Chapter: Clinical Anesthesiology: Clinical Pharmacology: Anticholinergic Drugs
Anticholinergic Drugs
Anticholinergic Drugs
One group of cholinergic antagonists has
already been discussed: the nondepolarizing neuromuscular-blocking agents.
These drugs act primarily at the nicotinic receptors in skeletal muscle.
MECHANISMS OF ACTION
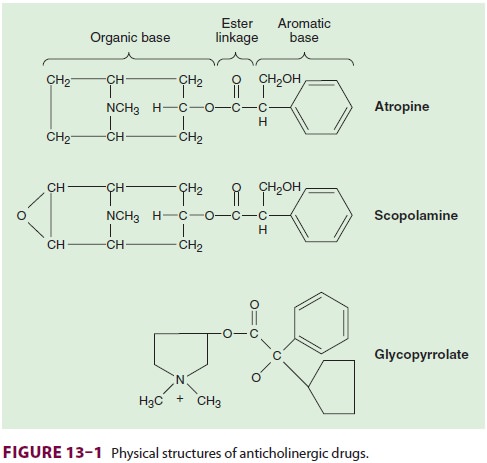
Anticholinergics are esters of an
aromatic acid combined with an organic base ( Figure 13–1). The ester linkage
is essential for effective binding ofthe anticholinergics to the acetylcholine
receptors.
This
competitively blocks binding by acetylcho-line and prevents receptor
activation. The
cellulareffects of acetylcholine, which are mediated through second messengers,
are inhibited. The tissue recep-tors vary in their sensitivity to blockade. In
fact, muscarinic receptors are not homogeneous, and receptor subgroups have
been identified including: neuronal (M1),
cardiac (M2), and glandular (M3) receptors.

CLINICAL PHARMACOLOGY
General Pharmacological Characteristics
In normal clinical doses, only
muscarinic receptors are blocked by the anticholinergic drugs discussed. The
extent of the anticholinergic effect depends on the degree of baseline vagal
tone. Several organ systems are affected.
A. Cardiovascular
Blockade of muscarinic receptors in the sinoatrial node produces tachycardia. This effect is especially useful in reversing bradycardia due to vagal reflexes (eg, baroreceptor reflex, peritoneal traction, or ocu-locardiac reflex). A transient slowing of heart rate in response to smaller intravenous doses of atropine (<0.4 mg) has been reported. The mechanism of this paradoxical response is unclear. Facilitation of conduction through the atrioventricular node short-ens the P–R interval on the electrocardiogram and often decreases heart block caused by vagal activity. Atrial arrhythmias and nodal (junctional) rhythms occasionally occur. Anticholinergics generally have little effect on ventricular function or peripheral vas-culature because of the paucity of direct cholinergic innervation of these areas despite the presence of cholinergic receptors. Presynaptic muscarinic recep-tors on adrenergic nerve terminals are known to inhibit norepinephrine release, so muscarinic antag-onists may modestly enhance sympathetic activity. Large doses of anticholinergic agents can result in dilation of cutaneous blood vessels (atropine flush).
B. Respiratory
The anticholinergics inhibit the
secretions of the respiratory tract mucosa, from the nose to the bron-chi, a
valuable property during airway endoscopic or surgical procedures. Relaxation
of the bron-chial smooth musculature reduces airway resistance and increases
anatomic dead space. These effects are particularly pronounced in patients with
chronic obstructive pulmonary disease or asthma.
C. Cerebral
Anticholinergic medications can cause a
spectrum of central nervous system effects ranging from stimula-tion to
depression, depending on drug choice and dos-age. Cerebral stimulation may
present as excitation, restlessness, or hallucinations. Cerebral depression,
including sedation and amnesia, are prominent after scopolamine. Physostigmine,
a cholinesterase inhibi-tor that crosses the blood–brain barrier, promptly
reverses anticholinergic actions on the brain.
D. Gastrointestinal
Salivary secretions are markedly reduced
by anticho-linergic drugs. Gastric secretions are also decreased, but larger
doses are necessary. Decreased intesti-nal motility and peristalsis prolong
gastric empty-ing time. Lower esophageal sphincter pressure is reduced.
Overall, the anticholinergic drugs do not prevent aspiration pneumonia.
E. Ophthalmic
Anticholinergics cause mydriasis
(pupillary dila-tion) and cycloplegia (an inability to accommodate to near
vision); acute angle-closure glaucoma is unlikely following systemic
administration of most anticholinergic drugs.
F. Genitourinary
Anticholinergics may decrease ureter and
bladder tone as a result of smooth muscle relaxation and lead to urinary
retention, particularly in elderly men with prostatic hypertrophy.
G. Thermoregulation
Inhibition of sweat glands may lead to a
rise in body temperature (atropine fever).
Related Topics