Chapter: Medical Surgical Nursing: Assessment of Musculoskeletal Function
Assessment of Musculoskeletal Function: Physical Assessment
PHYSICAL ASSESSMENT
An examination of the
musculoskeletal system ranges from a basic assessment of functional
capabilities to sophisticated physical ex-amination maneuvers that facilitate
diagnosis of specific bone, muscle, and joint disorders (Chart 66-2). The
extent of assess-ment depends on the patient’s physical complaints, health
his-tory, and physical clues that warrant further exploration. The nursing
assessment is primarily a functional evaluation, focusing on the patient’s
ability to perform activities of daily living.
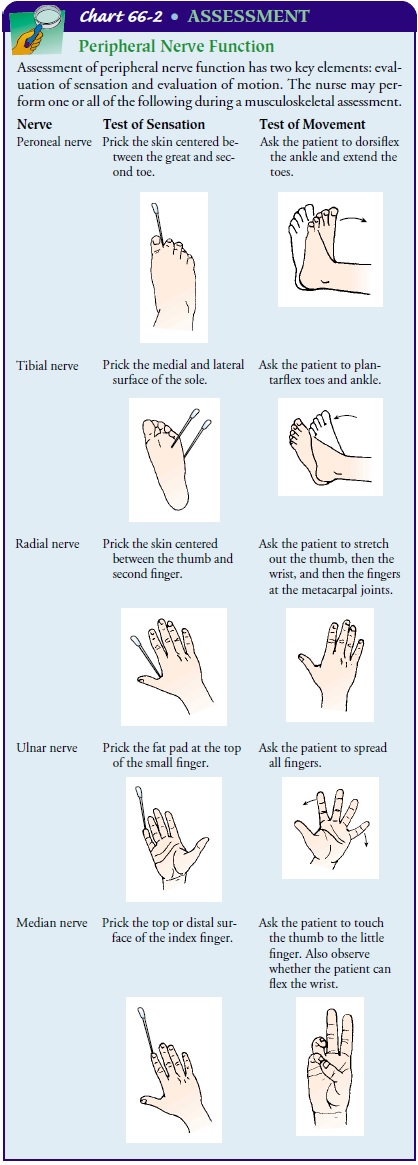
Techniques of inspection
and palpation are used to evaluate the patient’s posture, gait, bone integrity,
joint function, and muscle strength and size. In addition, assessing the skin
and neu-rovascular status is an important part of a complete musculo-skeletal
assessment. The nurse also should understand and be able to perform correct
assessment techniques on patients with mus-culoskeletal trauma. When specific
symptoms or physical findings of musculoskeletal dysfunction are apparent, the
nurse carefullydocuments the examination findings and shares the
information with the physician, who may decide that more extensive exami-nation
and diagnostic workup are necessary.
Posture
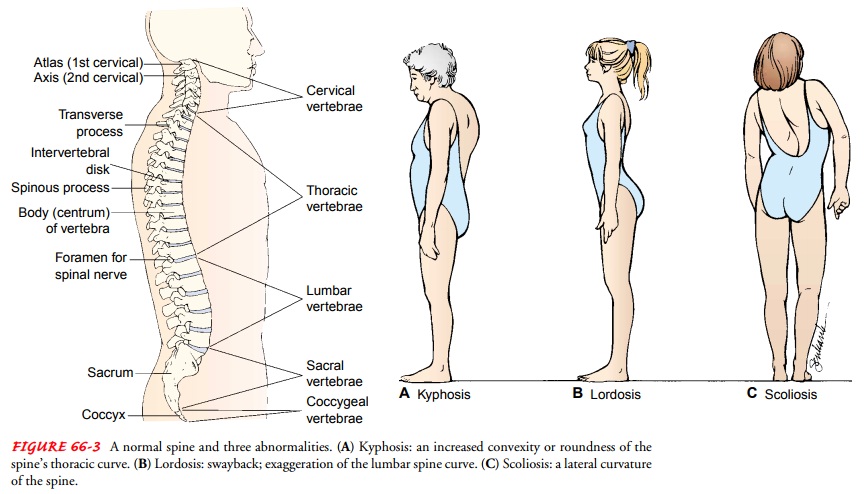
The normal curvature of
the spine is convex through the thoracic portion and concave through the
cervical and lumbar portions. Common deformities of the spine include kyphosis, an increased forward
curvature of the thoracic spine; lordosis,
or swayback, an exaggerated curvature of the lumbar spine; and scoliosis, a lat-eral curving deviation
of the spine (Fig. 66-3). Kyphosis is fre-quently seen in elderly patients with
osteoporosis and in some patients with neuromuscular diseases. Scoliosis may be
congeni-tal, idiopathic (without an identifiable cause), or the result of
damage to the paraspinal muscles, as in poliomyelitis. Lordosis is frequently
seen during pregnancy as the woman adjusts her pos-ture in response to changes
in her center of gravity.
During inspection of the spine, the entire back, buttocks, and legs are exposed. The examiner inspects the spinal curves and trunk symmetry from posterior and lateral views. Standing be-hind the patient, the examiner notes any differences in the height of the shoulders or iliac crests. The gluteal folds are normally symmetric. Shoulder and hip symmetry, as well as the line of the vertebral column, are inspected with the patient erect and with the patient bending forward (flexion).
(Scoliosis is evidenced by an abnormal lateral curve in the spine,
shoulders that are not level, an asymmetric waistline, and a prominent scapula,
accen-tuated by bending forward.) Older adults experience a loss in height due
to loss of vertebral cartilage and osteoporosis-related vertebral fractures.
Therefore, an adult’s height should be mea-sured periodically.
Gait
Gait is assessed by
having the patient walk away from the exam-iner for a short distance. The
examiner observes the patient’s gait for smoothness and rhythm. Any
unsteadiness or irregular move-ments (frequently noted in elderly patients) are
considered ab-normal. When a limping motion is noted, it is most frequently
caused by painful weight bearing. In such instances, the patient can usually
pinpoint the area of discomfort, thus guiding further examination. If one
extremity is shorter than another, a limp may also be observed as the patient’s
pelvis drops downward on the affected side with each step. Limited joint motion
may affect gait. In addition, a variety of neurologic conditions are associated
with abnormal gaits such as a spastic hemiparesis gait (stroke), steppage gait
(lower motor neuron disease), and shuffling gait (Parkinson’s disease).
Bone Integrity
The bony skeleton is
assessed for deformities and alignment. Symmetric parts of the body are
compared. Abnormal bony growths due to bone tumors may be observed. Shortened
ex-tremities, amputations, and body parts that are not in anatomic alignment
are noted. Fracture findings may include abnormal an-gulation of long bones,
motion at points other than joints, and crepitus (a grating sound) at the point
of abnormal motion. Movement of fracture fragments must be minimized to avoid
ad-ditional injury.
Joint Function
The articular system is evaluated by noting range of
motion, de-formity, stability, and nodular formation. Range of motion is
evaluated both actively (the joint is moved by the muscles sur-rounding the
joint) and passively (the joint is moved by the ex-aminer). The examiner is
familiar with the normal range of motion of major joints. Precise measurement
of range of motion can be made by a goniometer (a protractor de-signed for
evaluating joint motion). Limited range of motion may be the result of skeletal
deformity, joint pathology, or contrac-ture
of the surrounding muscles, tendons, and joint capsule. Inelderly patients,
limitations of range of motion associated with osteoarthritis (degenerative joint disease) may reduce their
abil-ity to perform activities of daily living.
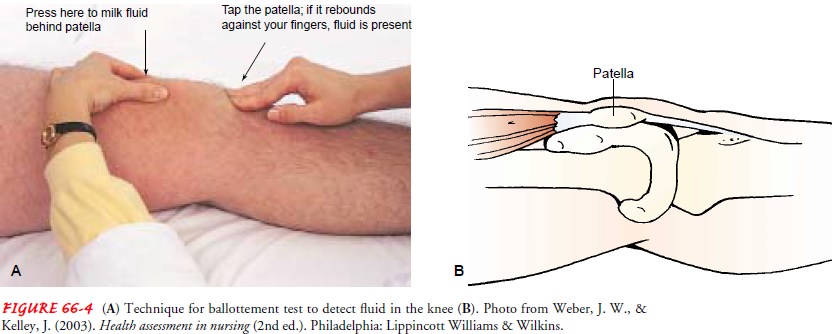
If joint motion is compromised or the joint is painful, the joint is examined for effusion (excessive fluid within the capsule), swelling, and increased temperature that may reflect active in-flammation. An effusion is suspected if the joint is swollen and the normal bony landmarks are obscured. The most common site for joint effusion is the knee. If a small amount of fluid is present in the joint spaces beneath the patella, it may be identified by the following maneuver. The medial and lateral aspects of the ex-tended knee are milked firmly in a downward motion. This dis-places any fluid downward.
As pressure is exerted against the medial or lateral side,
the examiner observes the opposite side for a bulge below the patella. When larger
amounts of fluid are pres-ent, the patella becomes elevated from the femur
during knee ex-tension and the ballottement test is positive (Fig. 66-4). If
inflammation or fluid is suspected in a joint, physician consulta-tion is
indicated.
Joint deformity may be caused by contracture (shortening of surrounding joint structures), dislocation (complete separation of joint surfaces), subluxation (partial separation of articular sur-faces), or disruption of structures surrounding the joint. Weakness or disruption of joint-supporting structures may result in a weak joint that requires an external supporting appliance (eg, brace).
Palpation of the joint
while it is passively moved provides in-formation about the integrity of the
joint. Normally, the joint moves smoothly. A snap or crack may indicate that a
ligament is slipping over a bony prominence. Slightly roughened surfaces, as in
arthritic conditions, result in crepitus
(grating, crackling sound or sensation) as the irregular joint surfaces move
across one another.
The tissues surrounding joints are examined for nodule for-mation. Rheumatoid arthritis, gout, and osteoarthritis produce characteristic nodules. The subcutaneous nodules of rheumatoid arthritis are soft and occur within and along tendons that provide extensor function to the joints. The nodules of gout are hard and lie within and immediately adjacent to the joint capsule itself.
They may rupture, exuding white uric acid crystals onto
the skin surface. Osteoarthritic nodules are hard and painless and repre-sent
bony overgrowth that has resulted from destruction of the cartilaginous surface
of bone within the joint capsule. They are frequently seen in older adults.
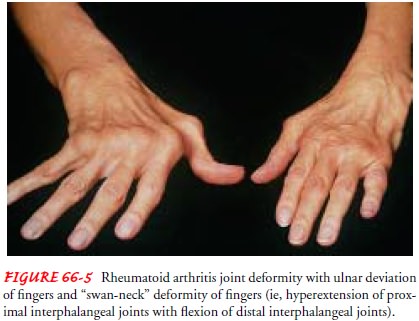
Often, the size of the joint is exaggerated by atrophy of
the muscles proximal and distal to that joint. This is seen in rheuma-toid
arthritis of the knees, in which the quadriceps muscle may atrophy
dramatically. In rheumatoid arthritis, joint involvement assumes a symmetric
pattern (Fig. 66-5).
Muscle Strength and Size
The muscular system is
assessed by noting the patient’s ability to change position, muscular strength
and coordination, and the size of individual muscles. Weakness of a group of
muscles might indicate a variety of conditions, such as polyneuropathy,
electrolyte disturbances (particularly potassium and calcium), myasthenia
gravis, poliomyelitis, and muscular dystrophy. By palpating the muscle while
passively moving the relaxed ex-tremity, the nurse can determine the muscle
tone. The nurse as-sesses muscle strength by having the patient perform certain
maneuvers with and without added resistance. For example, when the biceps are
tested, the patient is asked to extend the arm fully and then to flex it
against resistance applied by the nurse. A simple handshake may provide an
indication of grasp strength.
The nurse may elicit muscle clonus (rhythmic contractions of a muscle) in the ankle or wrist by
sudden, forceful, sustained dorsiflexion of the foot or extension of the wrist.
Fasciculations (involuntary
twitching of muscle fiber groups) may be observed.
The nurse measures the girth of an extremity to monitor in-creased size due to exercise, edema, or bleeding into the muscle. Girth may decrease due to muscle atrophy. The unaffected ex-tremity is measured and used as the reference standard. Measure-ments are taken at the maximum circumference of the extremity. It is important that the measurements be taken at the same loca-tion on the extremity, and with the extremity in the same position, with the muscle at rest. Distance from a specific anatomic land-mark (eg, 10 cm below the medial aspect of the knee for mea-surement of the calf muscle) should be indicated in the patient’s record so that subsequent measurements can be made at the same point. For ease of serial assessment, the nurse may indicate the point of measurement by marking the skin. Variations in size greater than 1 cm are considered significant.
Skin
In addition to assessing
the musculoskeletal system, the nurse in-spects the skin for edema,
temperature, and color. Palpation of the skin can reveal whether any areas are
warmer, suggesting increased perfusion or infection, or cooler, suggesting
decreased perfusion, and whether edema is present. Cuts, bruises, skin color,
and evi-dence of decreased circulation or infection can influence nursing
management of musculoskeletal conditions.
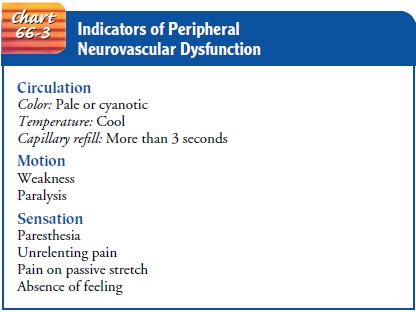
Neurovascular Status
It is important for the
nurse to perform frequent neurovascular assessments of patients with
musculoskeletal disorders (especially of those with fractures) because of the
risk of tissue and nerve dam-age. One complication that the nurse needs to be
alert for when assessing the patient is compartment syndrome, which is
described in detail later in this unit. This major neurovascular problem is
caused by pressure within a muscle compartment that increases to such an extent
that microcirculation diminishes, leading to nerve and muscle anoxia and
necrosis. Function can be permanently lost if the anoxic situation continues
for longer than 6 hours. Assessment of neurovascular status (Chart 66-3) is
frequently re-ferred to as assessment of CMS (circulation, motion, and
sensation).
The Patient With Musculoskeletal Injury
Special precautions must be taken when assessing a trauma pa-tient. If there is injury to an extremity, it is important to assess for soft tissue trauma, deformity, and neurovascular status. If the pa-tient has a possible cervical spine injury and is wearing a cervical collar, the collar must not be removed until the absence of spinal cord injury is confirmed on x-ray. When the collar is removed, the cervical spine area is gently assessed for swelling, tenderness, and deformity. With pelvic trauma, abdominal organ injuries may occur. The patient is assessed for abdominal pain, tender-ness, hematomas, and the presence or absence of femoral pulses. If blood is present at the urinary meatus, the nurse should sus-pect bladder and urethral injury, and the patient should not be catheterized. Instead, such findings should be reported imme-diately to the primary health care provider.
Related Topics