to create the Office of Alternative Medicine (OAM) in
1992, and then to establish the National Center for Complementary and Alternative
Med-icine (NCCAM) in 1999.
The NCCAM grouped
complementary and alternative med-icine interventions into five main
categories: alternative medical systems, mind–body interventions, biologically
based therapies, manipulative and body-based methods, and energy therapies
(National Institutes for Health, National Center for Comple-mentary and
Alternative Medicine, accessed 9/8/01).
· Alternative medical
systems are defined as complete systemsof theory and
practice that are different from conventional medicine. Some examples are
traditional Eastern medicine (including acupuncture, herbal medicine, oriental
massage, and Qi gong); India’s traditional medicine, Ayurveda (in-cluding diet,
exercise, meditation, herbal medicine, mas-sage, exposure to sunlight, and
controlled breathing to restore harmony of an individual’s body, mind, and
spirit); homeo-pathic medicine (including herbal medicine and minerals); and
naturopathic medicine (including diet, acupuncture, herbal medicine,
hydrotherapy, spinal and soft-tissue ma-nipulation, electrical currents,
ultrasound and light therapy, therapeutic counseling, and pharmacology).
· Mind–body interventions are defined as techniques to facilitatethe mind’s ability to affect
symptoms and bodily functions. Some examples are meditation, dance, music, art
therapy, prayer, and mental healing.
· Biologically based
therapies are defined as natural and bio-logically
based practices, interventions, and products. Some examples are herbal
therapies (an herb is a plant or plantpart that produces and contains chemical substances
that act upon the body), special diet therapies (such as those of Drs. Atkins,
Ornish, and Pritikin), orthomolecular thera-pies (magnesium, melatonin,
megadoses of vitamins), and biologic therapies (shark cartilage, bee pollen).
· Manipulative and body-based methods are defined as
inter-ventions based on body movement. Some examples are chi-ropracty
(primarily manipulation of the spine), osteopathic manipulation, massage
therapy (soft tissue manipulation), and reflexology.
· Energy therapies are defined as interventions that focus
onenergy fields within the body (biofields) or externally (elec-tromagnetic
fields). Some examples are Qi gong, Reiki, therapeutic touch, pulsed
electromagnetic fields, magnetic fields, alternating electrical current, and
direct electrical current.
A patient may choose to seek an alternative to conventional medical or
surgical therapies. Many of these alternative therapies are becoming widely
accepted as feasible treatment options. Therapies such as acupuncture and
herbal treatments may be rec-ommended by a patient’s physician to address
aspects of a condi-tion that are unresponsive to conventional medical treatment
or to minimize side effects associated with conventional medical therapy. Alternative
therapy used to supplement conventional medicine may be referred to as complementary therapy.
Physicians and advanced
practice nurses may work in collab-oration with an herbalist or with a
spiritualist or shaman to pro-vide a comprehensive treatment plan for the
patient. Out of respect for the way of life and beliefs of patients from
different cultures, it is often necessary that the healers and health care
providers respect the strengths of each approach (Palmer, 2001). Complementary
therapy is becoming more common as health care consumers become more aware of
what is available through information in printed media and on the Internet.
As patients become more
informed, they are more likely to participate in a variety of therapies in
conjunction with their con-ventional medical treatments. The nurse needs to
assess each pa-tient for use of complementary therapies, remain alert to the
danger of conflicting treatments, and be prepared to provide information to the
patient regarding treatment that may be harmful. The nurse must, however, be
accepting of the patient’s beliefs and right to control his or her own care. As
a patient advocate, the nurse facili-tates the integration of conventional
medical, complementary, and alternative medical therapies.
Related Topics