Chapter: Essentials of Psychiatry: Therapeutic Management of the Suicidal Patient
Assessment of Suicidal Patients
Assessment
of Suicidal Patients
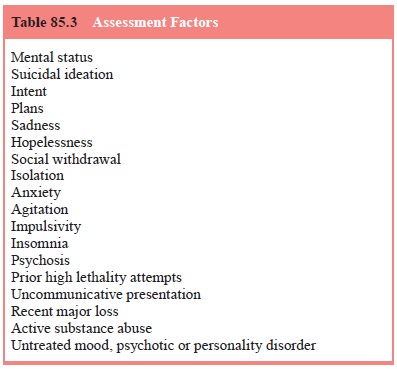
Common
presentations include acute, chronic, contingent, and/or potentially
manipulative suicidal patient. All are associated with anxiety for the care
provider doing the assessment. Careful as-sessment, use of collateral
information and acceptance of predic-tive limitations can be helpful (see Table
85.3).
As
reviewed by Nicholas and Golden (2001), factors to be considered in the
assessment of the acutely suicidal patient include the current mental status,
with special attention to direct inquiry about suicidal ideation, intent (may
be ascertained from family and friends, for example, saying good-byes or
putting af-fairs in order), and plans (well thought out with available means).
Sadness, hopelessness, social withdrawal/isolation, anxiety, agitation,
impulsivity, insomnia, psychosis (especially command hallucinations or
distressing persecutory delusions) are addi-tional concerning symptoms. These
factors, coupled with prior high lethality attempts, uncommunicative
presentation, recent major loss, active substance abuse, or untreated mood,
psychotic, or personality disorder, might indicate that hospitalization is
warranted to ensure safety prior to treating the underlying psy-chiatric
disorder (Nicholas and Golden, 2001).
Sachs and
colleagues (2001) reviewed suicide prevention strategies for bipolar
outpatients, but they can easily be adapted to any potentially suicidal
patient. The reader is reminded that “care providers can, however, be fooled by
the deceptions of a
clever
patient intent on carrying out a lethal act”. Individual-ized treatment plans
should be developed after eliciting current symptoms, including suicidal
ideation; review of risk factors, stressors, comorbid states like substance
use; and past history of suicide attempts. Acute efforts are directed toward
safety and treating the underlying disorder, with follow-up monitoring.
Ad-junctive medications like antipsychotics and anxiolytics can be beneficial.
Clinicians must monitor the amounts of medications prescribed and continue to
be vigilant during early recovery. Harm reduction strategies can include
minimizing access to le-thal means, decreasing social isolation, close
follow-up and in-forming of emergency contact procedures. Hospitalization may
be warranted if suicide is considered as a solution for problems, for active
suicidal ideation, or if there has been a recent attempt. With the caveat that
while admission may provide safety, current knowledge of risk factors do not
wholly inform when to admit or discharge, overreliance on hospitalization may
deter honest reporting, and many acutely depressed patients can be managed as
outpatients with sufficient safeguards. Involuntary admission, while not
therapy in and of itself, may be lifesaving. ECT remains a safe, typically
quick onset, effective option for those at high risk of suicide (Sachs et al., 2001).
There is
no evidence that denial of suicidal intent predicts nonsuicide. Review of
standard risk factors, additional risk factors (e.g. acute relationship and
employment changes), acute versus chronic suicidal ideation, and treatment of
readily reversible factors should be undertaken. High risk diagnoses include
major depression, bipolar disorder, schizophrenia, alcoholism and substance
abuse, and borderline personality disorder. Comorbid alcoholism increases the
risk in every diagnostic category. A history of past attempts, hopelessness,
previous hospitalizations and recent discharge, while not individually
predictive, do heighten concern. Acute risk factors include severe anxiety,
panic attacks, global insomnia and agitation. These symptoms should be
carefully assessed, with aggressive intervention. Benzodiazepines and
antipsychotics can be employed to address anxiety and agitation. Caution must
be taken with benzodiazepines to avoid disinhibition and combination with
alcohol. Mixed states may require mood stabilizers. Serial assessments should
be performed with acute changes as well as chronic suicidal states.
Chronically
suicidal patients also require aggressive treatment of anxiety and agitation.
DBT and cognitive behavioral therapy (CBT) can be helpful in addressing
parasuicidal and suicidal behavior.
A significant
number of psychiatrists utilize the no-suicide contract, or the contract for
safety. Over half of a sample of psy-chiatrists acknowledged using them in
recent survey, and 41% of them had patients make suicide attempts after
entering into one (Kroll, 2000). Sixty-four percent of 14 psychiatric hospital
inpa-tient suicides denied suicidal ideation and half had some form of
no-suicide agreement in place in the week before their deaths (Busch et al., 1993). These have not been
systematically stud-ied as to whether they have any protective effect (Gray and
Otto, 2001). Resnick (2002) cautions that psychiatrists tend to view the
patient as a collaborator in treatment. However, the psychia-trist can be less
viewed as an “ally” and become an “adversary” when the patient has determined
to die by suicide. He notes that failure to recognize this shift in the
doctor–patient relationship can have devastating results. Objective evidence,
as opposed to patient subjective reports, may be telling. Alliances with family
and other caregivers should be maintained, as they can become crucial sources
of information. Resnick believes that no-suicide contracts have little
credence, especially in an adversarial rela-tionship, cause a false sense of
security for the therapist, and have no research literature to suggest efficacy
(Resnick, 2002).
Gutheil
and Schetky (1998) wrote of a most difficult as-sessment: the patient who
expresses suicidal ideation in terms of a future eventuality. The “if [event or
outcome does or does not happen], I will kill myself” contingency poses different
chal-lenges from acute suicidality, manipulative suicidal threats and chronic
suicidality. Suicidality typically engenders anxiety in the therapist.
Contingency suicidality frequently lacks verbal-ized imminence, may make
involuntary commitment difficult, and invites countertransferences which can
lead to exaggerated or inappropriately muted responses. For some patients, the
con-tingency is a defense against suicide. For others, it represents the
ultimate control. Gutheil and Schetky (1998) make several im-portant points: 1)
Some patients almost have an object relation-ship with death, with death
personified as a benevolent bringer of relief. The therapist should approach
that tie with caution, as it may be the only one in which the patient has any confidence;
2) Future deadlines should not be accepted literally; 3) Even when the
contingency is met positively, the suicidal ideation may not re-solve; 4) Some
patients view themselves as already dead, cannot conceive of life without
depression, and challenge the therapist to resurrect them. This stance
undermines any potential relation-ship; and 5) It is of benefit to negotiate a
halt to suicidal acts until depression can be separated from decision-making.
Gutheil and Schetky assert “… psychiatrists should never support suicide, but
should acknowledge the human impossibility of preventing it”. The authors note
that in these circumstances, the patient is at least communicating their
suicidal ideation. The rationale can be explored and an effort made to maintain
the therapeutic relation-ship. Helplessness should be discussed, as suicidal
ideation can be a defense against lack of control or an expression of pain. The
countertransference of the therapist should be considered, as it can cloud
clinical judgment. Consultation with colleagues can be very helpful. The
competency of the patient may be called into question, and has been used as a
defense in suicide malprac-tice cases. The clinician can frequently be
justified in involun-tary commitment as critical dates or junctures approach.
Finally, Gutheil and Schetky state that “accepting the patient’s pain and sense
of hopelessness is not the same as acceding to his or her wish to commit
suicide; the psychiatrist must always hold out hope. At the same time, it may be
therapeutic and realistic to let patients know that one can not ultimately
prevent their suicides” (Gutheil and Schetky, 1998).
Related Topics