Chapter: Human Neuroanatomy(Fundamental and Clinical): Autonomic Nervous System
Autonomic Nerve Supply of some Important Organs
Autonomic Nerve Supply of some Important Organs
The Eyeball
The sphincter pupillae is supplied by parasympathetic nerves. The preganglionic neurons concerned are located in the Edinger Westphal nucleus. Their axons travel through the oculomotor nerve and terminate in the ciliary ganglion. Postganglionic neurons are located in this ganglion. Their axons supply the sphincter pupillae and the ciliaris muscle (Fig. 19.9).
The dilator pupillae is supplied by sympathetic nerves. The preganglionic neurons concerned are located in the intermediolateral grey column of the first thoracic segment of the spinal cord. Their axons emerge through the anterior nerve root of the first thoracic nerve to reach the stellate ganglion. They, however, pass through this ganglion without relay, and ascend in the sympathetic trunk to reach the superior cervical sympathetic ganglion. Postganglionic neurons are located in this ganglion. Their axons pass through the internal carotid nerve. In the cavernous sinus they pass (through communicating twigs) to the ophthalmic division of the trigeminal nerve. They travel through the nasociliary nerve and its long ciliary branches to the dilator pupillae.
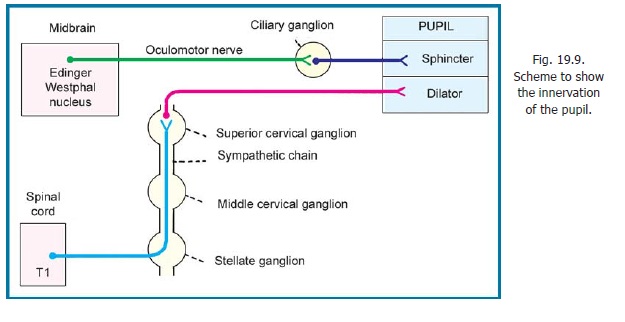
Some sympathetic fibres reach the eyeball after passing through the ciliary ganglion. These fibres do not relay in this ganglion, but merely pass through it. They supply the blood vessels of the eyeball. Occasionally the fibres for the dilator pupillae may follow this route. Apart from the dilator pupillae and blood vessels, sympathetic fibres also supply the orbitalis muscle, smooth muscle in the eyelids, and probably also the ciliaris.
Clinical:
Horner’s syndrome
Interruption of sympathetic supply to the head and neck results in Horner’s syndrome. This consists of the following:
(a) Constriction of the pupil.
(b) Drooping of the upper eyelids (ptosis).
(c) Reduced prominence of the eyeball (enophthalmos).
(d) Absence of sweating on the face and neck.
(e) Flushing of the face.
Salivary Glands
Submandibular and Sublingual glands
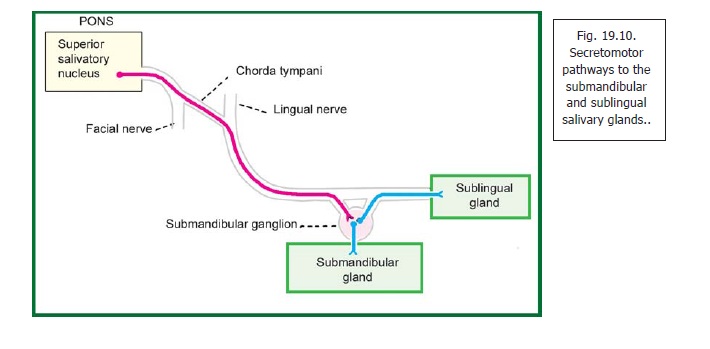
The secretomotor supply to the salivary glands is parasympathetic. Preganglionic neurons for the submandibular gland and for the sublingual gland are located in the superior salivary nucleus (Fig. 19.10). Their axons pass through the facial nerve, its chorda tympani branch and then through the lingual nerve to reach the submandibular ganglion. The postganglionic neurons are located in this ganglion. Their axons reach the submandibular gland through branches from the ganglion to the gland. Some postganglionic neurons may be located in the hilum of the submandibular gland.
Fibres meant for the sublingual gland reenter the lingual nerve and pass through its distal part to reach the gland.
Parotid gland
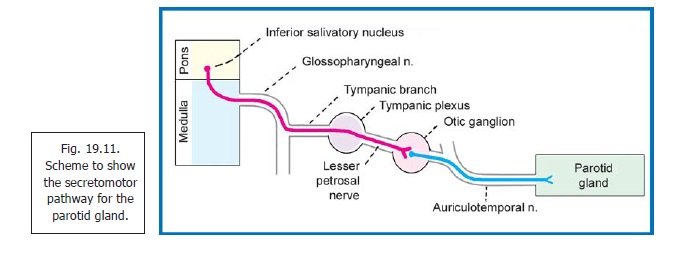
The preganglionic neurons for the parotid gland are located in the inferior salivary nucleus. Their axons pass through the glossopharyngeal nerve and its tympanic branch, the tympanic plexus and the lesser petrosal nerve to terminate in the otic ganglion (Fig. 19.11). Postganglionic fibres arising in this ganglion reach the gland through the auriculotemporal nerve. (It has been reported that some parasympathetic fibres may reach the parotid gland through the facial nerve).
Sympathetic fibres travel to salivary glands along the blood vessels.
Lacrimal Gland
Preganglionic neurons for the lacrimal gland are located near the salivary nuclei. Their axons pass through the facial nerve, its greater petrosal branch, and through the nerve of the pterygoid canal to reach the pterygopalatine ganglion. Postganglionic fibres arising in this ganglion pass successively through the maxillary nerve, its zygomatic branch, the zygomaticotemporal nerve, a communicating branch from the zygomaticotemporal nerve to the lacrimal branch of the ophthalmic nerve, and finally through the lacrimal branch itself to reach the gland. However, some workers are of the opinion that postganglionic fibres reach the lacrimal gland through direct lacrimal rami from the pterygopalatine ganglion.
Gastrointestinal Tract
1. The parasympathetic nerve supply of the greater part of the gastrointestinal tract (from the pharynx to the junction of the right two thirds of the transverse colon with the left one third) is through the vagus. The preganglionic neurons are situated in the dorsal nucleus of the vagus (Fig. 19.6A). (Some of them may lie in or near the nucleus ambiguus).
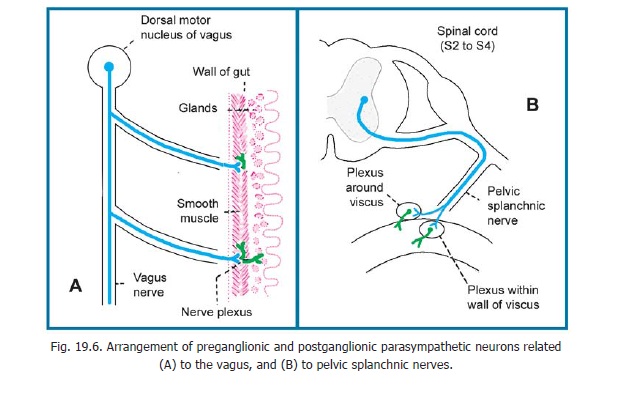
2. The left one third of the transverse colon, the descending colon, the sigmoid colon, the rectum and the upper part of the anal canal are supplied by the sacral part of the parasympathetic system. The preganglionic neurons concerned are located in the second, third and fourth sacral segments of the spinal cord (Fig. 19.6B). They emerge through the ventral nerve roots of the corresponding nerves, and pass into their pelvic splanchnic branches. The fibres to the rectum and the upper part of the anal canal pass through the inferior hypogastric plexus. The remaining fibres pass through the superior hypogastric plexus and are distributed along the inferior mesenteric artery.
3. The postganglionic parasympathetic neurons are located in the myenteric and submucosal plexus in the region to be supplied.
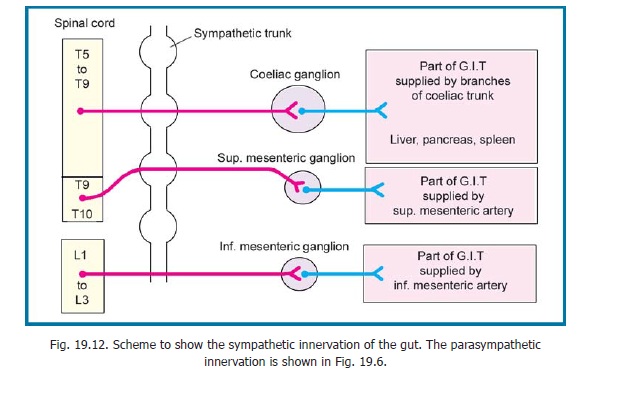
4. Preganglionic sympathetic neurons for the gut are located in the thoracolumbar region of the spinal cord (Fig. 19.12). Their axons pass through the sympathetic trunks without relay. They travel through the splanchnic nerves to terminate in plexuses (and ganglia) related to the coeliac artery, the superior mesenteric artery, the inferior mesenteric artery and the aorta itself. Postganglionic neurons are located in these plexuses. They travel along these blood vessels to reach the gut.
As a rule, parasympathetic nerves stimulate intestinal movement and inhibit the sphincters. They are secretomotor to the mucosal glands. Sympathetic fibres are distributed chiefly to blood vessels.
Afferent fibres travel both along sympathetic and parasympathetic pathways. Pain from most of the gastrointestinal tract travels along sympathetic nerves. However, pain from the pharynx and oesophagus is carried by the vagus, and that from the rectum and lower part of the pelvic colon by pelvic splanchnic nerves.
Urinary Bladder
The parasympathetic nerves to the urinary bladder are derived from the sacral outflow. The preganglionic fibres pass through the pelvic splanchnic nerves and the inferior hypogastric plexuses to reach the vesical plexus. Parasympathetic postganglionic neurons are located in the vesical plexus. Parasympathetic stimulation is motor to the detrusor muscle and inhibitory to the sphincter.
Sympathetic preganglionic neurons are located in spinal segments T10 to L2. Their axons terminate in the inferior mesenteric, superior hypogastric, inferior hypogastric and vesical plexuses. Postganglionic neurons are located in these plexuses. According to classical teaching sympathetic stimulation has an effect opposite to that of the parasympathetic. However, some investigators believe that normal bladder function is controlled only by the parasympathetic nerves, and that sympathetic nerves are purely vasomotor in function.
Clinical:
Sensory fibres carry impulses of distension and of pain from the urinary bladder. They run through both sympathetic and parasympathetic pathways. In the spinal cord, fibres carrying the two types of sensation follow different routes. Fibres carrying pain are located in the anterior and lateral white columns while fibres carrying the sensation of bladder filling travel through the posterior column. As a result, intractable bladder pain (such as may occur because of carcinoma) can be relieved by cutting the anterior and lateral white columns of both sides (bilateral anterolateral cordotomy) without abolishing the sensation of bladder filling.
Severe lesions of the spinal cord above the sacral segments interfere with both afferent and efferent pathways. Normal micturition becomes impossible. However, the bladder empties reflexly when it is full (automatic bladder).
Ureter
Autonomic nerves to the ureter are predominantly sensory in function. They are derived mainly from segments T10 to L2 of the cord and also from segments S2 to S4. Distension by a stone causes severe pain (called renal colic). This is referred to regions of skin innervated by segments T10 to L2. It, therefore, commences in the back over the lower ribs, and shoots downwards and forwards to the inguinal region, scrotum, and sometimes into the front of the thigh.
Heart
Parasympathetic preganglionic neurons for the heart are located in the dorsal nucleus of the vagus. They reach the heart through cardiac branches of the vagus. The postganglionic neurons are located within the superficial and deep cardiac plexuses, and also in the walls of the atria. Their axons are distributed to the atria, the AV bundle, the SA node and the AV node.
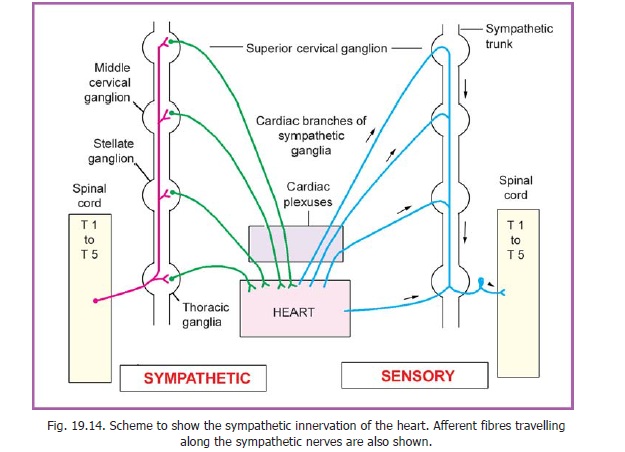
Preganglionic sympathetic neurons are located in segments T1 to T5 of the spinal cord (Fig. 19.14). On reaching the sympathetic trunks their axons synapse with postganglionic neurons in the upper thoracic ganglia. Some fibres run upwards in the sympathetic trunk to end in cervical sympathetic ganglia. Postganglionic fibres leave these ganglia through their cardiac branches, and join the vagal fibres in forming the cardiac plexuses.
Contraction of cardiac muscle is not dependent on nerve supply. It can occur spontaneously. The nerves supplying the heart, however, influence heart rate.
Sympathetic stimulation increases heart rate and parasympathetic stimulation reduces it.
Sympathetic nerves supplying the coronary arteries cause vasodilatation increasing blood flowthrough them.
Clinical:
Afferent fibres from the heart travel through both sympathetic and parasympathetic pathways. Impulses of pain arising in the heart are carried mainly by the cardiac branches of the middle and inferior cervical sympathetic ganglia. Some fibres also pass through cardiac branches of thoracic sympathetic ganglia. These fibres pass through the sympathetic trunks and enter the spinal cord through spinal nerves T1 to T5. The cell bodies of the neurons concerned are located in the dorsal nerve root ganglia on these nerves. These pathways are important as they convey impulses of pain produced as a result of anoxia of heart muscle (angina). The pain is predominantly retrosternal, but it may be referred in various directions including the left shoulder and the inner side of the left arm. (Note that the inner side of the arm is supplied by segment T1). Afferent fibres running along the vagus are concerned with reflexes controlling the activity of the heart.
Bronchi
Parasympathetic preganglionic neurons, that supply the bronchi, are located in the dorsal vagal nucleus. The fibres travel through the vagus and its branches, to reach the anterior and posterior pulmonary plexuses. Postganglionic neurons are located near the roots of the lungs. Their axons run along the bronchi and supply them.
Preganglionic sympathetic neurons are located in the second to fifth thoracic segments of the spinal cord. Their axons terminate in the corresponding sympathetic ganglia. Postganglionic fibres arising in these ganglia reach the bronchi through branches from the sympathetic trunks to the pulmonary plexuses.
Parasympathetic stimulation causes bronchoconstriction, while sympathetic stimulation causes bronchodilatation. Parasympathetic stimulation also produces vasodilatation and has a secretomotor effect on glands in the bronchi. Sympathetic stimulation causes vasoconstriction.
Raynaud’s disease (or phenomenon)
In all persons, exposure to cold can cause vasoconstriction. In some persons this response is abnormally high and vasoconstriction of arterioles in the distal part of the limb may seriously impair blood supply to the hands. In such cases a series of events may be observed. When the hand is cooled first there is a loss of colour (blanching) and the hand becomes pale. After an interval the arterioles dilate and blood starts flowing into the hand, but this blood is deoxygenated (because of stagnation in arteries). The hand becomes swollen and dark. As more blood flows into the hand the deoxygenated blood is washed off (with oxygenated blood) and the hand becomes red in colour.
Basically the condition is caused by abnormally active sympathetic nerves. It can be controlled with drugs. In more severe cases sympathetic denervation of blood vessels of the limb is necessary. This can be achieved by surgical removal of the upper thoracic sympathetic ganglia (preganglionic cervico-dorsal sympathectomy).
Thromboangitis obliterans (Buerger’s disease)
In this condition arteries of the leg and foot are narrowed, and there is thrombophlebitis of veins. The condition is seen only in male smokers. Localized inflammatory changes are present in the walls of arteries and veins. Symptoms of arterial insufficiency are present. Gangrene of toes can occur. The condition can sometimes be controlled by complete abstinence from smoking, and may benefit from lumbar sympathectomy.
Related Topics