Chapter: Modern Medical Toxicology: Cardiovascular Poisons: Cardiotoxic Plants
Common Oleander - Cardiotoxic Plant

![]() Common
Oleander
Common
Oleander
Other Common Names
White oleander, Pink oleander, Rose laurel, Rose bay, Rosa
francesca, Laurier rose, Adelfa.
Botanical Name
Nerium
oleander
Physical Appearance
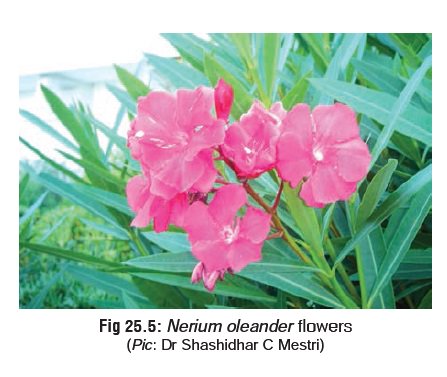
This plant belonging to family Apocynaceae is a large
evergreen ornamental shrub with long lanceolate leaves and clusters of whitish
or pinkish flowers (Fig 25.4 and Fig 25.5). The leaves produce a clear,
thick sap.

Toxic Part
All parts, especially the root.
Toxic Principles
The seeds, stem, and root are rich in the following cardiac
glycosides: oleandrin, neriin, folinerin, rosagenin, and digi-toxigenin.
Uses
·
Decoction of the leaves and root are
used in Indian tradi-tional medicine as local applications for various skin
ailments.
·
Root is used by rural folk as
abortifacient.
·
Common oleander is a popular
ornamental garden plant.
Usual Fatal Dose
· About 5 to 15 leaves
· About 15 grams of root.
Serious
poisoning rarely develops after “taste” ingestions of whole plant material by
children. Taste/exploratory ingestions of Nerium
oleander are unlikely to result in toxicity.
Mode of Action
All
the glycosides have digoxin-like effects; they inhibit sodium-potassium ATPase.
Clinical Features
Symptoms generally begin within 10 to 20 minutes of
inges-tion. A tingling or burning sensation in the fingers and toes is usually
seen first, followed by sweats and chills, a generalised paraesthesia, dryness
of mouth, and numbness. The following are seen:
·
GIT:
Nausea, vomiting, diarrhoea. Numbness of tongueoccurs sometimes.
·
CVS:
Increased ectopy and conduction delay
(bradycardia,supraventricular tachycardia with AV block), electrolyte
imbalances (especially hyperkalaemia) and hypotension/ hypertension.
Ventricular fibrillation is potentially lethal. Decreased QRS-T interval, T
wave flattening/inversion, irregular ventricular rate, and increased PR
interval, etc., have also been reported. Smoke from a burning oleander plant
can cause dizziness, vomiting, and cardiac arrhyth-mias.
·
CNS:
Delirium, lethargy, dizziness, drowsiness.Occasionally there
may be seizures, and coma.
Diagnosis
·
Because oleander-derived cardiac
glycosides are cross-reactive with the frequently used radio-immunoassays for
digoxin, an elevated level may help confirm suspicion of oleander poisoning.
·
Thin-layer chromatography and
fluorescence spectropho-tometry can also be used to identify oleander
glycosides.
·
Reverse-phase HPLC and HPLC/MS are
more specific.
Treatment
·
All patients with a history of
cardiac glycoside-containing plant ingestion should have a baseline ECG and
electrolytes. Patients who at presentation show signs of toxicity, independent
of the dose ingested, should be admitted to the ICU for at least 24 hours of
observation and treatment.
·
Gastric lavage, activated charcoal: Gastric lavage is of
limited benefit in patients ingesting plant parts, particularly children,
because of the size of the plant parts relative to the lavage tube. Also, the
procedure may worsen bradycardia secondary to vagal stimulation. Whole gut
lavage may be more useful in such situations.
· IV fluids.
· Careful measurement of serum
potassium is one of the most important laboratory tests to be done, since
hyperkalaemia is quite common. The emergency management of life-threatening
hyperkalaemia (potassium levels greater than 6.5 mEq/L) includes IV
bicarbonate, glucose, and insulin (administer 0.2 unit/kg of regular insulin
with 200 to 400 mg/kg glucose). Concurrent administration of IV sodium
bicarbonate (about 1 mEq/kg) is of additive value in rapidly lowering serum
potassium levels.
· Atropine for sinus bradycardia and
AV block: 1 mg IV; repeat in 3 to 5 minutes if asystolic cardiac arrest
persists. 3 mg (0.04 mg/kg) IV is generally considered to be a fully vago-lytic
dose in most adults. Insertion of a pacemaker should be considered in those
patients with severe bradycardia, and/ or slow ventricular rate due to second
degree AV block who fail to respond to atropine (and/or phenytoin).
· Antiarrhythmics (e.g. lignocaine):
Lignocaine is useful in the management of ventricular tachy-arrhythmias, PVCs,
and bigeminy.
· Digoxin-specific Fab fragment
therapy is said to be effec-tive. Treatment with Fab fragments should be
considered in those severely intoxicated patients who fail to respond to
immediately available conventional therapy.
· Haemodialysis is ineffective in
removing cardiac glyco-sides, but may assist in restoring serum potassium to
normal levels.
Forensic Issues
·
Accidental poisoning from its use in
traditional medicine. Suicidal ingestion of decoction prepared from leaves or
root is fairly common in rural areas.
·
Homicidal cases are rare, but have
been reported. In one attempeted case of murder, a middle-aged male presented
to the ED with a two-month history of nausea, anorexia, colicky abdominal pain,
vomiting, diarrhoea, lethargy, confusion, dry mouth, dizziness, paraesthesias,
tremor, and episodes of slurred speech with blurred, yellowish vision.
Subsequent police investigation revealed that the wife was attempting to poison
him by using water boiled with roots of Nerium
oleander for making coffee over an eight-week period.
Related Topics