Chapter: Essentials of Psychiatry: Cognitive and Behavioral Therapies
Cognitive Model
Cognitive
Model
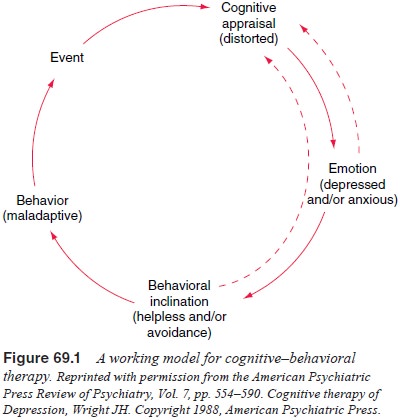
The basic
theories of the cognitive model are rooted in a long tradition of viewing
cognitions as primary determinants of emo-tion and behavior. For excellent
reviews of the historical bases of cognitive therapy, see Dobson and Block
(1988) Clark et al. (1999). The
description of cognitive theories given here is based largely on Beck’s
concepts. This model of therapy tends to give somewhat more emphasis to
cognitive than behavioral factors in treatment interventions, but both are
considered to be integral parts of the model (Figure 69.1).
Depending
on the case formulation and the phase of therapy, attention may be directed
primarily at cognitive or behavioral as-pects of the disorder. In most cases, a
combination of cognitive and behavioral techniques is used.
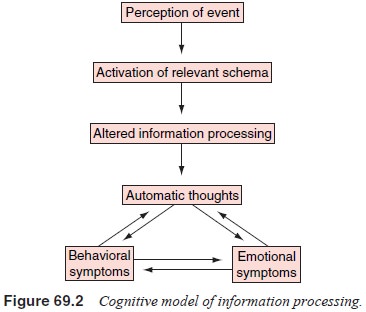
Figure
69.2 displays a simplified model for understanding the relationships between
environmental events, cognitions, emo-tion and behavior (Wright and Beck, 1994;
Wright, 1988; Thase and Beck, 1993). This model is based on the theoretical
assumptionthat environmental stimuli trigger cognitive processes and the
ensuing cognitions give the event personal meaning and elicit subsequent
physiological and affective arousal. These emotions, in turn, have a potent
reciprocal effect on cognitive content and information processing, such that
cascades of dysfunctional thoughts and emotions can occur. The individual’s
behavioral re-sponses to stimuli and thoughts are viewed as both a product and
a cause of maladaptive cognitions. Thus, treatment interventions may be targeted
at any or all components of the model.
Of
course, many other factors are involved in psychiatric disorders, including
genetic predisposition, state-dependent neuro-biological changes and various
interpersonal variables. These influ-ences are also included in the case
conceptualization in CBT. Wright and Thase (1992) have outlined an expanded
cognitive–biological model that can be used for synthesizing cognitive and
neurobiologi-cal factors in a combined therapy approach. Contemporary
psychi-atric research is striving to understand how best to combine and/or
sequence CBT and pharmacotherapy, and relate CBT technique to new
understandings in cognitive neuroscience. Nevertheless, the working model in
Figure 69.2 can be used as a practical template to guide the therapist’s case
formulation and interventions.
Automatic Thoughts and Schemas
Dysfunctional
information processing is apparent in many psychi-atric disorders at two major
levels of cognition–automatic thoughts and schemas (Beck, 1976; Dobson and
Shaw, 1986; Teasdale, 1983; Segal, 1988; Alfrod and Correia, 1994). Automatic
thoughts are cognitions that stream rapidly through an individual’s mind,
whether spontaneously or in response to some prompt or stimu-lus. Automatic
thoughts may be triggered by affective arousal (i.e., anger, anxiety, or
sadness), or conversely, affective shifts are gener-ally accompanied by
automatic negative thoughts (Teasdale, 1983). Their automatic nature refers to
their speed of entry into awareness and their implicit believability. In this
way, automatic thoughts have emotional validity (Thase and Beck, 1993). For
most people, before therapy, automatic thoughts are usually not examined
carefully for validity. In fact, many people susceptible to anxiety or
depression are likely to use an affectively focused logic referred to as
emotional reasoning (i.e., “I feel
that this is correct, therefore it is correct”). Although we all experience
automatic thoughts, in depression, anx-iety and other psychiatric disorders the
thoughts are distinguished by their greater intensity and frequency (LeFebvre,
1981).
Beck (1967) coined the term cognitive triad to describe the content of automatic negative thoughts. Typically, automatic negative thoughts may be grouped by themes pertaining to self, world (i.e., significant others or people in general) and future. As described subsequently, the themes revealed in one’s characteris-tic automatic negative thoughts may be used to infer deeper levels of cognition: beliefs, rules and schemas. Patients can be taught to examine their beliefs and their operational rules. Although pa-tients are not fully aware of their schemas, these cognitions are usually accessible through the questioning techniques used in CBT (Wright and Beck, 1994).
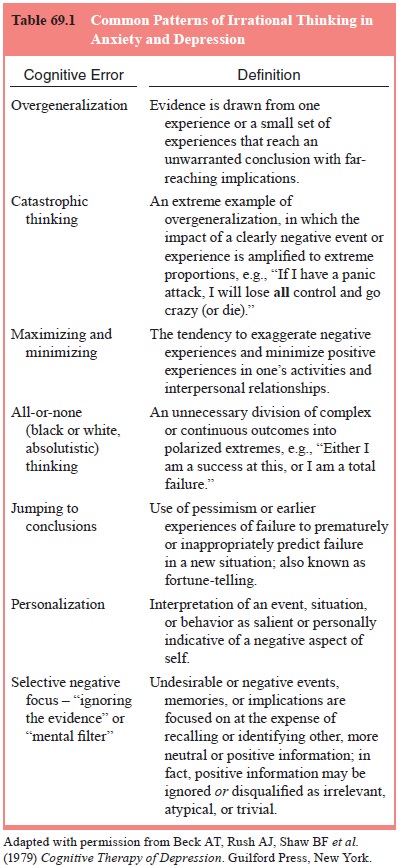
Beck and
coworkers (Beck et al., 1979; Beck
and Emery, 1985; Wright and Beck, 1983) have noted that stereotypic errors in
logic (termed cognitive errors or cognitive distortions) also shape the content
of automatic thoughts (Table 69.1).
Schemas
represent the sum of one’s beliefs and attitudes. They are the basic
assumptions or unspoken rules that act as templates for screening and decoding
information from the environment (Segal, 1988; Wright and Beck, 1983; Young and
Lindermann,
1992). Psychological well-being may be understood in part by development of a
set of schemas that yield realistic appraisals of self in relation to world
(e.g., “I’m reasonably attrac-tive, but looks aren’t everything”, “I can be
loved under the right circumstances”, or “I must work harder to compensate for
an av-erage intellect”). Although unspoken, schemas may be inferred from one’s
beliefs and attitudes. In the cognitive model, dysfunc-tional attitudes are the
structural “bridge” between pathological schemas and automatic negative
thoughts. Schemas pertaining to safety, vulnerability to threat,
self-evaluation, one’s lovability, and one’s competence or self-efficacy
contain the ground rules for personal behavior that are particularly relevant
to the understand-ing of disorders such as anxiety, depression, or
characterological
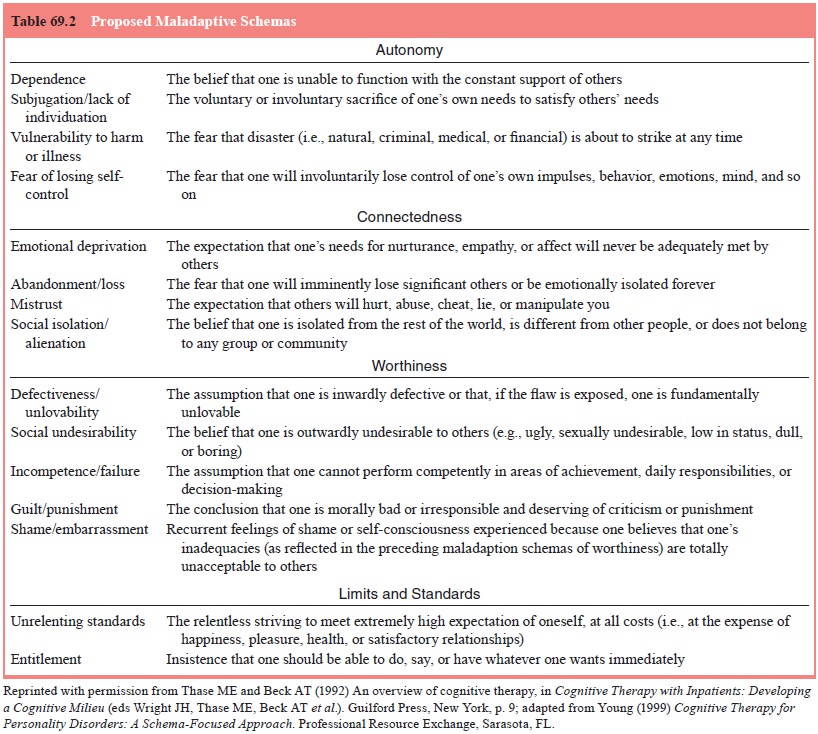
disturbances
(Segal, 1988; Young and Lindermann, 1992; Blackburn et al., 1986b; Beck et al.,
1990). A number of schemas relevant to psychiatric illness are listed in Table
69.2. Bowlby (1985) has noted that most psychopathologically relevant sche-mas
are developed early in life, when the individual is relatively powerless and
dependent on caregivers.
The
cognitive model of psychiatric illness emphasizes the concept of stress-diathesis
(Thase and Beck, 1993; Metalsky et al.,
1987). From this perspective, a schema such as “I must be loved to have worth”, might remain latent until activated by a
relevant life stressor (i.e., a romantic breakup).
Underlying
schemas may be buttressed by either mala-daptive or adaptive attitudes (e.g.,
“No matter how hard I try, I’m bound to fail” versus “I’m a survivor; if I just
hang in there things will be okay”), but many of these cognitive structures
have mixed features (Wright and Beck, 1994). Schemas such as “If I’m not
perfect, I’m a failure” may lead to driven obsessional behav-ior, rigid
attitudes and beliefs, and frequent bouts of dysphoric or irritable moods.
However, basic perfectionistic beliefs such as these can also result in high
levels of performance and success.
The
concept of attributional style (Hammen et
al., 1989) describes an alternative view of cognitive vulnerability.
Derived from human studies of the learned helplessness para-digm (Seligman,
1975), attributional style refers to the charac-teristic way that people
explain the causality, controllability and impact of events. People susceptible
to depression are more likely to have an attributional style in which negative
events are per-ceived to be personally controllable (i.e., internality),
far-reaching (i.e., globality), and enduring (i.e., stability) (Peterson et al., 1985; Abramson et al., 1989; Sweeney et al., 1986).
The
results of many studies suggest that disturbances in information processing are
essential features of depression and anxiety.
Related Topics