Chapter: Modern Pharmacology with Clinical Applications: Antipsychotic Drugs
Antipsychotic Drugs: Adverse Effects
ADVERSE EFFECTS
Antipsychotic drugs are
characterized by high thera-peutic indices with respect to mortality, but side
effects occur routinely at therapeutic doses, mostly as exten- sions of
pharmacological actions (Table 34.2). The char-acteristic neurological symptoms
(discussed next) caused by these agents are particularly troublesome, of-ten
limit the tolerated dose, and may interfere with the desired benefits and patient
compliance.
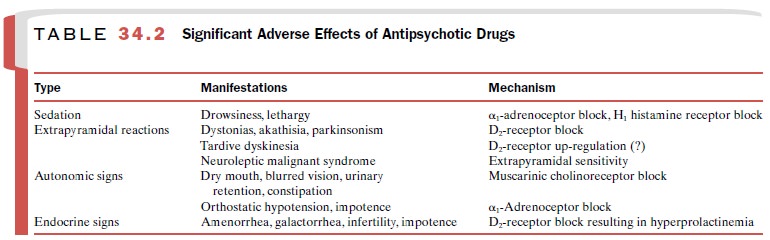
Sedation
Sedation is common after use
of all antipsychotic drugs and is especially notable with the low-potency
phenoth-iazines; this is a result of their activity at α1-adrenergic and H1-histaminergic
receptors. However, sedation de-creases during long-term treatment, and many
patients become tolerant to this effect. Single daily doses given at bedtime
minimize this problem.
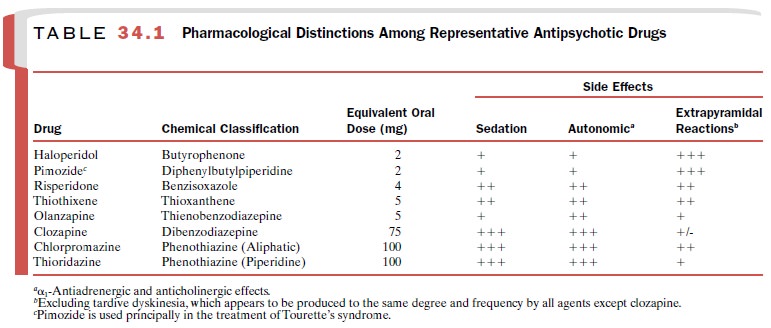
Extrapyramidal Reactions
Two extrapyramidal
conditions, acute dystonia and akathisia, occur early during treatment, while
parkinson-ism tends to evolve gradually over days to weeks. All three reactions
occur most commonly with the high-potency antipsychotics (Table 34.1) and are
related to high D2-receptor occupancy.Acute dystonia, which occurs
in about 5% of patients on antipsychotic therapy, consists of uncontrollable
movements and distortions of the face, head, and neck. It can be treated with
centrally acting an-timuscarinic agents, such as benztropine, while
antipsy-chotic therapy is temporarily discontinued. When this re-action
subsides, the anticholinergic can be withdrawn.
The incidence of akathisia is
about 20%; the syn-drome consists of intense motor restlessness and agi-tation
that contribute to a behavioral deterioration. It is frequently unresponsive to
anticholinergics and is more effectively treated with benzodiazepines and β-adrenergic antagonists, such
as propranolol.
Signs of parkinsonism—akinesia, tremor, rigidity— can develop gradually, but this reaction usually re-sponds favorably to central antimuscarinic agents. As with dystonia, parkinsonism may subside, permitting withdrawal of the antimuscarinic drug.
Tardive dyskinesia is a
late-occurring syndrome of abnormal movements of the face and tongue with
wide-spread choreoathetosis. It is the most serious adverse effect of the
antipsychotic drugs. It can be expected to occur in 20 to 40% of chronically
treated patients; there is no established treatment, and reversibility may be
limited. These reactions are more frequent and severe in the elderly.
Tardive dyskinesia is
generally accepted to be a D2 supersensitivity phenomenon, though
research has not unequivocally established this postulate. An appropri-ate
clinical response to these symptoms would be to re-duce the dose or discontinue
the antipsychotic agent and then eliminate all drugs with central
anticholinergic action, such as antidepressants. The rationale is to bal-ance
the risks of continuing treatment in a patient with tardive dyskinesia with the
benefits of antipsychotic ad-ministration. If these steps are not helpful,
clozapine therapy can be considered, or diazepam can be em-ployed to enhance
GABAergic activity. Prevention of this reaction is important. Generally,
antipsychotics should be prescribed in minimally effective doses and their use
reserved for time-limited treatment except in the treatment of chronic
schizophrenic disorders.
The neuroleptic malignant syndrome is a rare med-ical emergency
involving extrapyramidal symptoms that occurs in about 1% of patients receiving
antipsychotics. The concern is not the incidence but that about 10% of these
cases are fatal. The condition is marked by hyper-thermia or fever, diffuse
muscular rigidity with severe extrapyramidal effects, autonomic dysfunction
such as increased blood pressure and heart rate, and fluctuating levels of
consciousness. Neuroleptic malignant syn-drome is most common in males, with
about 80% of cases occurring in patients under 40 years of age. Treatment
should include general supportive measures, such as rehydration and body
cooling; antipsychotic therapy should be discontinued. Short-term therapy with
dantrolene in combination with antiparkinson agents such as bromocriptine has
been employed to control the muscular rigidity and hyperthermia.
Autonomic and Endocrine Effects
Most antipsychotics have both
α-adrenergic and cholin-ergic
antagonist activities, and blocking actions at hista-mine and serotonin
receptors also contribute to the au-tonomic effects of some agents. Postural
hypotension and depression of medullary cardiovascular centers re-sulting from α1-adrenoceptor blockade is
particularly troublesome in elderly or debilitated patients. β2-Agonists, such as
epinephrine, are contraindicated, as they may worsen the hypotension. The
anticholinergic effects can be very bothersome but usually subside as tolerance
to these effects occurs. Typically, autonomic signs can be controlled by
adjustment of dose.
All antipsychotics except
clozapine and perhaps olanzapine produce hyperprolactinemia by removing the
inhibitory actions of dopamine on prolactin secre-tion. This results in
amenorrhea, galactorrhea, and in-fertility in women and in loss of libido and
impotence in men. Inhibition of the release of follicle-stimulating and
luteinizing hormones may also play a role. In addition, weight gain is common,
and food intake must be moni-tored.
Other Adverse Effects
Cholestatic jaundice is
observed infrequently, usually during the first few weeks of treatment. This is
thought to be a hypersensitivity reaction and is usually mild and self-limited.
Cutaneous allergic reactions are occasion-ally reported. Both types of problems
normally disap-pear upon changing to an antipsychotic from a different chemical
class. Photosensitivity usually manifests as an acute hypersensitivity reaction
to sun with sunburn or rash, but the condition is generally mild and does not
re-quire dosage adjustment.
Opacities of the cornea and
lens due to deposition of fine particulate matter are a common complication of
chlorpromazine therapy but regress after drug with-drawal. The most serious ocular
complication is pigmen-tary retinopathy associated with high-dose thioridazine
administration; it is an irreversible condition leading to decreased visual
acuity and possibly blindness.
Agranulocytosis is a
potentially catastrophic idio-syncratic reaction that usually appears within
the first 3 months of therapy. Although the incidence is extremely low (except
for clozapine), mortality is high. Thus, any fever, sore throat, or cellulitis
is an indication for dis-continuing the antipsychotic and immediately
conduct-ing white blood cell and differential counts.
Contraindications for
antipsychotic therapy are few; they may include Parkinson’s disease, hepatic
fail-ure, hypotension, bone marrow depression, or use of CNS depressants.
Overdoses of antipsychotics are rarely fatal, except for thioridazine, which is
associated with major ventricular arrhythmias, cardiac conduction block, and
sudden death. For other agents gastric lavage should be attempted even if
several hours have elapsed since the drug was taken, because gastroin-testinal
motility is decreased and the tablets may still be in the stomach. Moreover,
activated charcoal effec-tively binds most of these drugs and can be followed
by a saline cathartic. The hypotension often responds to fluid replacement or
pressor agents such as norepi-nephrine.
Related Topics