Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Orthopedic Surgery
Anesthesia for Total Hip Arthroplasty
TOTAL HIP ARTHROPLASTY
Preoperative Considerations
Most patients undergoing total hip
replacement suffer from osteoarthritis (degenerative joint dis-ease),
autoimmune conditions such as rheumatoid arthritis (RA), or avascular necrosis.
Osteoarthritis is a degenerative disease affecting the articular sur-face of
one or more joints (most commonly the hips and knees). The etiology of
osteoarthritis appears to involve repetitive joint trauma. Because
osteoarthri-tis may also involve the spine, neck manipulation during tracheal
intubation should be minimized to avoid nerve root compression or disc
protrusion.
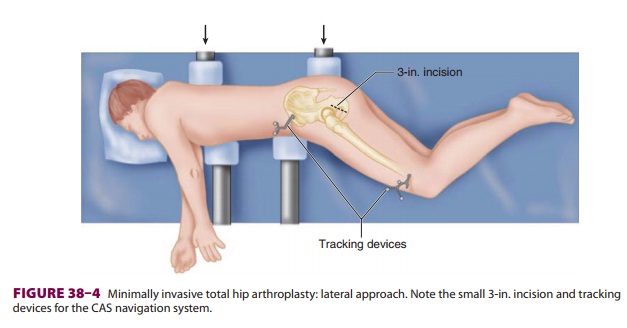
RA is characterized by immune-mediated joint destruction with chronic
and progressive inflam-mation of synovial membranes, as opposed to the
articular wear and tear of osteoarthritis. RA is a systemic disease affecting
multiple organ systems (Table 38–1). RA often affects the small
joints of the hands, wrists, and feet causing severe deformity; when this
occurs, intravenous and radial artery can-nulation can be challenging.
Extreme cases of RA involve almost all
synovial membranes, including those in the cervical spine and temporomandibular
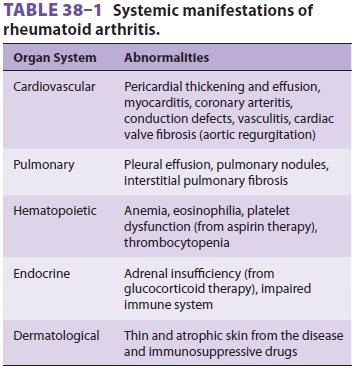
joint. Atlantoaxial subluxation, which can be diagnosed radiologically, may
lead to protrusion of the odontoid process into the foramen magnum during
intubation, compromising vertebral blood flow and compressing the spinal cord
or brainstem (Figure 38–3). Flexion and extension lat-eral
radiographs of the cervical spine should beobtained preoperatively in patients
with RA severe enough to require steroids, immune therapy, or methotrexate. If
atlantoaxial instability is present, tracheal intubation should be performed
with inline stabilization utilizing video or fiberoptic laryngos-copy.
Involvement of the temporomandibular joint can limit jaw mobility and range of
motion to such a degree that conventional orotracheal intubation may be
impossible. Hoarseness or inspiratory stridor may signal a narrowing of the
glottic opening caused by cricoarytenoid arthritis. This condition may lead to
postextubation airway obstruction even when a smaller diameter tracheal tube
has been used.
Patients with RA or osteoarthritis commonly receive nonsteroidal
antiinflammatory drugs (NSAIDs) for pain management. These drugs can have
serious side effects such as gastrointestinal bleeding, renal toxicity, and
platelet dysfunction.
Intraoperative Management
Total hip replacement (THR) involves several
surgi-cal steps, including positioning of the patient (usu-ally in the lateral
decubitus position), dislocation and removal of the femoral head, reaming of
the acetabulum and insertion of a prosthetic acetabular cup (with or without
cement), and reaming of the femur and insertion of a femoral component
(femo-ral head and stem) into the femoral shaft (with or without cement). THR
is also associated with three potentially life-threatening complications: bone
cement implantation syndrome, intra- and postop-erative hemorrhage, and venous
thromboembolism. Thus, invasive arterial monitoring may be justified for select
patients undergoing these procedures. Neuraxial administration of opioids such
as mor-phine in the perioperative period extends the dura-tion of postoperative
analgesia.
A. Hip Resurfacing Arthroplasty
The increasing number of younger patients presenting for hip arthroplasty and of other patients who require revision of standard (metal-on-polyethylene) total hip arthroplasty implants has led to redevelopment of hip resurfacing arthroplasty techniques. Compared with traditional hip arthroplasty implants, hip resur-facing maintains patients’ native bone to a greater degree. Metal-on-metal hybrid implants are usually employed. Surgical approaches can be anterolateral or posterior, with the posterior approach theoreti-cally providing greater preservation of the blood sup-ply to the femoral head. With the posterior approach, patients are placed in the lateral decubitus position similar to traditional hip arthroplasty.
Outcomes data related to hip resurfacing
versus traditional total hip arthroplasty are controversial. Prospective
studies have not shown a difference in gait or postural balance at 3 months
postoperatively. A recent meta-analysis favored resurfacing in terms of
functional outcome and blood loss despite com-parable results for postoperative
pain scores and patient satisfaction. Of particular concern is the finding that
patients who undergo resurfacing are nearly twice as likely to require revision
surgery as those receiving traditional hip arthroplasty. There is a higher
incidence of aseptic component loosening (possibly from metal hypersensitivity)
and femo-ral neck fracture, particularly in women. Finally, the presence of
metal debris in the joint space (from metal-on-metal contact) has led to a
marked narrowing of indications for the prostheses and the procedure.
B. Bilateral Arthroplasty
Bilateral hip arthroplasty can be safely
performed in fit patients as a combined procedure, assuming the absence of
significant pulmonary embolization after insertion of the first femoral
component. Monitoringmay include echocardiography. Effective com-munication between the anesthesia provider and surgeon is
essential. If major hemodynamic instability occurs during the first hip
replacement procedure, the second arthroplasty should be postponed.
C. Revision Arthroplasty
Revision of a prior hip arthroplasty may be
associated with much greater blood loss than in the initial pro-cedure. Blood
loss depends on many factors, includ-ing the experience and skill of the
surgeon. Some studies suggest that blood loss may be decreased during hip
surgery if a regional anesthesia technique is used (eg, spinal or epidural
anesthesia) compared with general anesthesia even at similar mean arte-rial
blood pressures. The mechanism is unclear. Because the likelihood of
perioperative blood trans-fusion is high, preoperative autologous blood
dona-tion and intraoperative blood salvage should be considered. Preoperative
administration of vitamins (B12 and K) and iron can treat mild forms of chronic anemia. Alternatively
(and more expensively), recombinant human erythropoietin (600 IU/kg
subcutaneously weekly beginning 21 days before surgery and ending on the day of
surgery) may also decrease the need for perioperative allogeneic blood
transfusion. Erythropoietin increases red blood cell production by stimulating
the division and differen-tiation of erythroid progenitors in the bone marrow.
Maintaining normal body temperature during hip replacement surgery reduces
blood loss.
D. Minimally Invasive Arthroplasty
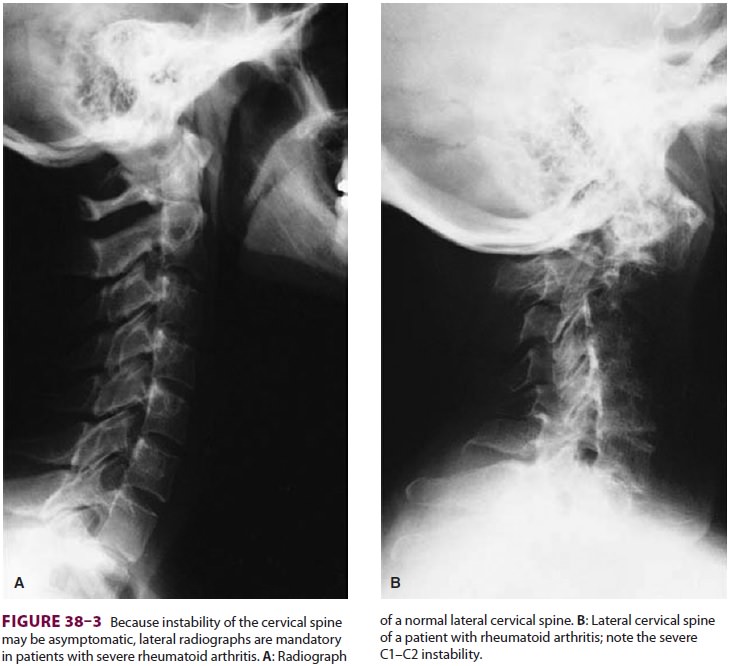
Computer-assisted surgery (CAS) may improve
surgical outcomes and promote early rehabilitation through minimally invasive
techniques employ-ing cementless implants. Computer software can accurately
reconstruct three-dimensional images of bone and soft tissue based on
radiographs, fluo-roscopy, computed tomography, or magnetic reso-nance imaging.
The computer matches preoperative images or planning information to the
position of the patient on the operating room table. Tracking devices are
attached to target bones (Figure 38–4)
and instruments used during surgery, and the navi-gation system utilizes
optical cameras and infrared light-emitting diodes to sense their positions.
CAS thus allows accurate placement of implants through
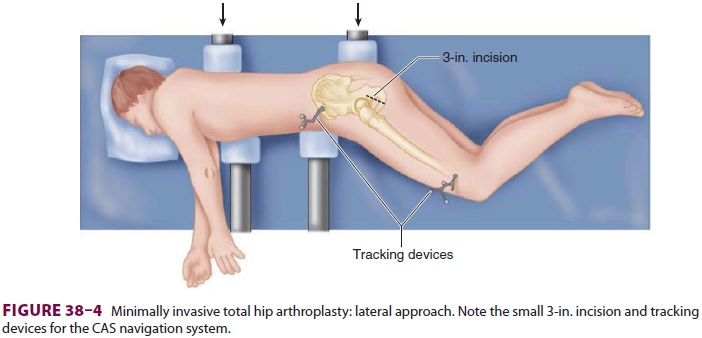
small incisions, and the resulting reduction
in tissue and muscle damage could lead to less pain and early rehabilitation.
The lateral approach utilizes a single 3-in. incision with the patient in the
lateral decubitus position (Figure 38–4); an anterior approach utilizes two
separate 2-in. incisions (one for the acetabular component and another for the
femoral compo-nent) with the patient supine. Minimally invasive techniques can
reduce hospitalization to 24 h or less. Anesthetic techniques should promote
rapid recov-ery and can include neuraxial regional anesthesia or total
intravenous general anesthesia.
E. Hip Arthroscopy
In recent years, hip arthroscopy has increased in popularity as a
minimally invasive alternative to open arthrotomy for a variety of surgical
indications such as femoroacetabular impingement (FAI), ace-tabular labral
tears, loose bodies, and osteoarthritis. At present, there is fair evidence in
the published lit-erature (small, randomized controlled trials) to sup-port hip
arthroscopy for FAI, but evidence is lacking for other indications.
Related Topics