Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Candida, Aspergillus, and Other Opportunistic Fungi
Aspergillosis : Clinical Aspects
ASPERGILLOSIS : CLINICAL ASPECTS
MANIFESTATIONS
Aspergillus can cause clinical allergies or occasional invasive infection. In both cases, thelung is the organ primarily involved. Allergic aspergillosis, which can be a mechanism of exacerbation in patients with asthma, is characterized by transient pulmonary infiltrates, eosinophilia, and a rise in Aspergillus-specific antibodies. These conditions follow direct inhalation of fungal elements or, more commonly, colonization of the respiratory tract. Areas of the bronchopulmonary tree with poor drainage because of underlying disease or anatomic abnormalities may serve as a site for growth of organisms and continuous seed-ing with antigen.
Invasive aspergillosis occurs in the settings of preexisting pulmonary disease (bronchiec-tasis, chronic bronchitis, asthma, tuberculosis) or immunosuppression. Colonization with Aspergillus can lead to invasion into the tissue by branching septate hyphae. In patients whoalready have a chronic pulmonary disease, mycelial masses can form a radiologically visible fungus ball (aspergilloma) within a preexisting cavity. Lung tissue invasion may penetrate blood vessels, causing hemoptysis or erosion into other structures with development of fistu-las. Invasive disease outside the lung is rare unless patients are immunocompromised.
An acute pneumonia may occur in severely immunocompromised patients, particu-larly those with phagocyte defects or depressed neutrophil counts due to immunosuppres-sive drugs. Multifocal pulmonary infiltrates expanding to consolidation are present with high fever. The prognosis is grave and dissemination to other organs common, which is not the case in immunocompetent hosts.
DIAGNOSIS
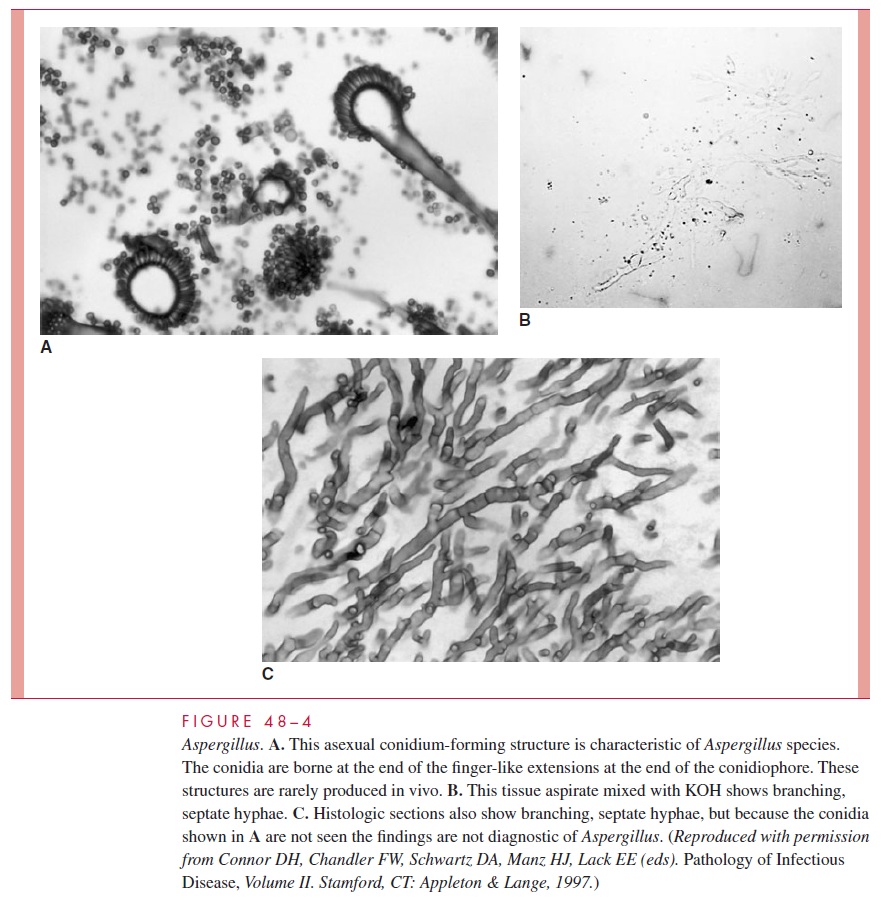
Aspergillus is relatively easy to isolate and identify. Its rapidly spreading mold growthand all too frequent contamination of cultures cause it to be regarded by microbiologists as a kind of weed. The diagnostic problem is distinguishing contamination and coloniza-tion with Aspergillus from invasive disease. The diagnosis cannot be made for certain without the use of lung aspiration, biopsy, or bronchoalveolar lavage. With material di-rectly from the lesion, the presence of large, branching, septate hyphae (Fig 48–4B and 48–4C) and a positive culture are diagnostic. Occasionally, the complete fruiting bodies are produced in vivo, creating a striking and diagnostic histologic picture (see Fig 48–4A). Serologic methods have been developed to demonstrate Aspergillus antibodies. Although these tests may be helpful in suggesting allergic aspergillosis, they have little value in invasive disease because anti-Aspergillus antibody is common in healthy persons.
TREATMENT AND PREVENTION
Amphotericin B and itraconazole are the recommended antimicrobics for invasive as-pergillosis. Neither can be considered particularly effective, because the mortality rate of invasive disease approaches 100%. In cases with pulmonary structural abnormalities and fungus balls, chemotherapy has little effect. Surgical removal of localized lesion is some-times helpful, even in the brain. Construction of rooms with filtered air has been at-tempted to reduce exposure to environmental conidia.
Related Topics