Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Postanesthesia Care
Circulatory Complications
CIRCULATORY
COMPLICATIONS
The most
common circulatory disturbances in the PACU are hypotension, hypertension, and
arrhyth-mias. The possibility that the circulatory abnor-mality is secondary to
an underlying respiratory disturbance should always be considered before any
other intervention, especially in children.
Hypotension
Hypotension is usually due to
relative hypovolemia, left ventricular dysfunction, or, less commonly, excessive
arterial vasodilatation. Hypovole-mia is by far the most common cause of
hypotension in the PACU. Absolute hypovolemia can result from inadequate
intraoperative fluid replace-ment, continuing f ulid sequestration by tissues
(“third-spacing”), wound drainage, or hemorrhage. Vasoconstriction during
hypothermia with central sequestration of intravascular volume may mask
hypovolemia until the patient’s temperature begins to rise again; subsequent
peripheral vasodilation during rewarming unmasks the hypovolemia and results in
delayed hypotension. Relative hypovole-mia is often responsible for the
hypotension associ-ated with spinal or epidural anesthesia (especially in the
setting of concomitant general anesthesia), venodilators, and α-adrenergic blockade: the venous
pooling reduces the effective circulating
blood volume, despite an otherwise normal
intra-vascular volume . Hypotension associated with sepsis and allergic
reactions is usu-ally the result of both hypovolemia and vasodila-tion.
Hypotension from a tension pneumothorax or cardiac tamponade is the result of
impaired venous return to the right atrium.Left ventricular dysfunction in
previously healthy persons is unusual, unless it is associated with severe
metabolic disturbances (hypoxemia, acidosis, or sepsis). Hypotension due to
ventricu-lar dysfunction is primarily encountered in patients with underlying
coronary artery or valvular heart disease or congestive heart failure and is
usually precipitated by fluid overload, myocardial ischemia, acute increases in
afterload, or arrhythmias.
Treatment of Hypotension
Mild hypotension during recovery from
anesthesia is common and typically does not require intensive treatment.
Significant hypotension is often defined as a 20% to 30% reduction in blood
pressure below the patient’s baseline level and usually requires cor-rection.
Treatment depends on the ability to assess intravascular volume. An increase in
blood pres-sure following a f luid bolus (250–500 mL crystal-loid or 100–250 mL
colloid) generally confirms hypovolemia. With severe hypotension, a
vasopres-sor or inotrope (dopamine or epinephrine) may be necessary to increase
arterial blood pressure until the intravascular volume deficit is at least
partially corrected. Signs of cardiac dysfunction should be sought in patients
with heart disease or cardiac risk factors. Failure of a patient with severe
hypotension to promptly respond to initial treatment mandates invasive
hemodynamic monitoring, or, better still, echocardiographic examination;
manipulations of cardiac preload, contractility, and afterload are often
necessary. The presence of a tension pneumo-thorax, as suggested by hypotension
with unilater-ally decreased breath sounds, hyperresonance, and tracheal
deviation, is an indication for immediate pleural aspiration, even before
radiographic confir-mation. Similarly, hypotension due to cardiac tam-ponade,
usually following chest trauma or thoracic surgery, often necessitates
immediate pericardiocen-tesis or surgical exploration.
Hypertension
Postoperative hypertension is common in the
PACU and typically occurs within the first 30 min after admission. Noxious
stimulation from inci-sional pain, endotracheal intubation, or bladder
distention is usually responsible. Postoperative hypertension may also reflect
the neuroendocrine stress response to surgery or increased sympathetic tone
secondary to hypoxemia, hypercapnia, or met-abolic acidosis. Patients with a
history of hyperten-sion are likely to develop hypertension in the PACU, even
in the absence of an identifiable cause. Fluid overload or intracranial
hypertension may also occasionally present as postoperative hypertension.
Treatment of Hypertension
Mild hypertension generally does not require
treat-ment, but a reversible cause should be sought. Marked hypertension can
precipitate postopera-tive bleeding, myocardial ischemia, heart failure, or
intracranial hemorrhage. Although decisions to treat postoperative hypertension
should be indi-vidualized, in general, elevations in blood pressure greater than
20% to 30% of the patient’s baseline, or those associated with adverse effects
such as myo-cardial ischemia, heart failure, or bleeding, should be treated.
Mild to moderate elevations can be treated with an intravenous β-adrenergic blocker, such as labetalol,
esmolol, or metoprolol; an angiotensin-converting enzyme inhibitor, such as
enalapril; or a calcium channel blocker, such as nicardip-ine. Hydralazine and
sublingual nifedipine (when administered to patients not receiving β-blockers) may cause tachycardia and
myocardial ischemia and infarction. Marked hypertension in patients with
limited cardiac reserve requires direct intraarterial pressure monitoring and
should be treated with an intravenous infusion of nitroprusside, nitroglycerin,
nicardipine, clevidipine, or fenoldopam. The end point for treatment should be
consistent with the patient’s own normal blood pressure.
Arrhythmias
Respiratory disturbances, particularly
hypoxemia, hypercarbia, and acidosis, will commonly be associ-ated with cardiac
arrhythmias. Residual effects from anesthetic agents, increased sympathetic
nervous system activity, other metabolic abnormalities, and preexisting cardiac
or pulmonary disease also pre-dispose patients to arrhythmias in the PACU.
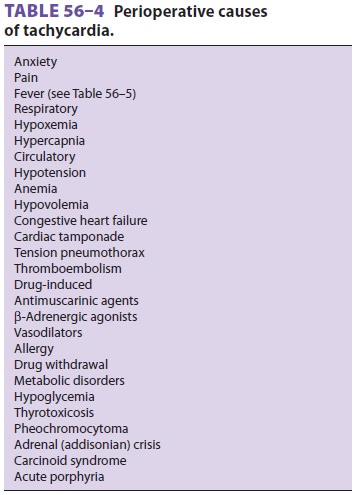
Bradycardia often represents the residual
effects of cholinesterase inhibitors, opioids, or β-adrenergic blockers. Tachycardia may represent the effect of an
anticholinergic agent; a β-agonist, such as albuterol; reflex tachycardia from hydralazine; and
more com-mon causes, such as pain, fever, hypovolemia, and anemia.
Anesthetic-induced depression of barore-ceptor function makes heart rate an
unreliable mon-itor of intravascular volume in the PACU.
Premature atrial and ventricular beats often
represent hypokalemia, hypomagnesemia, increased sympathetic tone, or, less
commonly, myocardial ischemia. The latter can be diagnosed with a 12-lead ECG.
Premature atrial or ventricular beats noted in the PACU without discernable
cause will often also be found on the patient’s preoperative ECG, if one is
available. Such patients with a preexisting history of extrasystoles may or may
not have a history of palpitations or other symptoms, and previous car-diology
evaluation often has found no definitive cause. Supraventricular
tachyarrhythmias, including paroxysmal supraventricular tachycardia, atrial
flut-ter, and atrial fibrillation, are typically encountered in patients with a
history of these arrhythmias and are more commonly encountered following
thoracic surgery.
Related Topics