Chapter: Essentials of Psychiatry: Cognitive and Behavioral Therapies
Behavioral Techniques
Behavioral
Techniques
In CBT,
behavioral methods are usually integrated with cogni-tive restructuring in a
comprehensive treatment plan. Behavioral strategies may be given a greater
emphasis earlier in therapy with more severely symptomatic patients such as
those with intense depression, bipolar symptoms, or schizophrenia (Beck et al., 1979; Thase and Wright, 1991;
Kingdon and Turkingdon, 1995; Basco and Rush, 1996; Scott and Wright, 1997).
Some cogni-tive–behavior therapists may rely primarily on behavioral
inter-ventions for conditions such as obsessive–compulsive disorder (OCD) or
simple phobias. Commonly used behavioral strategies are described here in
alphabetical order.
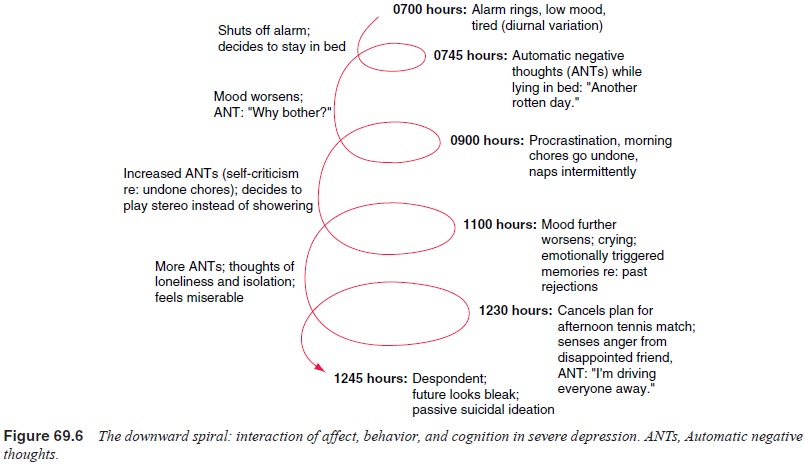
Activity Scheduling, Graded Tasks and Mastery–Pleasure Exercises
One key
to the behavioral approach for treatment of depression is the interruption of
the downward spiral linking mood, inactiv-ity and negative cognition (Beck et al., 1979; Lewinsohn et al., 1982) (Figure 69.6). Completing
an activity schedule is often the first behavioral homework assignment used in
CBT (Beck and Greenberg, 1974). Depressed patients are asked to begin to keep a
daily log that is used to chart the relationship between their moods and their
activities (Figure 69.7).
The
nature of the activities is examined, and deficits in activities that might
elicit pleasure or feelings of competence are identified. Next, assignments are
made to engage in discrete pleasurable activities (or, in the case of an
anhedonic individ-ual, activities that were rewarding before becoming
depressed). If needed, a “menu” of reinforcers can be generated by having the
patient fill out a Pleasant Events Schedule (Lewinsohn et al., 1982). Following operant principles, activities that have
been “high-grade” reinforcers in the past are scheduled during times of low
moods or decreased activity. Next, subjective ratings of
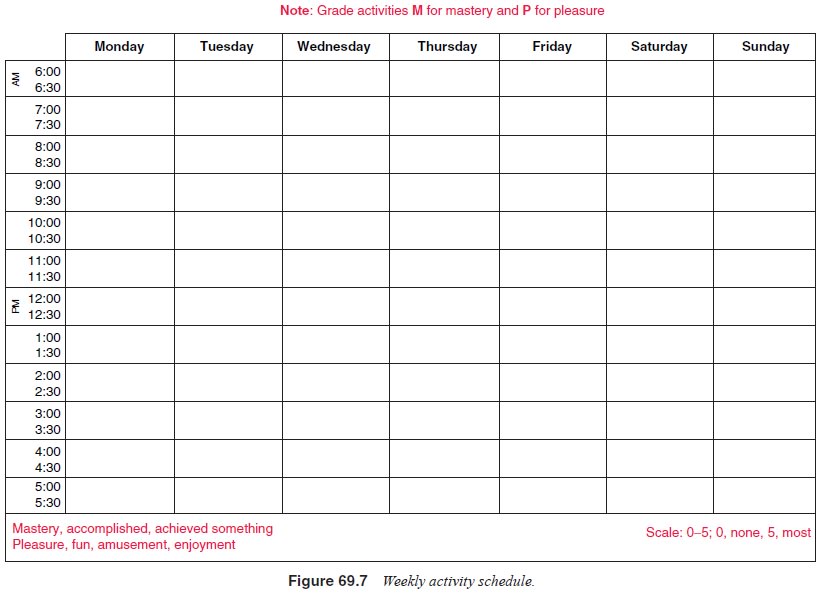
mastery
or competence and pleasure are added to the activity schedule by use of a
simple scale (i.e., 0–5), to avoid the tendency of dichotomous thinking. In
this way, achieving a small degree of pleasure or mastery during a scheduled
activity may be framed as an accomplishment, particularly early in the course
of therapy.
Breathing Control
An
important component of CBT for anxiety disorders involves teaching the patient
breathing exercises that may be used to counteract hyperventilation and/or
reduce tension (Clark et al., 1985).
Slow, deep breathing can have a calming effect not unlike progressive muscle
relaxation (Bernstein and Borkovec, 1973). These exercises also help to distract
the patient from autonomic cues. After initial instruction and practice, the
breathing skills are then applied in progressively more anxiety-provoking
situations.
A note of
caution is in order when teaching patients breath-ing control exercises. We
have seen many patients who have misunderstood instructions and who have
developed a pattern of deep overbreathing in response to stress. Instead of
helping reduce anxiety, their breathing changes may increase the chances of
hyperventilation. Thus, we typically recommend that patients be taught about
the pace and form of normal breathing patterns. Next clinicians can model
normal, calm breathing as compared with overbreathing during an anxiety attack.
The second hand of a watch can be used to time breaths so that they can be
slowed to a normal rate. Positive, calming images can also be used to reduce
anxiety during the breathing exercises. Finally, we suggest that patients
practice breathing exercises regularly to gain mastery of this anxiety
management technique.
Contingency Contracting and Behavior Exchange
These
strategies use the principles of operant conditioning (Skinner, 1938) to modify
the probability of occurrence of either undesired or desired behaviors. An
excellent introduction to these methods is presented by Malott and colleagues
(1993). One key to applied behavioral analysis is control over the
contingencies or reinforcers. Another important factor is that the terms of the
contract are negotiated and should be specific and relatively straightforward.
The positive contingency or reinforcer should be desirable and available
shortly after the terms of the contract have been met. A paycheck is a good
example of a contingency contract. Another common strategy is to chain, or
pair, a high-frequency behavior (e.g., reading, watching television, or
listening to music) to a low-frequency one (e.g., doing paperwork, doing
housework, spending time with the children). Contingencies should generally
start out relatively “rich” (e.g., 1 hour of video game time after 15 minutes
of paperwork) and may be progressively “thinned” in time (Malott et al., 1993). Punishments or “response
cost” contingencies are less widely used because of their negative affective
responses (Azrin and Holz, 1966).
Behavioral
contracts may be particularly useful for assisting patients with medication
adherence. For example, thetherapist may help the patient identify barriers to
taking medica-tion as prescribed and then work out behavioral solutions which
are written in contract form. Behavioral methods may include pairing medication
taking with routine activities such as brush-ing teeth or meals, reminder
systems and reinforcement from sig-nificant others. We recommend explicit
discussion of adherence problems and mutual agreement on a plan for taking
medications when patients have difficulty in following the pharmacotherapy
plan.
Desensitization and Relaxation Training
Systematic
desensitization (Wolpe, 1958) was one of the first behavioral strategies to
gain wide acceptance. Systematic desensitization relies on exposure through a
progressive hierarchy of fear-inducing situations. This procedure may use
pairing of progressive deep muscle relaxation and visualization of the target
behavior to decondition fearful responses. Systematic desensitization is useful
for treatment of simple phobias, social phobia, panic attacks and generalized
anxiety (Wolpe, 1982). Some evidence suggests that the active ingredient of
systematic desensitization is exposure to the feared situation, first in imagination
and later in reality, rather than an actual counterconditioning through the
relaxation response (Kazdin and Wilcoxin, 1976). Progressive deep muscle
relaxation is also useful as a self-directed coping strategy and for treatment
of sleep-onset insomnia (Goldfried and Davison, 1994; Bernstein and Borkovec,
1973).
Exposure and Flooding
The
purpose of these strategies is to speed extinction of conditioned fear or
anxiety responses. Behavioral theory dictates that fearfulness is reinforced by
avoidance and escape behaviors (Rachman et
al., 1986). Because the basis of the fear or phobia is irrational, the
optimal strategy is to increase exposure to the feared activity without
aversive consequences. In obsessive–compulsive disorder, the ritualistic behavior
(e.g., handwashing or checking) is presumed to be reinforced by the relief of
the anxiety associated with the compulsion (e.g., handwashing temporarily
relieves the fear of contamination) (Rachman et al., 1986). In exposure, there are at least three means of fear
reduction: autonomic habituation, recognition that the fear is irrational and
explicit enhancement of morale or self-efficacy that accompanies mastering the
previously dreaded activity.
In graded
or progressive exposure, a hierarchy is estab-lished, ranging from least to
most anxiety-provoking situations. The individual is taught one or more ways to
cope with anxiety (e.g., relaxation or self-instruction), and with the help of
the ther-apist, the items on the hierarchy are worked through, one item at a
time. Mastery is predicated on maintaining a sufficient duration of exposure
for the fear to extinguish or dissipate. In some cases, imagery (exposure in vitro) is used before moving to
exposure to the actual feared stimulus. Exposure may also be enhanced by guided
support (i.e., the therapist’s presence during the session) or by use of coping
cognitions for the duration of the exposure exercise.
Flooding,
which relies on the same principles, dispatches with the hierarchical approach.
The individual is exposed to the maximal level of anxiety as quickly as
possible. The rationale for this accelerated approach is that it may hasten
autonomic habituation. To be effective, flooding needs to be accompanied by
response prevention. In response prevention treatment of OCD, the individual
agrees not to perform the compulsion de-spite strong urges to do so. Because
obsessions are more private than compulsions, there can be less certainty that
the individual has fully participated in response prevention exercises (Stern,
1978).
Simple
phobias may be rapidly treated by an accelerated form of exposure referred to
as participant modeling or contact desensitization. The therapist serves as a
supportive coach or guide and assists the patient through a progressively more
de-manding level of exposure to the feared situation. In most cases, lifelong
fears of air travel, tunnels, heights, matches, dogs, water, or insects can be
fully treated in a few hours of guided exposure.
Social Skills Training
Satisfactory
interpersonal relationships require a complex set of skills, including
reciprocity, respect for another’s opinion, appro-priate modulation of
self-disclosure, the tempered ability to yield on some occasions and to set
limits at other times, the natural use of social reinforcers, and the capacity
to express anger and re-solve conflicts in a constructive manner (Lewinsohn et al., 1982; Hersen et al., 1984). Many people with
psychiatric disorders suf-fer from either a state-dependent deterioration of
these social skills or lifelong deficits of such skills. Once established,
social skills deficits can increase the likelihood of experiencing stress-ful
life events as well as “turn off ” family members and other sources of social
support that may help to buffer people against stressors (Coyne et al., 1987).
Problems
as diverse as underassertiveness, temper “atta-cks”, excessive self-disclosure,
monopolistic conversational style, underreinforcement of significant others and
splitting (i.e., playing one against another) are amenable to social skills
train-ing. The methods employed include modeling (i.e., the therapist
demonstrates a more effective alternative approach), role-playing and role
reversal, behavior rehearsal and specific practice as-signments. Often, the
interpersonal anxiety and lack of self-confidence that go hand in hand with
social skills deficits lessen in response to successful mastery of targeted
assignments.
Thought Stopping and Distraction
Automatic
negative thoughts and repetitive, intrusive rumina-tions are sometimes too
intense to address with purely cogni-tive interventions. The technique of
thought stopping capitalizes on the individual’s ability to use a selectively
narrowed atten-tional focus to suppress the intrusive cognitions. For example,
a ruminative individual may be asked to visualize a large red “stop” sign,
including its octagonal shape and white lettering. The command “Stop!” is
paired with the image. The image and command are then used to interrupt a “run”
of ruminations. At first, the technique is practiced in sessions at times when
auto-matic thoughts or ruminations are mild. After initial success, the
technique is next applied to more intensely disturbing cognitions. For
individuals who find visualization difficult or ineffective, a rubber band may
be worn on the wrist as a distractor. In a manner similar to that described
before, the command “Stop!” is paired with a brisk snap of the rubber band.
Indications for Treatment
The
cognitive and behavioral therapies are indicated as pri-mary treatments for
adults suffering from several nonpsychotic, nonorganic disorders including
major depressive disorder, dysthymic disorder, panic disorder, social phobia,
OCD, post traumatic stress disorder (PTSD), generalized anxiety disorder and
bulimia nervosa (Wright et al.,
2002b). Cognitive and be-havioral therapies are also useful as adjunctive
treatments for patients with bipolar disorder (Basco and Rush, 1996; Basco and
Thase, 1998; Lam et al., 2000) and
schizophrenia (Mueser, 1998; Kingdon and Turkington, 1995; Senky et al., 2000). Although not extensively
studied, cognitive and behavioral therapies in-corporating coping skills
training and relapse prevention strate-gies may also improve the outcome of
individuals with substance abuse disorders (Wright et al., 2002b).
Cognitive
and behavioral therapies, like most other types of treatment, have not been
studied widely in patients with Axis II disorders. However, the CBT approach to
problem specifica-tion and explicit training in coping skills may be well
suited for treatment of individuals willing to work on changing these
ha-bitual, ingrained patterns of thinking and behavior (Beck et al., 1990). Specific
cognitive–behavioral formulations have been de-veloped for each of the
personality disorders, and modifications of CBT methods have been described for
working with patients with Axis II problems (Beck et al., 1990). Linehan’s model of CBT (dialectical behavior
therapy) has been shown to be effica-cious in reducing parasuicidal behavior in
patients with border-line personality disorder (Linehan et al., 1991, 1993).
Related Topics