Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Neurologic & Psychiatric Diseases
Anesthesia for Substance Abuse
SUBSTANCE ABUSE
Behavioral disorders from abuse of
psychotropic (mind-altering) substances may involve a socially acceptable drug
(alcohol), a medically prescribed drug (eg, diazepam), or an illegal substance
(eg, cocaine). Characteristically, with chronic abuse, patients develop
tolerance to the drug and varying degrees of psychological and physical
dependence. Physical dependence is most often seen with opioids, barbiturates,
alcohol, and benzodiazepines. Life-threatening complications primarily due to
sympa-thetic overactivity can develop during abstention.
Knowledge of a patient’s substance abuse pre-operatively may
prevent adverse drug interactions, predict tolerance to anesthetic agents, and
facilitate the recognition of drug withdrawal. The history of substance abuse
may be volunteered by the patient (usually only on direct questioning) or
deliberately hidden.
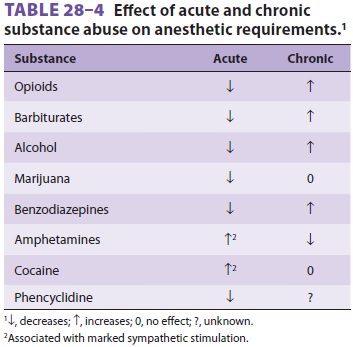
Anesthetic requirements for substance
abusers vary, depending on whether the drug exposure is acute or chronic (see Table28–4).
Elective proce-dures should be postponed for acutely intoxicated patients and
those with signs of withdrawal. When surgery is deemed necessary in patients
with physical dependence, perioperative doses of the abused sub-stance should
be provided, or specific agents should be given to prevent withdrawal. In the
case of opioid dependence, any opioid can be used, whereas for alcohol, a
benzodiazepine is usually substituted due to the reluctance of hospital
pharmacies to dispense
alcohol-containing beverages to
patients. Alcoholic patients should receive B vitamin/folate supplemen-tation
to prevent Korsakoff ’s syndrome. Tolerance to most anesthetic agents is often
seen, but is not always predictable. For general anesthesia, a technique
pri-marily relying on a volatile inhalation agent may be preferable so that
anesthetic depth can be readily adjusted according to individual need.
Awareness monitoring should be likewise considered. Opioids with mixed
agonist–antagonist activity should be avoided in opioid-dependent patients
because such agents can precipitate acute withdrawal. Clonidine is a useful
adjuvant in the treatment of postoperative withdrawal syndromes.
Patients routinely present acutely
intoxicated for emergency surgery following trauma related to sub-stance abuse.
Patients have often consumed more than one class of intoxicating agent. Acute
cocaine intoxi-cation may produce hypertension secondary to the increase in
central neurotransmitters, such as norepi-nephrine and dopamine. Hypertension
and arrhyth-mias can occur perioperatively. Chronic abusers deplete their
sympathomimetic neurotransmitters, potentially developing hypotension.
Amphetamine abusers have similar anesthetic concerns, as amphet-amines also
affect the sympathetic nervous system. Patients on chronic prescribed opioid
therapy, or those taking medications illicitly, have substantiallyincreased
opioid postoperative requirements. Multimodal approaches to pain control are
useful perioperatively, and patients should be started on maintenance methadone
as soon as possible.Consultation with pain management and addic-tion
specialists is often indicated.
Related Topics