Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Neurologic & Psychiatric Diseases
Anesthesia for Seizure Disorders
Seizure Disorders
Preoperative Considerations
Seizures represent abnormal synchronized
electrical activity in the brain. They may be a manifestation of an underlying
central nervous system disease, a systemic disorder, or idiopathic. Potential
underly-ing mechanisms are thought to include (1) loss of inhibitory activity,
(2) enhanced release of excitatory amino acids, and (3) enhanced neuronal
firing due to abnormal voltage-mediated Ca 2+ currents. Up to 2% of the population may experience
a seizure in their lifetime. Epilepsy is a disorder characterized by recurrent
paroxysmal seizure activity. Healthy indi-viduals who experience an isolated
nonrecurrent seizure are not considered to have epilepsy.Seizure activity may
be localized to a specific area in the brain or may be generalized. Moreover,
initially localized (focal) seizures can subsequently spread, becoming
generalized. A simple classifi-cation scheme is presented in Table28–2. Partial
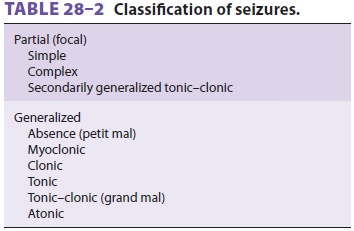
seizures (also called focal) are
clinically manifested by motor, sensory, autonomic, or psychiatric symp-toms,
depending on the cortical area affected. Focal seizures associated with
impairment in conscious-ness are termed “complex partial” (psychomotor or
temporal lobe) seizures. Generalized seizures char-acteristically produce
bilaterally symmetric electri-cal activity without local onset. They result
with or without abnormal motor activity, loss of con-sciousness, or both.
Generalized activity resulting in isolated, transient lapses in consciousness
are called absence (petit mal) seizures. Other general-ized seizures are
usually classified according to the type of motor activity. Tonic–clonic (grand
mal) seizures are most common and are characterized by a loss of consciousness
followed by clonic and then tonic motor activity.
PREOPERATIVE MANAGEMENT
Anesthetic evaluation should focus primarily on the underlying
disorder and secondarily on the seizures. One should determine the cause and
type of seizure activity and the drugs with which the patient is being treated.
Seizures in adults are most commonly due to structural brain lesions (head
trauma, tumor, degeneration, or stroke) or metabolic abnormalities (uremia,
hepatic fail-ure, hypoglycemia, hypocalcemia, drug toxicity, or drug/alcohol
withdrawal). Idiopathic seizures occur most often in children, but may persist
into adulthood. Characterization of the type of seizure is important in
detecting such activity
perioperatively. Seizures—particularly grand mal seizures—are
serious complicating factors in sur-gical patients and should be treated
promptly to prevent musculoskeletal injury, hypoventilation, hypoxemia, and
aspiration of gastrointestinal con-tent. Even partial seizures can progress to
grand mal seizures. If a seizure occurs, maintaining an open airway and
adequate oxygenation are the first priorities. Intravenous propofol (50–100
mg), phenytoin (500–1000 mg slowly), or a benzodiaz-epine such as diazepam
(5–10 mg) or midazolam (1–5 mg) can be used to terminate the seizure. Most
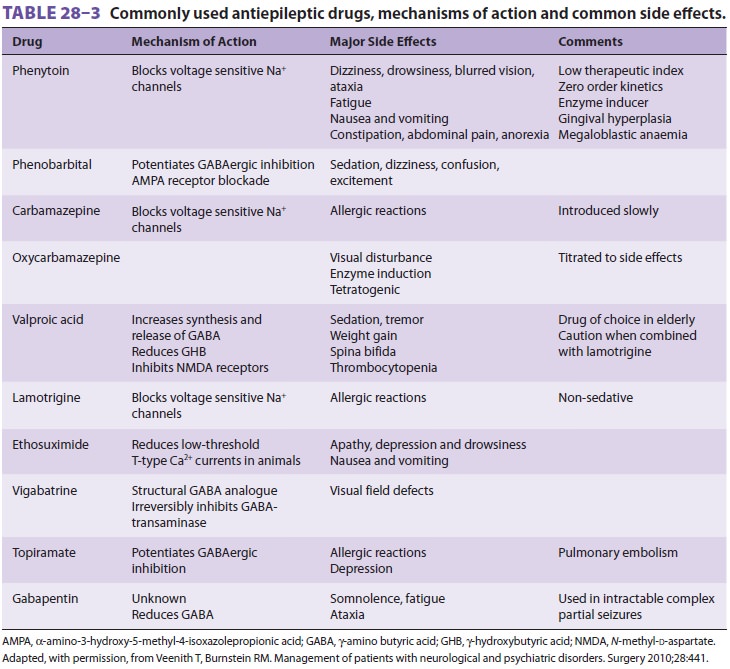
patients with seizure disorders receive antiepileptic drugs preoperatively ( Table28–3).
Antiseizure medications should be continued throughout the perioperative period
to maintain therapeutic levels.
INTRAOPERATIVE MANAGEMENT
In selecting anesthetic agents, drugs
with epilepto-genic potential should be avoided, most notably the general
anesthetic enflurane (now of only historicinterest). Theoretically, ketamine
and methohexi-tal (in small doses) can precipitate seizure activity.
Hypothetically, large doses of atracurium, cisatracu-rium, or meperidine may be
relatively contraindi-cated because of the reported epileptogenic potential of
their respective metabolites, laudanosine, and normeperidine. Hepatic
microsomal enzyme induc-tion should be expected from chronic antiseizure
therapy. Enzyme induction may increase the dose requirement and frequency of
intravenous anesthet-ics and nondepolarizing neuromuscular blockers (NMBs) and
may increase the risk for hepatotoxicity from halothane.
Related Topics