Chapter: Essentials of Psychiatry: Substance Abuse: Cannabis-related Disorders
Assessment and Differential Diagnosis - Cannabis-related Disorders
Assessment and Differential
Diagnosis
Cannabis-related Disorders
To diagnose any of the cannabis-related disorders,
it is impor-tant to obtain a detailed history of the individual’s pattern of
substance abuse (including abuse not only of cannabis but of other substances)
and to attempt to substantiate this report with toxicology screening for drugs
of abuse. Individuals who smoke cannabis regularly can have substantial
accumulations of THC in their fat stores. Thus, for weeks after cessation of
smoking, de- tectable levels of cannabinoids may be found in urine (Johnson,
1990). However, a positive response on toxicology screening for cannabinoids
cannot establish any of the cannabis-related diag-noses; it is useful only as
an indicator that these diagnoses should be considered.
Cannabis Dependence
It is uncommon to see patients who exhibit cannabis
depend-ence as their only diagnosis because such individuals rarely seek
treatment as they generally do not acknowledge that they have a problem and are
unaware that treatment is available. However, some patients with this disorder
will respond to offers for treat-ment because they realize that they are unable
to stop use on their own and because they notice the deleterious effect of
compulsive use (Roffman and Barnhart, 1987). Therefore, the diagnosis of
cannabis dependence will most often be made in patients who present with other
psychiatric problems, such as mood and anxi-ety disorders, and other substance
use disorders. Another manner in which individuals with cannabis dependence may
come to the attention of psychiatrists is when they are arrested for possession
of the substance or some crime related to cannabis abuse, such as driving under
the influence of the drug. Nevertheless, cannabis dependence is probably
underdiagnosed in both psychiatric and general medical populations because it
is not considered.
The diagnosis of cannabis dependence cannot be made
without obtaining a history indicating that the cannabis use is impairing the
patient’s ability to function either physically or psychologically. Areas to
inquire about include the patient’s per-formance at work, ability to carry out
social and family obliga-tions, and physical health. It is also important to
find out how much of the patient’s time is spent on cannabis-related activities
and whether the patient has tried unsuccessfully to stop or cut down on use in
the past. Although it has been our experience that people who have used
cannabis daily over a period of years almost invariably report tolerance to
many of the effects of can-nabis and to experience an unpleasant withdrawal
state if use is discontinued, neither tolerance nor withdrawal is necessary for
the diagnosis of cannabis dependence. When this diagnosis is made, it can be
described further by the following specifiers: with or without physiological
dependence, early full or partial remission, sustained full or partial
remission, or in a controlled environment. These diagnostic distinctions must
be based on the pattern of use reported by the patient.
Cannabis Abuse
Most individuals who are diagnosed with cannabis
abuse have only recently started using cannabis. As with cannabis depend-ence,
cannabis abuse is unlikely to be diagnosed unless some additional condition or
circumstance brings the individual to medical attention. Teenagers often fall
into this category because they spend time in supervised environments like
school and home where responsible adults may intervene. Also, teenagers are
more likely to have motor vehicle accidents while intoxicated because they are
inexperienced drivers, and are more likely to be arrested for possession
because they have a greater tendency to participate in risky behaviors of all
types.
Although virtually all individuals with cannabis
depend-ence meet the inclusion criteria for cannabis abuse, they cannot be
given this diagnosis because the presence of cannabis depend-ence is an
exclusion criterion. Undoubtedly, the vast majority of people with cannabis
dependence would have been given the diagnosis of cannabis abuse until they
developed dependence.
It is probable that individuals qualifying for a
diagnosis of can-nabis abuse will either cease use or develop cannabis
dependence. The criteria for cannabis abuse focus on adverse consequences of
cannabis use that could potentially re-sult from just a single use such as
failure to fulfill obligations at work, school, or home, participating in
potentially dangerous activities like driving while intoxicated with cannabis,
having cannabis-related legal problems, or social or interpersonal
dif-ficulties. Even though these adverse consequences can occur following a
single episode of cannabis use, the consequences must be recurrent, requiring
multiple episodes of use. Since the number of episodes necessary for
“recurrent” is not defined, and the pattern of use is often dependent on
patient self-report, it is often difficult to distinguish between abuse and
dependence. This difficulty is easier to recognize if one looks at the
extremes. On one end of the continuum, a high school student who actually has
only used cannabis twice, but who was unfortunate enough to be caught and
suspended from school on both occasions, would appropriately be diagnosed with
cannabis abuse. At the other end of the continuum, a high school student who
had actually been using cannabis every day for three years and met the criteria
for dependence, who was also caught and suspended from school twice but denied
symptoms of dependence, would incorrectly be diagnosed with cannabis abuse.
The difference between people with cannabis abuse
and those with cannabis dependence is that the people with depend-ence have
been using more regularly (one or more times per day) and for a longer duration
(one or more years), and the acute prob-lems associated with abuse have turned
into the chronic problems associated with dependence. For example, what started
as failure to fulfill obligations at work or school has resulted in dropping
out of school or working at jobs with extremely low expectations. Multiple car
accidents or arrests have led to chronic injuries (of-ten associated with
obtaining SSDI), loss of licenses, probation and even periods of time in
prison. Social or interpersonal prob-lems have resulted in isolation or at
least separation from people who are not regular cannabis users. If there is a
committed rela-tionship where the partner is typically cannabis dependent, and
if children are involved, chronic neglect is present if caring for children
while intoxicated with cannabis represents neglect.
Cannabis Intoxication
There are four criteria necessary to make this
diagnosis (see DSM-IV criteria for intoxication). The first is that recent use
of cannabis must be established. This cannot be done with toxicol-ogy screening
because the result may be negative after a single episode of smoking or,
alternatively, may be positive even if the individual has not used the drug for
a time much longer than the period of intoxication (see section on Cannabis
botany and phar-macology). Thus, the recent use of cannabis must be reported by
the patient or another person who witnessed the patient’s use. In addition, the
symptoms resulting from cannabis use must pro-duce “clinically significant
maladaptive behavioral or psycho-logical changes”. Thirdly, the patient must
exhibit some physical signs of cannabis use. DSM-IV-TR requires the patient to
have at least two of four signs – conjunctival injection, increased ap-petite,
dry mouth and tachycardia – within 2 hours of cannabis use. Fourthly, symptoms
cannot be accounted for by a general medical condition or another mental
disorder. There is a specifier, “with perceptual disturbances”, that can be
used if the patient is experiencing illusions or hallucinations while not
delirious and while maintaining intact reality testing.
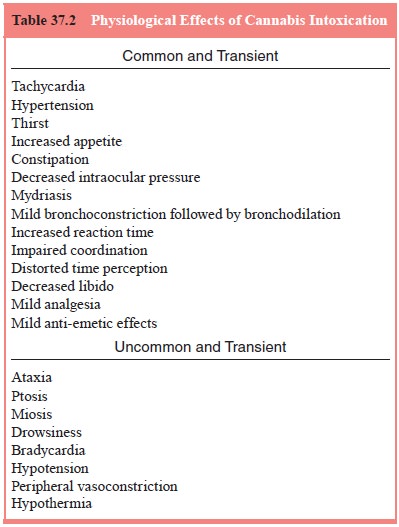
There has been extensive research on the effects of
acute cannabis intoxication. In addition to the symptoms and signs required for
a DSM-IV-TR diagnosis, many psychological and physiological effects have been
reported. Awareness of these may enhance the psychiatrist’s ability to
recognize cannabis intoxica-tion. Physiological effects are listed in Table
37.2, and are divided into commonly observed effects and rare effects that have
been described only after the use of very high doses of cannabis (Hall and
Solowij, 1998; Ameri, 1999; Perez-Reyes, 1999). Cannabis has low toxicity, and
to our knowledge, no deaths from canna-bis overdose have been reported (Hall
and Solowij, 1998). Simi-larly, psychological effects are listed in Table 37.3,
divided into commonly observed effects and uncommon effects. Most people find
the commonly experienced psychological effects enjoyable. However, some
individuals, especially women (Thomas, 1996)
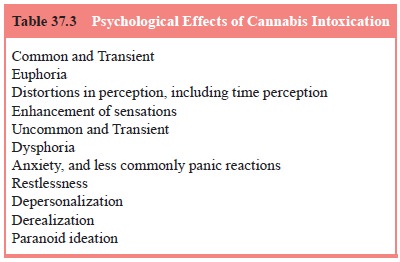
and inexperienced users in an unfamiliar
environment, find them frightening and experience anxiety and even have panic
reactions (Hall and Solowij, 1998; Johns, 2001; Thomas, 1996). Although all of
these effects typically persist only for the period of acute intoxication, some
reports have described individuals who report “flashbacks” of cannabis
intoxication long after use, and deper-sonalization persisting long after acute
intoxication (Keeler et al., 1968,
1971; Levi and Miller, 1990; Annis and Smart, 1973; Stanton and Bardoni, 1972).
At this time there is insufficient evidence to ascertain whether these reports
are attributable to cannabis itself, to confounding factors such as the
concomitant use of other drugs, or the presence of other Axis I disorders
(Johns, 2001).
In addition, cannabis use produces deficits in a
number of neuropsychological functions, both during acute intoxication and after
up to a week or more of abstinence in chronic, long-term users. These tasks
include short-term memory, sustained or divided attention, and complex
decision-making (Ehrenreich et al.,
1999; Pope et al., 1995, 1997, 2001a;
Pope and Yurgelun-Todd, 1996; Schwartz et
al., 1989; Solowij et al., 1991,
1995; Solowij, 1995, 1998). A study of chronic, long-term users found that
these deficits were reversible after 28 days of abstinence (Pope et al., 2001a). However, a few studies
have found that sub-tle electrophysiologic changes, of uncertain clinical
significance, may persist even after years of abstinence (Solowij, 1995, 1998;
Struve et al., 1998).
Cannabis Intoxication Delirium
We have not located any original reports of this
entity, although it is mentioned in various reviews and is included in DSM-IV.
Thus, if cannabis intoxication delirium does occur in neurologi-cally intact
individuals, it is probably a rare complication. If the delirium does not
resolve within 24 to 48 hours, it is almost cer-tainly a result of an
underlying neurological or medical condi-tion. Therefore, in a patient with
delirium, even if recent cannabis use has been reported, a full diagnostic
work-up should be per-formed to rule out a concomitant, treatable neurological
condi-tion (Halikas, 1974; Johns, 2001).
The following two substance-induced conditions are
not generally diagnosed unless the symptoms are in excess of those usually
associated with the intoxication or withdrawal state and are sufficiently
severe to warrant independent clinical attention.
Cannabis-induced Psychotic Disorder
There are two subtypes of cannabis-induced
psychotic disor-der: one featuring delusions, the other hallucinations. The
di-agnosis of this disorder is readily made in individuals who have psychotic
symptoms that appear immediately after ingestion of cannabis. However, a
careful history is required to establish whether the individual has a
preexisting psychotic disorder (as is often the case in such situations) or
whether the symptoms arose de novo after
cannabis consumption. There is little evi-dence that cannabis-induced psychotic
disorders can arise in previously asymptomatic individuals (Gruber and Pope,
1994). Therefore, if psychotic symptoms persist for 24 to 48 hours af-ter the
period of acute intoxication, they are likely due to an underlying psychiatric
disorder which must be diagnosed and treated (Hall and Degenhardt, 2000; Johns,
2001, Gruber and Pope, 1994).
Cannabis-induced Anxiety Disorder
This disorder may be further described by the following
specifiers: with generalized anxiety, with panic attacks, with
obsessive–compulsive
symptoms and with phobic symptoms. The literature contains papers that report
individuals who have anxiety, panic reactions and paranoid ideation during the
period of acute intoxication, but we are unaware of any papers that re-port obsessive–compulsive
or phobic symptoms. People who ex-perience anxiety after using cannabis are
typically inexperienced users who react to the novel experiences of perceptual
distortions and intensified sensations with anxiety and even panic reactions,
rather than enjoyment (Thomas, 1996; Johns, 2001; Szuster et al., 1988). Women are more likely than men to experience
canna-bis-induced anxiety (Thomas, 1996). As with cannabis-induced psychotic
disorders, we have been unable to find clear cases of cannabis-induced anxiety
disorders in individuals without a preexisting Axis I disorder. Again, if
symptoms of severe anxiety or panic persist for 24 to 48 hours after the period
of acute intoxi-cation, they are likely due to an underlying psychiatric
disorder that must be diagnosed and treated (Johns, 2001).
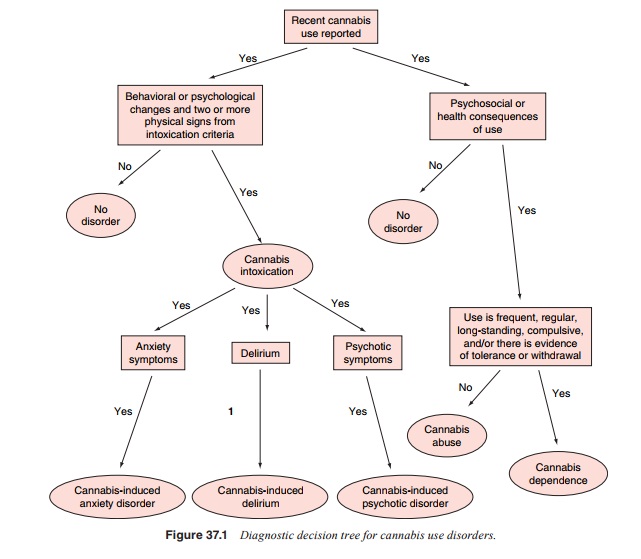
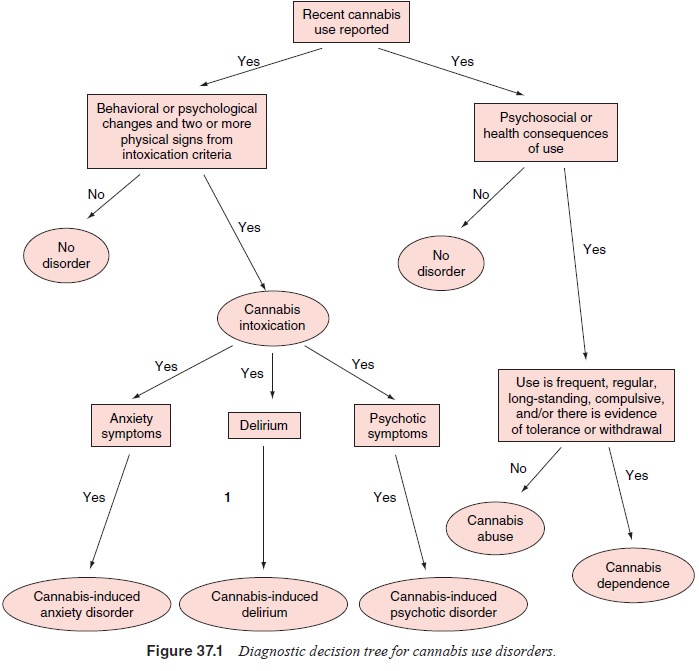
A
diagnostic decision tree for cannabis use disorders is presented in Figure
37.1.
Related Topics