Chapter: Essentials of Psychiatry: Cognitive and Behavioral Therapies
Cognitive and Behavioral Treatment Strategies
Cognitive
and Behavioral Treatment Strategies
The
cognitive and behavioral therapies are well known for their use of specific
treatment techniques. Commonly used CBT procedures are directly linked to the
theoretical constructs and empirical research of this school of therapy.
Although techniques are given somewhat more emphasis in CBT than in other forms
of psychotherapy, there is still considerable room for therapists to be
creative and flexible in developing a treatment plan. In fact, nov-ice
therapists sometimes focus too much on applying techniques at the expense of
nurturing the therapeutic alliance and case for-mulation. Development of a
productive therapeutic relationship and an individualized case conceptualization
should always take precedence over the implementation of specific cognitive or
be-havioral techniques. A number of the more important CBT strat-egies are
described briefly here. More detailed accounts of CBT interventions can be
found elsewhere (Beck et al., 1979;
Beck 1995; Barlow and Cerny, 1988; Freeman et
al., 1989; Persons, 1989).
Collaborative Empiricism
The
therapeutic relationship is as important in CBT as in any of the other
effective psychotherapies. However, interchanges be-tween therapist and patient
often differ from those observed in supportive or dynamically oriented
treatment. One difference is that the therapist is responsible for managing the
pace of the ses-sion and uses an agenda to help make each session as efficient
as possible. Cognitive–behavioral therapists strive for a therapeutic
relationship that emphasizes: 1) a high degree of collaboration and 2) a
scientific attitude toward testing the validity or usefulness of particular
cognitions and behavior. This therapeutic stance is re-ferred to as
collaborative empiricism. The empirical nature of the relationship reflects
that therapist and patient work together as an investigative team to develop
hypotheses about cognitive or be-havioral patterns, examine data, and explore
alternative ways of thinking or behaving. At first, therapists usually spend
more time teaching and explaining in CBT than in other forms of therapy, yet in
the course of therapy, patients are actively engaged to be-come increasingly
involved in the work of treatment.
The
collaborative empirical stance requires that the thera-pist and patient work
together to make an honest appraisal
of the validity of cognitions as well as of the adaptive or maladaptive nature
of beliefs and behaviors. If a negative assessment proves to be accurate (e.g.,
the patient actually has made serious mistakes, the individual’s spouse is
highly likely to leave, or the patient has engaged in a repetitive
self-defeating behavior pattern), then the therapist and patient need to work
together in a problem-solving mode to develop a plan to cope with the problems
at hand or prac-tice more adaptive strategies for use in the future.
Wright
and Beck (1994) and others (Clark et al.
1999) have recommended several strategies for enhancing collaborative
empiricism. These include: 1) adjusting the therapist’s level of activity to
match the patients’ symptom severity or the phase of treatment; 2) encouraging
use of self-help procedures; 3) attend-ing to the “nonspecific” variables
important in all therapeutic relationships (e.g., empathy, respect, equanimity,
kindness and good listening skills); 4) promoting frequent two-way feedback; 5)
devising coping strategies to help deal with real losses or im-plementing a
plan of action to address maladaptive behavior; 6) recognizing transference
phenomena; 7) customizing thera-peutic interventions; and 8) using humor
judiciously. It is also important to recognize and account for the wide variety
of indi-vidual differences in cultural backgrounds, social attitudes and
expectations that each patient brings to the therapy encounter (Wright and
Davis, 1994).
Psychoeducation
Most
forms of CBT integrate explicit psychoeducational proce-dures as a core element
of the treatment process. Psychoeduca-tional procedures are typically blended
into treatment sessions in a manner that de-emphasizes formal teaching. There
is a con-certed effort to teach the patient why it is important to challenge
automatic thoughts, identify cognitive errors and practice imple-menting a more
rational thinking style. Behavioral interventions are also preceded by
psychoeducation to convey the background for principles such as extinction,
reinforcement, self-monitoring, exposure and response prevention.
In the
early phases of treatment, special attention is paid to socializing the patient
to CBT. The basic cognitive–behavioral model is demonstrated, and expectations
for both patient and ther-apist are conveyed. Some of the frequently used
psychoeducational procedures in CBT include brief, impromptu explanations
(often written on a chalkboard or a pad of paper to increase the chances of
comprehension and retention) and reading assignments, such as Coping with Depression (Beck and
Greenberg, 1974), Feel-ing Good (Burns,
1980), Mind Over Mood (Greenberger
and Padesky, 1995) or Getting Your Life Back (Wright and
Basco, 2001). Psychoeducational initiatives typically become more com-plex as
therapy proceeds. For example, detailed explanations and repeated exercises may
be needed before the patient fully grasps abstract concepts such as
attributional style or schemas. As ther-apy progresses, homework assignments
continue explicitly to re-inforce material covered during therapy sessions.
Modifying Automatic Thoughts
The first
step in changing automatic thoughts is to help the patient recognize when she
or he is having them. The therapist is oftenable to illustrate the presence of
automatic negative thoughts dur-ing the initial session by gently calling
attention to a change in the patient’s mood. Such “mood shifts” can be
excellent learning experiences that give personally relevant illustrations of
the link-age between cognitions and feelings.
One
common misconception of CBT is that its practition-ers disregard the role of
affect or feelings in the etiology and treatment of psychiatric disorders.
Actually, one of the principal components of CBT is the stimulation and
modulation of emotion (see Figure 69.3). In fact, Beck referred to emotion as
“the royal road to cognition” (Beck, 1991). In contrast to experiential
thera-pies, variations in emotion are used in CBT to establish links with
cognition and identify errors in information processing. Getting in touch with
feelings is thus not a goal in CBT but only a means by which therapy helps
patients to gain greater control over the processes that influence their moods
and behaviors.
Socratic Questioning
The most
frequently used technique to uncover and modify au-tomatic negative thoughts is
Socratic questioning (or guided discovery) (Beck et al., 1979; Overholser, 1993a, 1993b, 1993c). Socratic
questioning teaches the use of rationality and inductive reasoning to challenge
whether what is thought or felt is actu-ally true. The therapist models the use
of Socratic questioning and encourages the patient to start raising questions
about the validity of his or her thinking. There are few formal guidelines for
Socratic questioning (Overholser, 1993a). Rather, therapists learn to use their
experience and ingenuity to frame good ques-tions that engage the patient in a
process aimed at recognizing and modifying a biased or distorted cognitive
style. Typical ques-tions include: What ran through your mind at that time?
What is the evidence that your impression is accurate? Could there be any
alternative explanations? If this were true, what would be the worst thing that
would happen? When guided discovery methods are not sufficient to draw out
automatic thoughts, the therapist may turn to several alternative ways of
eliciting dysfunctional cognitions, as described in the following.
Imagery Techniques and Role-playing
Imagery
techniques and role-playing are used when direct ques-tioning does not fully
reveal important underlying cognitions. When imagery is used, the therapist
sets the scene by asking the patient to visualize the situation that caused
distress. Although some patients can readily imagine themselves in a previous
scene, many need prompts or imagery induction to encourage their ac-tive
participation in the exercise. Several types of questions can be used to help
frame the scene. These include inquiries about: 1) the physical details of the
setting, 2) occurrences immediately before the interaction, and 3) descriptions
of the other people in the scene (Wright and Beck, 1994). In role-playing
exercises, the therapist and patient act out an interpersonal vignette to
uncover automatic thoughts or to try out a revised pattern of thinking. This
technique is used less frequently than imagery by most cog-nitive–behavioral
therapists and may be reserved for situations in which transference distortions
are unlikely (Wright and Beck, 1994).
Thought Recording
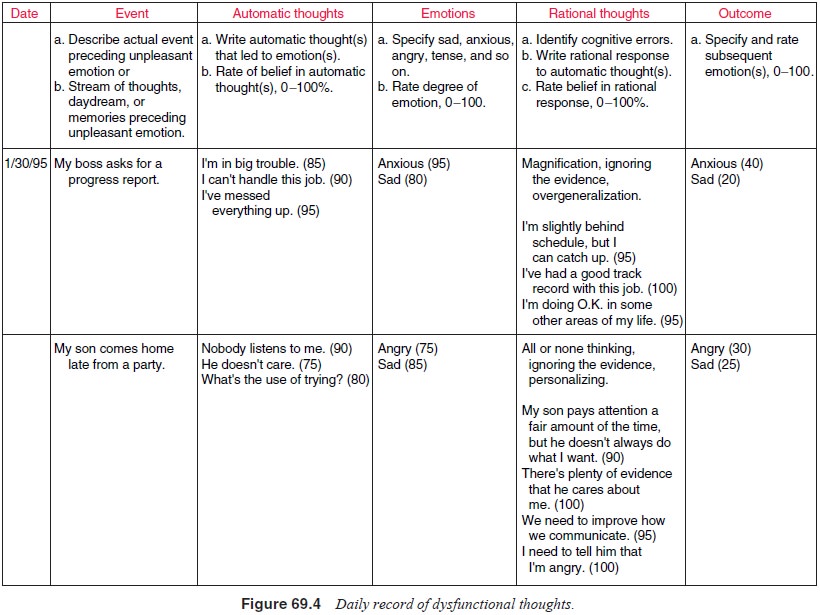
Thought
recording is one of the most useful procedures for iden-tifying and changing
automatic thoughts. This technique is first presented in relatively simple two-
or three-column versions in the early stages of therapy. When the two-column
procedure is used, patients are instructed to write down events in one column
and thoughts in the other. Alternatively, they can record events, thoughts and
emotions in the three columns. The purpose of this exercise is to encourage
patients to begin to use self-monitoring to increase awareness of their thought
patterns. Next, the strength of the emotion and the believability of the
automatic negative thoughts are rated on a scale of 0 to 100. In subsequent
sessions, a more complex five-column thought record, the Daily Record of
Dysfunctional Thoughts (DRDT) is introduced (Figure 69.4). The fourth column of
the DRDT encourages the patient to develop rational alternatives that rebut the
automatic negative thoughts; the fifth column is used for a reevaluation of the
mood and cog-nitive ratings. Work on identifying cognitive errors can also be
included in this form of thought recording.
Examining the Evidence
The
examining the evidence procedure is a collaborative exercise used to test the
validity of automatic negative thoughts. Cogni-tions are set forth as
hypotheses rather than established facts. The patient is encouraged to write
down evidence that either supports or refutes the automatic thought using a
two-column form (i.e., pros and cons). Cognitive errors such as magnification,
person-alization and all-or-nothing thinking are frequently revealed in these
situations.
Next, the
therapist helps to guide revision of the auto-matic negative thought in light
of the evidence (e.g., “I often feel
inferior to others, even when there’s no good evidence that they feel that way”
or “I have had a number of difficulties with my teachers and employers, but not
all relationships have been bad”). The process thus moves from the patient’s
general and globally negative interpretations to more specific, factually based
statements.
When an honest
appraisal uncovers evidence in support of negative cognitions, the therapist
may choose to focus on the patient’s attributions of causality or internality.
The patient who posits a negative attribution for poor work evaluation (e.g.,
“My performance was poor because I don’t have what it takes”) can usually be
aided to consider a more neutral attribution (e.g., “My performance was poor
because I was underprepared…my depression also prevented more energetic
preparation”). The treatment plan may also be revised to develop better methods
of coping in similar situations or to work on ways of remedi-ating skill
deficits. Sometimes, particular difficulties cannot be changed (e.g., physical
handicaps, markedly unattractive physi-cal looks, or severe financial
limitations).
Generating Alternatives
If automatic thoughts prove to be largely dysfunctional, the pa-tient is encouraged to generate alternatives that are more accu-rate or factual. Many of the techniques discussed earlier can be used to help generate alternatives to automatic thoughts. Socratic questioning is used in therapy sessions to help the patient start to think more creatively. Also, psychoeducational procedures may be employed to teach brainstorming techniques. For exam-ple, the patient may be taught to use “expert testimony” or the opinions of someone who knows her or him well (i.e., a sibling, spouse, or best friend) to help develop more rational alterna-tives. Thought records are often used to record alternatives to automatic thoughts. We often encourage patients to collect their thought records in notebook form for ongoing use. Figure 69.4 illustrates the use of rational alternatives during CBT for a de-pressed patient.
Many
patients with depression, anxiety and related conditions have relatively rigid
cognitive styles that perpetuate dysfunctional thought and behavior patterns.
These individu-als frequently experience “second-order” automatic negative
thoughts, that is, negative thoughts that are triggered by rational
alternatives (“that’s a cop-out…quit making excuses”). These thoughts about
thoughts tend to undermine the credibility of the rational responses and may
dampen the patient’s enthusiasm for using the procedure. The therapist may
notice a particular facial expression or a change in the patient’s posture that
suggests the existence of second-order thoughts. In such cases, more active
therapeutic assistance may be needed. For example, the therapist may need to act
as a teacher or coach in the area of adaptive cog-nitive functioning, rapidly
rebutting automatic thoughts as they arise. Coping cards, which are index cards
with helpful remind-ers on the use of CBT methods (in this case, rational
responses to repetitive automatic negative thoughts), may be written during
sessions and carried by the patient in his or her pocket, wallet, or purse for
later use.
Cognitive–Behavioral Rehearsal
Cognitive–behavioral
rehearsal is a treatment strategy that is par-ticularly useful for preparing
patients to put their experiences in CBT to work in real-life circumstances.
After automatic thoughts have been elicited and modified through procedures
described before, the therapist guides the patient in a series of rehearsalexercises
to try out alternative cognitions in a variety of situa-tions. By using imagery
and role-playing scenarios to practice generating more adaptive cognitions, the
patient may become aware of problems that could interfere with implementation
of the new style of thinking. Further practice and targeted homework
as-signments may then be needed before alternative cognitions can be fully
used. For example, the effects of cognitive–behavioral rehearsal may be
extended to real situations by assigning home-work to test use of the modified
automatic thoughts.
Modifying Schemas
The
emphasis in the early phases of therapy is usually on behavioral activation,
identifying and changing automatic thoughts, and the reduction of symptoms.
However, as the patient gains knowledge of cognitive–behavioral principles and
acute symptoms begin to subside, the focus of the treatment sessions usually
shifts toward work on the schema level. Because schemas serve as underlying
templates for making sense of new information, they play a major role in the
modulation of more superficial cognitions (automatic thoughts), regulation of
affect, self-esteem and control of the behavioral repertoire. Thus, schema
modification is an important component of cognitively oriented therapies.
With Axis
I disorders such as major depressive disorder and panic disorder, schema
revision efforts are directed at cor-recting dysfunctional attitudes that may
predispose the patientto symptomatic recurrences. After several months of
produc-tive therapy, schema modification may be placed in the context of
reducing future vulnerability. CBT of personality disorders typically requires
that a major portion of therapy be devoted to modifying schemas and related
patterns of behavioral dysfunc-tion (Beck et
al., 1990). When schematic work cannot be fully addressed in time-limited
therapy, the model of ongoing change may be introduced. Thus, the patient may
begin to change her or his “life course” by development of a long-term
self-help plan. Jarrett and colleagues (2001) have proposed continuation and
maintenance phases of CBT treatment of depression, and they argue for focusing
on schema change in these phases of treatment if it is not accomplished in the
acute phase of treatment.
Many of
the techniques used to test and modify auto-matic thoughts are also used to
identify and revise schemas. Psychoeducational interventions are usually
required as a first step. Most patients are not aware of their “guiding
principles”, so the therapist may need to begin by introducing and illustrat-ing
this concept. It is often useful to use synonyms for the term schema (such as
basic assumptions or core beliefs) and to dem-onstrate how schemas are linked
to automatic negative thoughts using material from the patient’s own experience
(Wright and Beck, 1994). Socratic questioning is the core procedure used for
schema modification (Beck et al.,
1979; Overholser, 1993c).
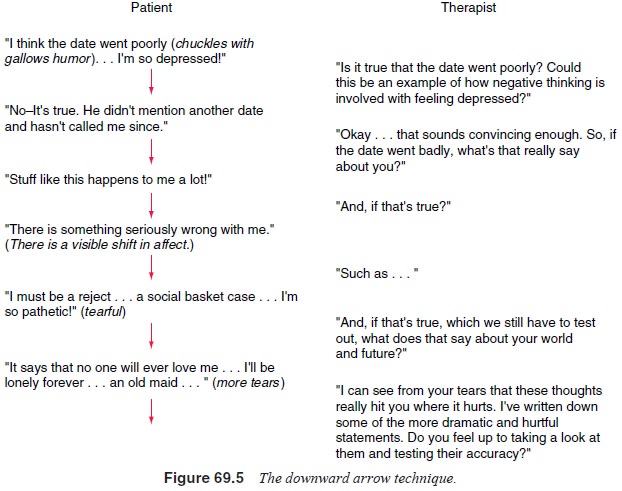
The
downward arrow technique (Figure 69.5) is a particu-larly powerful way to move
from surface cognitions to deeper cognitive structures (Thase and Beck, 1993).
This technique de-scribes asking the patient a question such as: “If this
automatic thought were true, what would it mean about you as a person?” Another
useful approach is to examine patterns of automatic thoughts from thought
records to sort out common themes. The therapist may suggest a thematic
collation based on her or his knowledge of the patient’s automatic negative
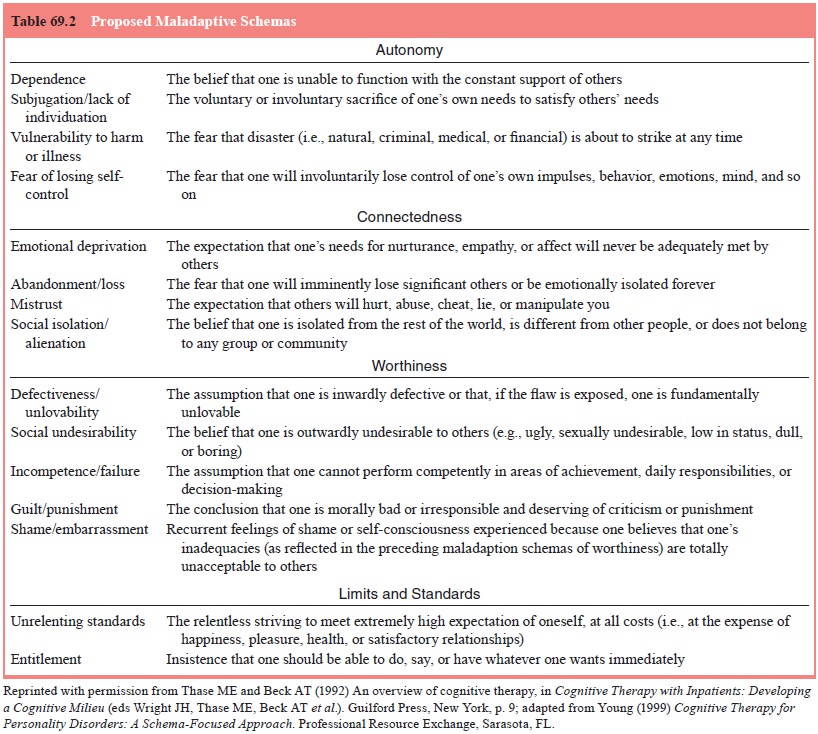
thoughts. In some
situations,
it may be helpful to have patients review a description of common pathological
schemas to recognize some of their core beliefs (see Table 69.2). On occasion,
it may be useful to have the patient write a brief autobiography to help
elucidate the historical antecedents of the schema. Computerized learning programs
can also be employed to help patients uncover their schemas (Wright et al., 1995, 2002a).
Because
schemas are so strongly held (in essence, they have helped define reality and
mold behavior for years), they may require intensive work in a number of therapy
sessions to undergo significant change. Sometimes long-term continuation and
maintenance CBT is required to accomplish schematic re-structuring. Therapists
can select from a number of CBT tech-niques, including examining the evidence,
listing advantages and disadvantages, generating alternatives, cognitive
response prevention and cognitive–behavioral rehearsal, as they attempt to
modify schemas (Wright and Beck, 1994). Examining the evidence, generating
alternatives and cognitive–behavioral re-hearsal were described earlier as
methods of changing automatic thoughts.
Cognitive Response Prevention
In cognitive response prevention, the patient agrees to complete a homework assignment in which she or he must behave in a way that is inconsistent with the pathological schema. For example, a person with perfectionistic attitudes may be engaged in an assign-ment in which she or he must perform in a “so-so” manner. This is intended to activate the schema which is triggering automatic negative thoughts (e.g., “They’ll think I’m a sloth” or “I’ll never be trusted with an important assignment again”). By not respond-ing to the perfectionistic demands dictated by the schema, the individual thus has the opportunity to cope with the automatic negative thoughts consequent to this “rule violation”.
Listing Advantages and Disadvantages
The
listing advantages and disadvantages procedure is particu-larly useful when a
schema appears to have both adaptive and maladaptive features. Schemas that
have damaging effects are often maintained because they also have a positive
side. For ex-ample, the schema “I must be perfect to be accepted” can have
significant benefits (e.g., hard work and attention to detail often lead to
success in work or school). Nevertheless, because perfec-tion is seldom
possible, the individual may remain vulnerable to setbacks. Other schemas, such
as “I’m a complete loser”, may not seem to have any advantages at first glance.
However, even such a markedly negative basic assumption can have certain
behavioral reinforcers associated with it. For example, a person who believes
that he or she is a loser may avoid making commitments, with-draw from
challenging assignments, or refuse to exert a sustained effort to solve a
difficult problem. This strategy may thus protect the person from painful
setbacks. The advantages and disadvan-tages analysis provides the patient and
therapist with essential in-formation for planning modifications. Revised
schemas are most likely to be used when they take into account both the
maladap-tive and the adaptive features of the old basic assumption.
In
general, it is recommended that patients keep a list of the schemas as they
have been identified. The schema list helps to focus the patient’s attention on
the overarching nature of these maladaptive principles. Because schemas often
become manifest only during periods of increased stress or symptom expression,
they may appear to fade in significance as the patient begins to improve. For
example, behavioral treatment programs that nei-ther endorse nor aim to modify
schemas are generally as effective as CBT in the short run. However, there may
be a false security engendered by symptom relief. The cognitive model posits
that the individual will remain vulnerable to the depressogenic im-pact of
“matching” life events unless schema revision is accom-plished (Thase and Beck,
1993).
Related Topics