Chapter: Medical Surgical Nursing: Assessment of Immune Function
Assessment of Immune Function
Assessment
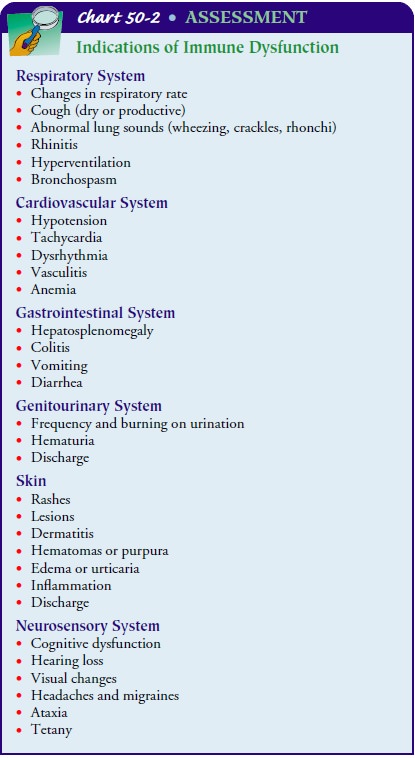
An
assessment of immune function begins with a health history and physical
examination. The history should note the patient’s age along with information
about past and present conditions and events that may provide clues to the
status of the patient’s immune system. Areas to be addressed include
nutritional sta-tus; infections and immunizations; allergies; disorder and
disease states, such as autoimmune disorders, cancer, and chronic ill-nesses;
surgery; medications; and blood transfusions. Physical as-sessment includes
palpation of the lymph nodes and examination of the skin, mucous membranes, and
respiratory, gastrointes-tinal, genitourinary, cardiovascular, and neurosensory
systems (Chart 50-2).
HEALTH HISTORY
Age
Age is
an important factor to elicit from the patient as people at the extremes of the
life span are more likely to develop problems related to immune system
functioning than are those in their middle years (Table 50-5).
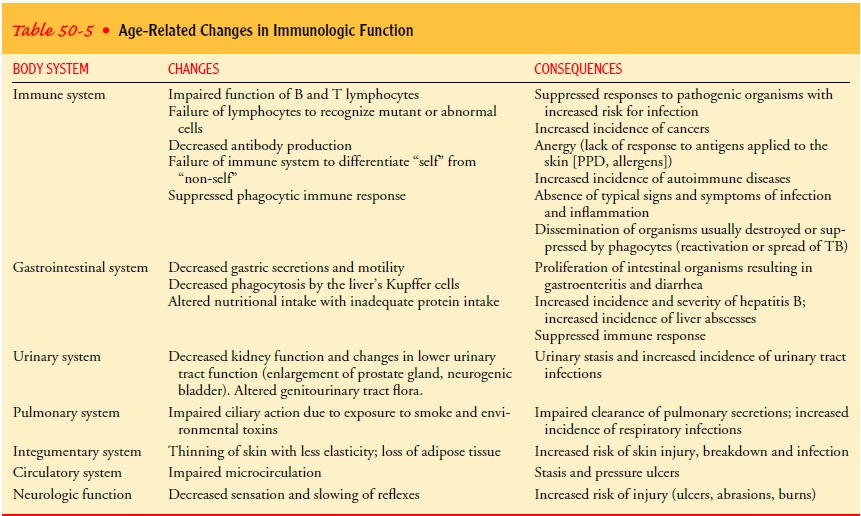
Gerontological Considerations
The frequency and severity of infections are
increased in elderly people, possibly due to a decreased ability to respond
adequately to invading organisms. Both the production and the function of T and
B lymphocytes may be impaired. Responses to antigen stimulation may be altered,
with increasing proportions of lym-phocytes becoming unresponsive with age
(Porth, 2002). The in-cidence of autoimmune diseases also increases with aging,
possibly from a decreased ability of antibodies to differentiate between self
and nonself. Failure of the surveillance system to recognize mu-tant, or
abnormal, cells may be responsible for the high incidence of cancer associated
with increasing age.
Declining function of various organ systems associated with increasing age also contributes to impaired immunity. Decreased gastric secretions and motility allow normal intestinal flora to proliferate and produce infection, causing gastroenteritis and di-arrhea. Decreased renal circulation, filtration, absorption, and ex-cretion contribute to risk for urinary tract infections. Moreover, prostatic enlargement and neurogenic bladder can impede urine passage and subsequently bacterial clearance through the urinary system. Urinary stasis, common in elderly people, permits the growth of microorganisms. Exposure to tobacco and environ-mental toxins impairs pulmonary function. Prolonged exposure to these agents decreases the elasticity of lung tissue, the effecttiveness of cilia, and the ability to cough effectively. These im-pairments hinder the removal of infectious organisms and toxins, increasing the elderly person’s susceptibility to pulmonary infec-tions and cancers.
Finally, with aging, the skin becomes thinner
and less elastic. Peripheral neuropathy and the accompanying decreased
sensa-tion and circulation may lead to stasis ulcers, pressure ulcers,
abrasions, and burns. Impaired skin integrity predisposes the aging person to
infection from organisms that are part of normal skin flora.
Nutrition
The nurse assesses the patient’s nutritional status, including caloric intake as well as the type of calories that the patient is consuming. Adequate nutrition is essential for optimal functioning of the im-mune system. Inadequate intake of vitamins that are essential for DNA and protein synthesis may lead to protein-calorie deficiency and subsequently to impaired immune function. Vitamins also help in the regulation of cell proliferation and maturation of im-mune cells. Excess or deficiency of trace elements (ie, copper, iron, manganese, selenium, or zinc) in the diet generally suppresses immune function.
Fatty acids are the building blocks that make
up the structural components of cell membranes. Lipids are precursors of
vitamins A, D, E, and K as well as cholesterol. Both excess and deficiency of
fatty acids have been found to suppress immune function.
Depletion
of protein reserves results in atrophy of lymphoid tissues, depression of
antibody response, reduction in the num-ber of circulating T cells, and
impaired phagocytic function. As a result, susceptibility to infection is
greatly increased. During pe-riods of infection and serious illness,
nutritional requirements may be exaggerated further, potentially contributing
to depletion of protein, fatty acid, vitamin, and trace elements and an even
greater risk of impaired immune response and sepsis.
Infection and Immunization
The patient is asked about immunizations
(including those re-ceived recently and those received in childhood) and the
usual childhood diseases. Known past or present exposure to tubercu-losis is
assessed, and the dates and results of any tuberculin tests (purified protein
derivative [PPD] or tine test) and chest x-rays are obtained. Recent patient
exposure to any infections and the exposure dates are elicited. It is important
for the nurse to assess whether the patient has been exposed to any sexually
transmitted diseases and bloodborne pathogens such as hepatitis A, B, C, D, and
E infections, and HIV infection. A history of sexually trans-mitted diseases,
such as gonorrhea, syphilis, HPV infection, and chlamydia, can alert the nurse
that the patient may have been ex-posed to HIV infection or hepatitis. A
history of past and present infections and the dates
and types of treatments that were used, along with a history of any multiple
persistent infections, fevers of unknown origin, lesions or sores, or any type
of drainage, are obtained.
Allergy
The
patient is asked about history of any allergies, including types of allergens
(pollens, dust, plants, cosmetics, food, med-ications, vaccines), the symptoms
experienced, and seasonal vari-ations in occurrence or severity in the
symptoms. A history of testing and treatments that the patient has received or
is cur-rently receiving for these allergies and the effectiveness of the
treatments is obtained. All medication and food allergies are listed on an
allergy alert sticker and placed on the front of the patient’s health record or
chart to alert others to the possibility of these allergies. Continued
assessment for potential allergic reactions in this patient is vital.
Disorders and Diseases
AUTOIMMUNE DISORDERS
The patient is asked about any autoimmune
disorders, such as lupus erythematosus, rheumatoid arthritis, or psoriasis. The
on-set, severity, remissions and exacerbations, functional limitations,
treatments that the patient has received or is currently receiving, and the
effectiveness of the treatments are described. Although most autoimmune
disorders are individually rare, together they affect approximately 5% of the U.S.
population. The occurrence of different autoimmune diseases within a family
strongly sug-gests a genetic predisposition to more than one autoimmune
dis-ease (Davidson & Diamond, 2001).
In general, autoimmune disorders are more
common in fe-males than in males. This is believed to be the result of the
ac-tivity of the sex hormones. The ability of sex hormones to modulate immunity
has been well established. There is evi-dence that estrogen modulates the
activity of T lymphocytes (especially suppressor cells), whereas androgens act
to preserve IL-2 production and suppressor cell activity. The effects of sex
hormones on B cells are less pronounced. Estrogen activates the
autoimmune-associated B-cell population that expresses the CD5 marker (an
antigenic marker on the B cell). Estrogen tends to enhance immunity, whereas
androgen tends to be immunosuppressive.
NEOPLASTIC DISEASE
A
history of cancer in the patient is obtained, along with the type of cancer and
date of diagnosis. Dates and results of any cancer screening tests are also
obtained.
Immunosuppression contributes to the
development of can-cers; however, cancer itself is immunosuppressive. Large
tumors can release antigens into the blood, and these antigens combine with
circulating antibodies and prevent them from attacking the tumor cells.
Furthermore, tumor cells may possess special block-ing factors that coat tumor
cells and prevent destruction by killer T lymphocytes. During the early
development of tumors, the body may fail to recognize the tumor antigens as
foreign and sub-sequently fail to initiate destruction of the malignant cells.
Hema-tologic cancers, such as leukemia and lymphoma, are associated with
altered production and function of WBCs and lymphocytes.
All treatments that the patient has received
or is currently re-ceiving, such as radiation or chemotherapy, are identified
and doc-umented in the health history. Radiation destroys lymphocytes and
decreases the population of cells required to replace them. The size or extent
of the irradiated area determines the extent of im-munosuppression. Whole-body
irradiation may leave the patient totally immunosuppressed. Chemotherapy also
destroys immune cells and causes immunosuppression.
A family history of cancer is obtained. If there is a family his-tory of cancer, the type of cancer, age of onset, and relationship (maternal or paternal) of the patient to the affected family mem-ber is noted. (See Genetics in Nursing Practice.)
CHRONIC ILLNESS AND SURGERY
The health assessment includes a history of
chronic illnesses, such as diabetes mellitus, renal disease, or chronic
obstructive pul-monary disease. The onset and severity of illnesses, as well as
treat-ment that the patient is receiving for the illness, are obtained. Chronic
illness may contribute to immune system impairments in various ways. Renal
failure is associated with a deficiency in circulating lymphocytes. In addition, immune
defenses may be al-tered by acidosis and uremic toxins. In diabetes, an
increased incidence of infection has been associated with vascular
insuffi-ciency, neuropathy, and poor control of serum glucose levels.
Re-current respiratory tract infections are associated with chronic obstructive
pulmonary disease as a result of altered inspiratory and expiratory function
and ineffective airway clearance. Additionally, a history of surgical removal
of the spleen, lymph nodes, or thy-mus or a history of organ transplantation is
noted because these conditions may place the patient at risk for impaired immune
function.
SPECIAL PROBLEMS
Conditions
such as burns and other forms of injury and infection may contribute to altered
immune system function. Major burns or other factors cause impaired skin
integrity and compromise the body’s first line of defense. Loss of large
amounts of serum with burn injuries depletes the body of essential proteins,
including immunoglobulins. The physiologic and psychological stressors
associated with surgery or injury stimulate cortisol release from the adrenal
cortex; increased serum cortisol also contributes to suppression of normal
immune responses.
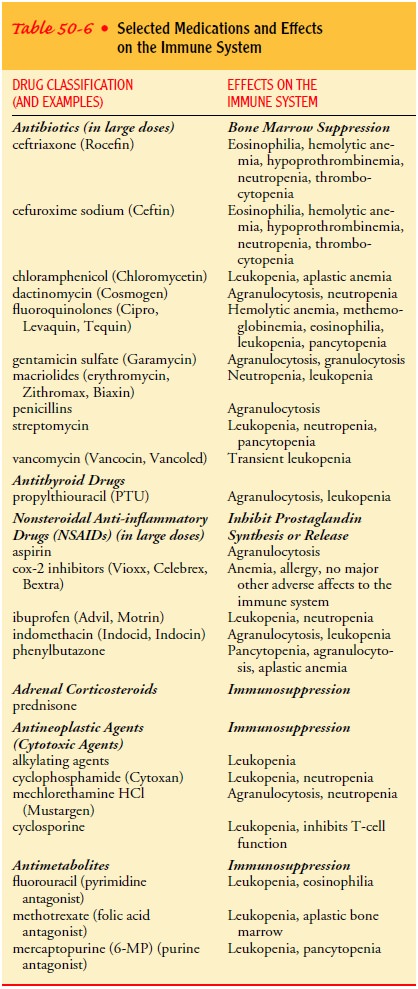
Medications and Blood Transfusions
A list
of past and present medications is obtained. In large doses, an-tibiotics,
corticosteroids, cytotoxic agents, salicylates, nonsteroidal anti-inflammatory
drugs (NSAIDs), and anesthetics can cause immune suppression (Table 50-6).
A
history of blood transfusions is obtained because previous exposure to foreign
antigens through transfusion may be associ-ated with abnormal immune function.
Additionally, although the risk of human immunodeficiency virus (HIV)
transmission through blood transfusion is extremely low in patients who
re-ceived a transfusion after 1985 (the year that testing of blood for HIV was
initiated in the United States), a risk still exists.
The
patient is also asked about use of herbal agents and over-the-counter
medications. Because many of these products have not been subjected to rigorous
testing, not all of their effects have been identified. It is important,
therefore, to ask patients about their use of these substances and to document
their use.
Lifestyle and Other Factors
Like any other body system, the immune system functions de-pend on other body systems. A detailed history of smoking, alco-hol consumption, dietary intake and nutritional status, amount of perceived stress, injection drug use, sexual practices, sexually transmitted diseases, and occupational or residential exposure to radiation or pollutants is obtained. Poor nutritional status, smok-ing, excessive consumption of alcohol, injection drug use, sexu-ally transmitted diseases, and exposure to environmental radiation and pollutants have been associated with impaired immune func-tion and are assessed in the patient history.
PSYCHONEUROIMMUNOLOGIC FACTORS
The assessment also addresses
psychoneuroimmunologic factors. It is thought that the immune response is
regulated and modu-lated in part by neuroendocrine influences. Lymphocytes and
macrophages have receptors capable of responding to neuro-transmitters and
endocrine hormones. Lymphocytes can produce and secrete adrenocorticotropic
hormone and endorphin-like compounds. Neurons in the brain, especially in the
hypothala-mus, can recognize prostaglandins, interferons, and interleukins as
well as histamine and serotonin, which are released during the inflammatory
process. Like all other biologic systems functioning in the interest of
homeostasis, the immune system is integrated with other psychophysiologic
processes and is subject to regula-tion and modulation by the brain.
Conversely, the immune processes can affect
neural and en-docrine function, including behavior. Thus, the interaction of
the nervous system and immune system appears to be bidirectional. Growing
evidence indicates that measurable immune system para-meters can be influenced
by biobehavioral strategies involving self-regulation. Examples of these
strategies are relaxation and imagery techniques, biofeedback, humor, hypnosis,
and conditioning. The assessment should address the patient’s general psychological
sta-tus and the patient’s use of these strategies.
PHYSICAL EXAMINATION
On physical examination (see Chart 50-2), the
skin and mucous membranes are assessed for lesions, dermatitis, purpura
(subcuta-neous bleeding), urticaria, inflammation, or any discharge. Any signs
of infection are noted. The patient’s temperature is recorded, and the patient
is observed for chills and sweating. The anterior and posterior cervical,
axillary, and inguinal lymph nodes are pal-pated for enlargement; if palpable
nodes are detected, the location, size, consistency, and reports of tenderness
upon palpation are noted. Joints are assessed for tenderness and swelling and
for lim-ited range of motion. The patient’s respiratory, cardiovascular,
gastrointestinal, genitourinary, and neurosensory status is evaluated for signs and
symptoms indicative of immune dysfunction. The patient’s nutritional status,
level of stress, and coping ability are also assessed, along with his or her
age and any functional lim-itations or disabilities.
Related Topics