Chapter: Surgical Pathology Dissection : Breast
Breast Mastectomy : Surgical Pathology Dissection
Mastectomy
True radical mastectomies are seldom performed anymore. The procedure includes complete axillary dissection including removal of the modified radical mastectomy is more common.
With this procedure the undersurface of the
spec-imen is composed only of fascial planes with occasional shreds of
pectoralis major muscles attached. The anterior surface usually contains an
island of skin and nipple with the subcutaneous tissue extending beyond it.
Nevertheless, com-plete axillary dissection typically is included within the
specimen, forming an elongated tail at one end of the otherwise elliptical
specimen. Most mastectomies are performed after a core needle biopsy has
established a diagnosis of in-vasive carcinoma or after a lumpectomy has not
been successful in completely removing an in
situ and/or invasive carcinoma.
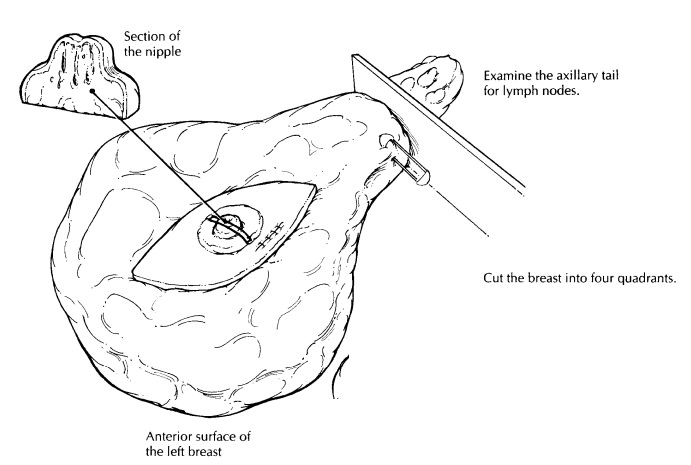
First,
orient the specimen to localize the four quadrants of the breast correctly.
This step should not be difficult if you use the axillary contents, the
sidedness of the breast, and the surgeon’s description of the location of the
tumor. Once the specimen has been oriented, place a safety pin in the corner of
the upper outer quadrant. This practice helps you to reorient the specimen
quickly in case you have to return to the speci-men. Weigh and measure the
specimen; then de-scribe the skin, nipple, and any biopsy sites seen. The
axillary tail can be removed now for later examination. Next, take the time to
palpate the specimen. Localize the biopsy scar, the biopsy cavity, and any
masses. Examine the deep surface of the specimen for attached fragments of
skeletal muscle, and ink it so perpendicular sections can be obtained to
evaluate the deep soft tissue margin. Also ink the exposed breast tissue
lateral to the skin ellipse on the anterior surface of the specimen (preferably
with ink of a different color). These constitute the anterior margins. Hence,
all surfaces except for the skin and axillary tail should be inked.
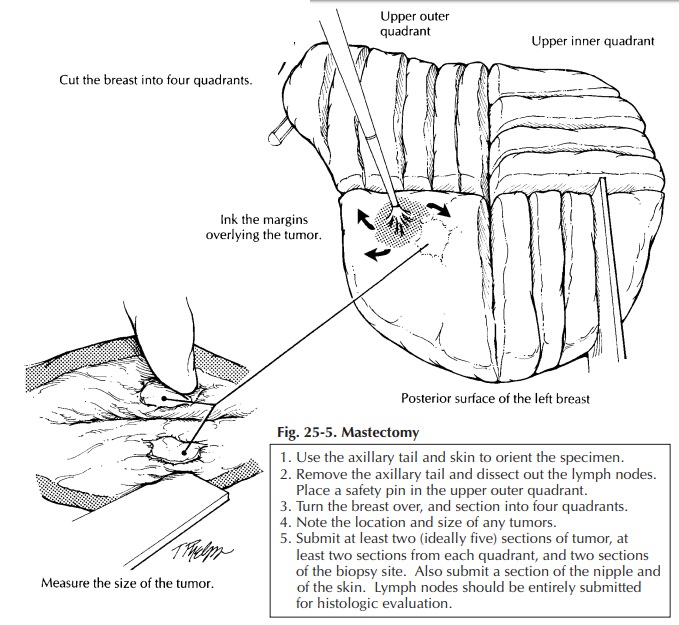
The
breast can then be placed skin surface down on a cutting board and sectioned.
As illus-trated (Figure 25-5), use the nipple to center the specimen; then with
two long perpendicular cuts section the breast into four quadrants. Each
quad-rant can be further sectioned, each in its own direction. These cuts
should not go all the way through the specimen but, instead, should leave the
pieces attached together by a rim of unsec-tioned breast or skin. This
procedure not only helps orient the specimen in a clinically relevant way, it
helps remind you to document in which quadrant(s) the lesion lies The gross dictation
should include
(1) the
over-all dimensions and the weight of the specimen;
![]() the
overall dimensions of the skin surface;
the
overall dimensions of the skin surface;
(2)
the presence or absence of a biopsy scar and
biopsy cavity and their relation to the nipple;
(3)
the presence of any retraction or ulceration of
the nipple and/or surrounding skin; (5) the pres-ence or absence of muscle on
the undersurface of the specimen; (6) the
size and gross appearance ofthe tumor including the quadrant of the breast in
which it is localized; and (7) the distance of thetumor to the deep and
anterior margins. At least two and ideally five sections of the primary lesion
should be submitted for histologic examination. Two sections can then be
submitted from each of the remaining breast quadrants. If the mastec-tomy was performed
as a prophylactic procedure in a patient with an in situ carcinoma, submit at least three sections from each
quadrant; also submit any suspicious lesions in their entirety. Submit a
section of the nipple and one of the skin in the area of the prior biopsy site.
Finally,
dissect all lymph nodes from the axillary contents. If lymph nodes are
separated into levels I, II, and III by their relationship to the pectoralis
minor muscle (lateral, below, and medial to it, respectively), maintain this
orienta-tion. When dealing with axillary lymph nodes in patients with carcinoma
of the breast, it is particularly important to identify and evaluate each lymph
node and to submit lymph nodes that are grossly negative for tumor in their
entirety. Grossly positive nodes do not need to be submitted in their entirety.
The size of the tumor in the grossly involved lymph node should be documented
in your gross report.
Related Topics