Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Genitourinary Surgery
Anesthesia for Transurethral Resection of the Prostate
TRANSURETHRAL RESECTION OF THE PROSTATE
Preoperative Considerations
Benign prostatic hyperplasia (BPH) frequently leads to bladder
outlet obstruction in men older than 60 years. Although increasingly being
treated medically, some men require surgical intervention. Transurethral
resection of the prostate (TURP) is the most common surgical procedure
performed for bladder outlet obstruction due to BPH, and indica-tions for TURP in
this setting include obstructive uropathy, bladder calculi, and recurrent
episodes of urinary retention, urinary tract infections, and hematuria.
Patients with adenocarcinoma of the prostate may also benefit from TURP to
relieve symptomatic urinary obstruction.
TURP requires regional or general
anesthe-sia, and patients should be evaluated for coexistent major organ
dysfunction. Despite advanced age (over half of TURP patients are older than 70
years) and prevalence of significant comorbidity in over two thirds of TURP
patients, perioperative mortality and medical morbidity (most frequently
myocardial infarction, pulmonary edema, and kidney failure) for this procedure
are both less than 1%.
The most common surgical complications
of TURP are clot retention, failure to void, uncontrolled hematuria requiring
surgical revision, urinary tract infection, and chronic hematuria, although
other, more rare, complications may include: TURP syn-drome, bladder
perforation, sepsis, hypothermia, and disseminated intravascular coagulation
(DIC). A blood type and screen is
ade-quate for most patients, although crossmatched blood should be available
for anemic patients and for patients with large glands in which extensive
resection is contemplated. Prostatic bleeding can be difficult to control
through the cystoscope.
Intraoperative Considerations
TURP is performed by passing a loop
through a special cystoscope (resectoscope). Using continuous irrigation and
direct visualization, prostatic tissue is resected by applying a cutting
current to the loop. Because of the characteristics of the prostate and the
large amounts of irrigation fluid often used, TURP
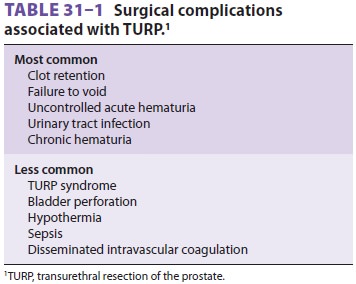
can be associated with a number of serious compli-cations ( Table 31–1).
A. TURP Syndrome
Transurethral
prostatic resection often opens the extensive network of venous sinuses in the
prostate, potentially allowing systemic absorption of the irrigating fluid. The
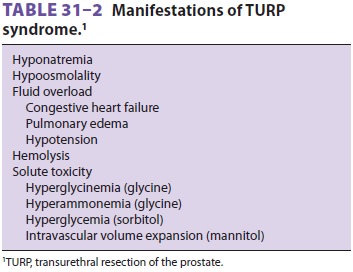
absorption of large amounts of fluid (2 L or more) results in a constellation
of symptoms and signs commonly referred to as the TURP syndrome (Table 31–2).
This syndrome pres-ents intraoperatively or postoperatively as headache,
restlessness, confusion, cyanosis, dyspnea, arrhyth-mias, hypotension, or
seizures, and it can be rapidly
fatal.
The manifestations are primarily those of circulatory fluid overload, water
intoxication,and, occasionally, toxicity from the solute in the irri-gating
fluid. The incidence of TURP syndrome is less than 1%.Electrolyte solutions
cannot be used for irriga-tion during TURP because they disperse the
electro-cautery current. Water provides excellent visibility because its
hypotonicity lyses red blood cells, but significant water absorption can
readily result in acute water intoxication. Water irrigation is gener-ally
restricted to transurethral resection of bladder tumors only. For TURP,
slightly hypotonic nonelec-trolyte irrigating solutions such as glycine 1.5%
(230 mOsm/L) or a mixture of sorbitol 2.7% and mannitol 0.54% (195 mOsm/L) are
most commonly used. Less commonly used solutions include sorbitol 3.3%,
mannitol 3%, dextrose 2.5–4%, and urea 1%.
Because all these
fluids are still hypotonic, signifi-cant absorption of water can nevertheless
occur. Solute absorption can also occur because the irriga-tion fluid is under
pressure, and high irrigation pres-sures (bottle height) increase fluid
absorption.
Absorption
of TURP irrigation fluid is depen-dent on the duration of the resection and
thepressure of the irrigation fluid. Most resections last 45–60 min, and, on
average, 20 mL/min of the irri-gating fluid is absorbed. Pulmonary congestion
or florid pulmonary edema can readily result from the absorption of large
amounts of irrigation fluid, particularly in patients with limited cardiac
reserve. The hypotonicity of these fluids also results in acute hyponatremia
and hypoosmolality, which can lead to serious neurological manifestations.
Symptoms of hyponatremia usually do not develop until the serum sodium concentration
decreases below 120 mEq/L. Marked hypotonicity in plasma ([Na +]
<100
mEq/L) may also result in acute intravascular hemolysis.
Toxicity may also
arise from absorption of the solutes in these fluids. Marked hyperglycinemia has been reported
with glycine solutions and may con-tribute to circulatory depression and central
nervous system toxicity. Plasma glycine concentrations in excess of 1000 mg/L
have been recorded (normal is 13–17 mg/L). Glycine is known to be an inhibitory
neurotransmitter in the central nervous system and has also been implicated in
rare instances of tran-sient blindness following TURP. Hyperammonemia,
presumably from the degradation of glycine, has also been documented in a few patients
with marked central nervous system toxicity following TURP. Blood ammonia
levels in some patients exceeded 500 µmol/L (normal is 5–50 µmol/L). The use of
large amounts of sorbitol or dextrose irrigating solutions can lead to
hyperglycemia, which can be marked in diabetic patients. Absorption of
manni-tol solutions causes intravascular volume expansion and exacerbates fluid
overload.
Treatment
of TURP syndrome depends on early recognition and should be based on the
severity of the symptoms. The absorbed water must be elimi-nated, and hypoxemia
and hypoperfusion treated. Most patients can be managed with fluid restric-tion
and intravenous administration of furosemide. Symptomatic hyponatremia
resulting in seizures or coma should be treated with hypertonic saline .
Seizure activity can be terminated with small doses of midazolam (2–4 mg).
Phenytoin, 10–20 mg/kg intravenously (no faster than 50 mg/ min), should also
be considered to provide more sustained anticonvulsant activity. Endotracheal
intu-bation may be considered to prevent aspiration until the patient’s mental
status normalizes. The amount and rate of hypertonic saline solution (3% or 5%)
needed to correct the hyponatremia to a safe level should be based on the
patient’s serum sodium con-centration . The rate of hypertonic saline solution
administration should be sufficiently slow as to not exacerbate circulatory fluid
overload.
B. Hypothermia
Large volumes of irrigating fluids at room tempera-ture can be a
major source of heat loss in patients. Irrigating solutions should be warmed to
body temperature prior to use to prevent hypothermia. Postoperative shivering
associated with hypother-mia may dislodge clots and promote postoperative
bleeding, as well as add deleterious physiological stress to the patient with
coexisting cardiopulmo-nary disease.
C. Bladder Perforation
The incidence of bladder perforation
during TURP is less than 1%. Perforation may result from the resectoscope going
through the bladder wall or from overdistention of the bladder with irrigation
fluid. Most bladder perforations are extraperitoneal and are signaled by poor
return of the irrigating fluid. Awake patients will typically complain of
nausea, diaphoresis, and retropubic or lower abdominal pain. Large
extraperitoneal and most intraperitoneal perforations are usually even more
obvious, present-ing as sudden unexplained hypotension or hyperten-sion, and
with generalized abdominal pain in awake patients. Regardless of the anesthetic
technique employed, perforation should be suspected in set-tings of sudden
hypotension or hypertension, par-ticularly with acute, vagally mediated
bradycardia.
D. Coagulopathy
DIC has on rare occasion been reported
following TURP and may result from the release of throm-boplastins from
prostate tissue into the circulation during the procedure. Up to 6% of patients
may have evidence of subclinical DIC. A dilutional thrombo-cytopenia can also
develop during surgery as part of the TURP syndrome from absorption of
irriga-tion fluids. Rarely, patients with metastatic carci-noma of the prostate
develop a coagulopathy from primary fibrinolysis due to secretion of a
fibrino-lytic enzyme. The diagnosis of coagulopathy may be suspected from
diffuse, uncontrollable bleeding but must be confirmed by laboratory tests.
Primary fibrinolysis should be treated with ε-aminocaproic acid (Amicar), 5 g
followed by 1 g/h intravenously. Treatment of DIC in this setting may require
hepa-rin in addition to replacement of clotting factors and platelets, and
consultation with a hematologist should be considered.
E. Septicemia
The prostate is often colonized with
bacteria and may harbor chronic infection. Extensive surgical resec-tion with
the opening of venous sinuses can allow entry of organisms into the
bloodstream. Bacteremia following transurethral surgery is common and can lead
to septicemia or septic shock. Prophylactic anti-biotic therapy (most commonly
gentamicin, levo-floxacin, or cefazolin) prior to TURP may decrease the
likelihood of bacteremic and septic episodes.
F. Choice of Anesthesia
Either spinal or epidural anesthesia
with a T10 sen-sory level, or general anesthesia, provides excellentanesthesia
and good operating conditions for TURP. When compared with general anesthesia,
regional anesthesia may reduce the incidenceof postoperative venous thrombosis.
It is also less likely to mask symptoms and signs of TURP syn-drome or bladder
perforation. Clinical studies have failed to show any differences in blood
loss, postop-erative cognitive function, and mortality between regional and
general anesthesia. The possibility of vertebral metastasis must be considered
in patients with carcinoma, particularly those with back pain, as metastatic
disease involving the lumbar spine is a relative contraindication to spinal or
epidural anes-thesia. Acute hyponatremia from TURP syndrome may delay or
prevent emergence from general anesthesia.
G. Monitoring
Evaluation of mental status in the awake
or moder-ately sedated patient is the best monitor for detec-tion of early
signs of TURP syndrome and bladder perforation. Tachycardia or decrease in
arterial oxy-gen saturation may be an early sign of fluid over-load.
Perioperative ischemic electrocardiographic changes have been reported in up to
18% of patients. Temperature monitoring is standard of care for gen-eral
anesthesia, and it should also be used in cases of lengthy resections under
spinal or epidural anes-thesia to detect hypothermia. Blood loss is
particu-larly difficult to assess during TURP because of the use of irrigating
solutions, so it is necessary to rely on clinical signs of hypovolemia . Blood
loss averages approximately 3–5 mL/min of resection (usually 200–300 mL total)
but is rarely life-threatening. Transient, postoperative decreases in
hematocrit may simply reflect hemodilution from absorption of irrigation fluid.
Less than 2% of patients require intraoperative blood transfusion; factors associated
with need for transfusion include procedure duration longer than 90 min and
resec-tion of more than 45 g of prostate tissue.
Related Topics